In cases of central nervous system infection, it is crucial for the neuroradiologist to provide an accurate differential diagnosis of the possible pathogens involved so that treating physicians can be aided in the choice of empiric therapy. This approach requires the radiologist to be aware of local epidemiology and have knowledge of infectious agents that are endemic to their area of practice. This article reviews and discusses the changing epidemiology of pathogens most often observed in meningitis, brain abscess, epidural abscess, postoperative infections, and human immunodeficiency virus infection.
- •
The rapid recognition and diagnosis of central nervous system (CNS) infection is critical to achieving a favorable clinical outcome.
- •
Pathogens vary based on the location of infection within the CNS, geographic exposures, vaccination status, age, surgical intervention, and immune suppression.
- •
Knowledge of the organisms that are most commonly present in various types of CNS infection is important in the selection of appropriate empiric antimicrobial therapy.
- •
Treatment of most CNS infections should be initiated promptly with the guidance of an infectious diseases specialist.
Introduction
Central nervous system (CNS) infections remain an important cause of morbidity and mortality worldwide. In 2004, globally there were 340,000 deaths estimated by the World Health Organization to be related to meningitis, with an incidence of 700,000. In the Americas there were approximately 13,000 deaths attributed to meningitis, which disproportionately affects those of low and middle income 12:1 when compared with individuals with high income. There are many infectious pathogens known to cause CNS infection, including the broad categories of bacteria, viruses, fungi, mycobacteria, and parasites. In most cases, it is impossible for the radiologist with certainty to identify a specific organism as the cause of an observed radiographic abnormality in the CNS. However, the geography, exposures, season, and clinical information supplied in the medical record can significantly aid in developing a more specific differential diagnosis. This review discusses the epidemiology and typical pathogens associated with infection of the CNS including meningitis, brain abscess, epidural abscess, and postoperative complications of neurologic surgery, as well as human immunodeficiency virus HIV/AIDS.
Meningitis
Bacteria
When bacteria infect the CNS, in most cases an acute syndrome of headache, fever, nuchal rigidity, and change of mental status occurs. Meningitis caused by bacteria continues to be a significant clinical syndrome that requires rapid recognition and treatment by clinicians to prevent associated life-threatening complications. With the introduction of vaccination for certain pathogens, the epidemiology of bacterial meningitis has changed dramatically over the past 2 decades.
The number of cases of meningitis caused by Haemophilus influenzae type B decreased by 94% after 1988 when the vaccine was introduced to a rate of 0.2 cases per 100,000. Unvaccinated adults with nontypable H influenzae now make up the majority of cases. Meningitis caused by Streptococcus pneumoniae has decreased 30%, from 1.1 cases per 100,000 in the late 1990s to 0.79 per 100,000 in the period 2004 to 2005. This decrease occurred after the introduction of the 7-valent conjugate pneumococcal vaccine for children, which was licensed in 2000. This decrease in incidence has extended to not only children but also adults, presumably secondary to herd immunity. However, other pneumococcal serotypes not covered in the vaccine are now being seen with increased frequency in certain locations. Mortality rates attributable to pneumococcal meningitis have remained the same at around 21% for adults and 8% for children. Other pathogens such as Neisseria meningitidis (0.6/100,000), Group B streptococcus (0.3/100,000), and Listeria monocytogenes (0.2/100,000) occur less frequently.
The patient’s age and immune status affects the organism most likely to be present in bacterial meningitis ( Table 1 ). While pneumococcus remains the most common in all age groups, organisms such as Listeria are more likely to be observed in older and immune-compromised patients. Group B streptococcus and gram-negative organisms such as Escherichia coli are most common in neonates who develop meningitis related to exposure to urogenital flora at the time of birth. Outbreaks of meningococcal meningitis occur under conditions of crowding. Clusters of cases have been reported on college campuses and with religious gatherings such as the Hajj. For the Hajj, vaccination programs have been initiated such that visitors are required to have received the quadrivalent meningococcal vaccine, which has decreased the incidence of invasive infection substantially. However, pilgrims often can still become colonized with N meningitidis and can therefore transmit the organism to household contacts on their return home, which has led to outbreaks in several European countries. In 2000 there were 25 cases per 100,000 pilgrims to the Hajj from Singapore. In addition, there was a subsequent attack rate of 18 cases per 100,000 in household contacts who were exposed to returning pilgrims. Therefore, there are now recommendations for household contacts of at-risk travelers to also receive the meningococcal vaccine.
| Pathogen | Risk Factor | Incidence |
|---|---|---|
| Streptococcus pneumoniae | Day care, HIV infection | Most common |
| Neisseria meningitidis | Crowded conditions | Outbreaks |
| Haemophilus influenzae | Significantly less common after vaccination | |
| Listeria monocytogenes | Immune compromise, elderly | Less common |
| Group B streptococcus | Neonates | Decreased with antenatal detection of group B streptococcus |
| Escherichia coli | Neonates | Less common |
| Mycobacterium tuberculosis | Exposure, older age, immune compromise | Rare |
The performance of a lumbar puncture is the first step in the evaluation of any patient suspected of meningitis or encephalitis. Imaging of the brain is often indicated in patients with neurologic deficits, immune-compromising conditions, or decreased level of consciousness. In one study, 45% of patients with bacterial meningitis met criteria for CNS imaging. If a mass lesion is present, there is risk for brain herniation at the time of cerebrospinal fluid (CSF) withdrawal.
Viruses
CNS infections caused by viruses are often referred to as aseptic meningitis because traditional bacterial cultures from the CSF are negative. Patients tend to present in a subacute fashion with headache and fever. There are many viruses that can cause aseptic meningitis ( Table 2 ). A study performed in Finland analyzing consecutive adult patients with aseptic meningitis found that 26% of cases were related to enteroviruses, 17% to herpes simplex virus (HSV)-2, and 8% related to varicella zoster virus (VZV). Of patients with encephalitis, VZV was found in 12% of cases and HSV-1 in 9%, with tick-borne viruses identified in 9%. In 44% of patients, a specific cause was not confirmed. Because viral culture is difficult and insensitive, molecular testing via the polymerase chain reaction (PCR) from CSF has greatly aided in the diagnosis of meningitis caused by viruses. With these techniques it has been shown that more than 90% of cases of aseptic meningitis are caused by enteroviruses in other studies. Enterovirus infection typically occurs in the summer to fall months and is most common in children, although it is also the most common cause of aseptic meningitis in adults. Outbreaks have been identified in various locations globally, including a large outbreak described in Taiwan in patients who also had associated hand-foot-and-mouth disease.
| Pathogen | Risk Factor | Incidence |
|---|---|---|
| Enteroviruses | Warm weather | Most common |
| Herpes simplex virus | Presence of latent virus | Common |
| Varicella zoster virus | Presence of latent virus, immune compromise | Occasional |
| West Nile virus | Mosquito borne | Outbreaks, declining in USA |
| La Crosse virus | Mosquito borne | Rare |
| Dengue | Mosquito borne | Regional outbreaks |
| Human herpesvirus 6 | Immune compromise | Rare |
| Lymphocytic choriomeningitis | Exposure to contaminated rodent excreta | Rare |
| Powassan virus | Regional tick exposure | Very rare |
| Chikungunya virus | Regional mosquito exposure | Regional outbreaks |
| Rabies | Exposure to infected animals | Rare |
| Japanese encephalitis | Summer, Southeast Asia | Regional |
| Mumps | Setting of outbreak | Very rare |
| HIV | Unprotected sexual exposure | Rare |
| Adenovirus | Outbreaks | Rare |
| Influenza | Seasonal epidemics | Rare |
Viral CNS infections often also can cause encephalitis. This situation occurs when there is infection of the brain parenchyma with associated inflammation, which is accompanied by changes in mental status and behavior, and sometimes reduced level of consciousness. Overall, it is estimated that there are 10.5 to 13.8 per 100,000 hospitalizations for children and 2.2 per 100,000 hospitalizations for adults for acute encephalitis syndrome. In one review, from 1950 to 1981 in Minnesota, there were 7.4 per 100,000 hospitalizations for encephalitis, with a specific virus identified in 25% of the cases. Early in the study period mumps and arboviruses were most common. The epidemiology of viral meningitis and encephalitis has been significantly altered by vaccination. In the 1940s and 1950s, mumps virus was encountered as a cause of viral meningitis in 15% of cases. Occasional outbreaks of mumps still occur; however, meningitis caused by this virus is now rare. In the Minnesota study, no cases of mumps-related encephalitis occurred after 1972.
Viruses transmitted by arthropod vectors that cause encephalitis and meningitis have become more common in recent years. During the summer of 1999, West Nile virus was recognized as having caused a widespread epidemic that began in New York City and eventually spread across the United States along bird-migratory routes. In 2002 there were 2942 cases of neuroinvasive West Nile disease, which represented 71% of the cases of viral meningoencephalitis reported. The incidence of West Nile–associated meningitis peaked in the late summer months during the years of increased incidence. As immunity has developed and the susceptible reservoir of bird populations has decreased, the incidence of West Nile encephalitis has decreased substantially in recent years. In 2009 there were only 373 cases of encephalitis or meningitis reported.
There are a variety of other arthropod-transmitted viruses that can cause meningitis and that have certain geographic distributions. St. Louis encephalitis, La Crosse virus, and Eastern Equine encephalitis are endemic within the United States and are observed to cause disease sporadically, from 0.01 to 0.04 cases per 100,000. Dengue is caused by a group of 4 viruses transmitted by mosquitoes and is a common cause of viral meningitis in tropical areas, particularly in South and Central America. The World Health Organization estimates that 50 million people are infected by dengue yearly. In the Americas in 2007 there were 890,000 cases reported, with 26,000 cases complicated by dengue hemorrhagic fever. In recent history dengue has not been endemic in the United States; however, in 2009 28 cases of dengue were identified in individuals who either traveled to or lived in Key West, Florida. Thus, as with West Nile virus, emerging pathogens are able to become endemic in new geographic locations including the United States.
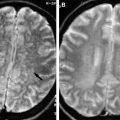
Reactivation or new infection with herpes viruses can also lead to infection in the CNS. The diagnosis of these infections has also been transformed by the ability to apply molecular techniques such as the PCR, although occasional false-negative results may be obtained. HSV-2 most commonly causes meningitis and can be associated with primary infection while HSV-1 can cause necrotizing encephalitis with significant neurologic sequelae. In a study performed in Sweden, there were 2.2 cases per million population of HSV-1–related encephalitis per year. Attributable mortality was 14%, with 21% of surviving patients having developed a seizure disorder as sequelae. HSV-1 has also been linked to a recurrent, benign lymphocytic meningitis known as Mollaret meningitis, which is considered to be rare. In this syndrome patients present with recurrent aseptic meningitis in which HSV-1 DNA has been found in some patients. In immune-compromised patients with solid organ transplantation or stem cell transplantation, human herpesvirus 6 (HHV-6) can cause meningitis or encephalitis when latent virus reactivates. Similarly, VZV can cause meningitis or encephalitis in immune-compromised patients when reactivation occurs in the setting of zoster or disseminated disease in those who are susceptible to primary infection.
Other less commonly encountered viruses are listed in Table 2 and include lymphocytic choriomeningitis virus, which can occur after exposure to contaminated rodent excreta. HIV infection can cause an aseptic meningitis–type syndrome at the time of acute infection and should be considered in patients with risk factors such as recent high-risk sexual contact. Neurologic disorders including aseptic meningitis have been described in up to 12% of patients who develop the acute retroviral syndrome associated with the acquisition of HIV infection. The clinician also must be aware of outbreaks that are occurring in various geographic areas to which patients may have traveled or where they reside. Powassan virus is transmitted by ticks and can cause encephalitis. This rare virus has been found to cause disease mostly in Maine, Vermont, and New York, where 7 cases were reported between 1999 and 2005. In an outbreak of Chikungunya virus on La Reunion Island from 2005 to 2006, out of 274 patients evaluated 70% had symptoms of headache. CNS symptoms have been reported rarely, but CNS pleocytosis has not been observed with this infection. Meningitis has rarely been reported as a complication of influenza. A large study conducted in Great Britain identified only 0.01% (21) of more than 141,000 patients with influenza-like illness who had developed this complication.
Infection with the rabies virus leads to severe encephalitis and carries a very high mortality rate. The incidence of human infection with rabies has declined substantially in the United States, from 33 cases in 1946 to 3 cases in 2006. Most cases of rabies occur after exposure to infected wild animals such as bats, skunks, raccoons, or foxes. In other locations globally, unvaccinated domestic dogs remain a significant reservoir for transmission. Postexposure prophylaxis can be life-saving in circumstances of high-risk animal bites. Japanese encephalitis is another serious viral infection that is transmitted by mosquitoes in South East Asia during the late summer and fall months. The annual incidence is estimated to be 30,000 to 50,000 cases in endemic areas, with 10,000 to 15,000 associated deaths. Vaccination is available to travelers who are at particularly high risk during times of peak transmission.
Fungi
CNS infections caused by fungi are generally considered to be rare and are mostly restricted to immune-compromised patients ( Table 3 ). Fungal organisms tend to cause chronic lymphocytic meningitis with a prolonged course of symptoms. The most common fungal organism encountered that causes CNS infection is Cryptococcus neoformans . This organism is a form of yeast with a large characteristic polysaccharide capsule that has a particular predilection for infection of the CNS. Patients infected with HIV with CD4 + T-cell counts of less than 100/μL have a reported incidence of infection of 6% to 13%. Prolonged corticosteroid use consisting of greater than 20 mg prednisone per day also is a risk factor, particularly for those with solid organ transplantation. It has been estimated that 20% of patients who develop cryptococcal meningitis have no underlying risk factor.
| Pathogen | Risk Factor | Incidence |
|---|---|---|
| Cryptococcus neoformans | Immune compromise, older age | Most common |
| Coccidioides immitis | Regional exposure | Regional |
| Blastomyces dermatitidis | Regional exposure, immune compromise | Rare |
| Histoplasma capsulatum | Regional exposure, immune compromise | Rare |
| Candida spp | Systemic infection | Rare |
| Aspergillus spp | Immune compromise, infection of structures adjacent to central nervous system | Rare |
| Zygomycetes | Immune compromise, infection of structures adjacent to central nervous system | Rare |
The second most common fungal organism to cause meningitis is Coccidioides immitis . This endemic fungal organism is found only in certain areas of the Sonoran desert in the southwestern United States and in certain areas of southern California. One-third to one-half of patients who have disseminated infection will develop meningitis. Immune-compromised patients are at higher risk for CNS infection. In one study from Tucson, Arizona, 27% of patients who had Coccidioides meningitis were found to have HIV infection complicated by AIDS.
Other fungal organisms are much less commonly observed to cause meningitis. Candida spp rarely invade the CNS in cases of intravenous drug use or in cases of systemic candidiasis in the setting of neutropenia. Other endemic fungi-related conditions such as blastomycosis or histoplasmosis also rarely invade the CNS and can lead to chronic meningitis or intraparenchymal CNS lesions. Finally, filamentous fungi such as Aspergillus , Zygomycetes, dematiaceous molds, and others all have been reported to cause CNS disease, mostly in instances of direct inoculation from trauma or direct extension from infection in adjacent structures such as the sinuses in patients with underlying diabetes or severe immune compromise.
Mycobacteria
Tuberculosis (TB) is the most common cause of CNS infection by mycobacteria. Meningitis caused by Mycobacterium tuberculosis tends to be characterized as a chronic process with chronic headache and a lymphocytic pleocytosis on CSF analysis. Tuberculosis cases increased substantially on a global scale when the HIV/AIDS epidemic began. In South Africa, of 60 patients presenting with meningitis type symptoms, 66% were infected by HIV and 9 had tuberculous meningitis. Since the 1990s in the United States, cases of TB have declined from 25,000 per year to 12,000 in 2008. 2000 of those cases were documented to be extrapulmonary TB, of which a fraction are cases of CNS infection. In a study from Denmark performed between 1988 and 2000 there were 20 patients with tuberculous meningitis, more than half of whom had come from countries of high TB endemicity. CNS infection with other atypical mycobacteria has not been commonly reported.
Parasites
Meningitis caused by parasitic organisms is rare. The organism most often associated is Strongyloides stercoralis , which can occasionally cause meningitis as part of the hyperinfection syndrome ( Table 4 ). Free-living amoeba such as Naegleria fowleri or Acanthamoeba can cause a rapidly fatal granulomatous meningoencephalitis. Although uncommon, occasional clusters of cases can be associated with children or young adults who swim in contaminated warm freshwater lakes. One study in Florida documented only 5 cases over 14 years, even though 58% of lakes were found to be contaminated with the organism. The larvae of the rat lungworm Angiostrongylus cantonensis , which is endemic to the tropics and southeast Asia, can cause an eosinophilic meningitis when humans become an accidental host, usually through ingesting contaminated mollusks. Worms that migrate through the CNS cause brain inflammation, resulting in neurologic sequelae such as cranial nerve paralysis. The epidemiology has not been systematically studied; however, approximately 2500 cases have been reported in the literature from various geographic locations including Hawaii and New Orleans, Louisiana.
| Pathogen | Risk Factor | Incidence |
|---|---|---|
| Strongyloides stercoralis | Regional exposure, immune compromise | Rare |
| Naegleria fowleri | Warm fresh water | Very rare |
| Angiostrongylus cantonensis | Regional exposure | Rare |
Other Organisms
A variety of organisms in other categories have also been associated with CNS infection ( Table 5 ). In the United States there are approximately 15,000 cases of Lyme disease, caused by infection with Borrelia burgdorferi , which is transmitted by ticks primarily in the northeastern states. Up to 15% of patients who are untreated will develop acute neuroborreliosis, which leads to chronic lymphocytic meningitis. Chronic CNS infection can occur in up to 5% of patients if left untreated. Syphilis can infect almost any organ including the CNS. Meningitis should be suspected particularly in patients with HIV infection with secondary syphilis. Most experts recommend lumbar puncture even in asymptomatic HIV-infected patients, because treatment strategies differ in patients with CNS involvement. Leptospirosis is one of the most common zoonoses. The spirochete is transmitted from animals to humans, usually by exposure to fresh water contaminated with infected animal urine. The organism can cause a multisystem illness in the first phase. In the second phase, an immune-mediated aseptic meningitis can develop in up to 80% of patients with a CSF lymphocytic pleocytosis. Over a 4-year period, 18 cases of CNS leptospirosis were identified in California when serology was retrospectively performed on patients with aseptic meningitis. Meningitis can also occur in the setting of infection with various rickettsial organisms. Rocky Mountain spotted fever, a tick-borne illness caused by Rickettsia rickettsii , can cause symptoms of meningismus in up to 18% of affected patients. Long-term neurologic sequelae were commonly detected, suggesting frequent CNS infection with this organism. Murine typhus, which is caused by Rickettsia typhi and is transmitted by fleas, can also rarely present with meningitis.
| Pathogen | Risk Factor | Incidence |
|---|---|---|
| Borrelia burgdorferi (Lyme) | Regional tick exposure | Regional |
| Treponema pallidum (syphilis) | Sexual transmission | Common with HIV coinfection |
| Leptospirosis | Contaminated fresh water | Regional |
| Rickettsia rickettsii | Tick borne | Regional |
| Rickettsia typhi | Fleas | Regional |
| Rickettsia prowazekii | Lice | Regional, epidemic |
| Rickettsia tsutsugamushi | Mites | Regional |
| Ehrlichia spp | Tick borne | Regional |
| Bartonella henselae | Cat-scratch | Rare |
| Coxiella burnetii | Contact with infectious material from infected animals | Rare |
Meningitis
Bacteria
When bacteria infect the CNS, in most cases an acute syndrome of headache, fever, nuchal rigidity, and change of mental status occurs. Meningitis caused by bacteria continues to be a significant clinical syndrome that requires rapid recognition and treatment by clinicians to prevent associated life-threatening complications. With the introduction of vaccination for certain pathogens, the epidemiology of bacterial meningitis has changed dramatically over the past 2 decades.
The number of cases of meningitis caused by Haemophilus influenzae type B decreased by 94% after 1988 when the vaccine was introduced to a rate of 0.2 cases per 100,000. Unvaccinated adults with nontypable H influenzae now make up the majority of cases. Meningitis caused by Streptococcus pneumoniae has decreased 30%, from 1.1 cases per 100,000 in the late 1990s to 0.79 per 100,000 in the period 2004 to 2005. This decrease occurred after the introduction of the 7-valent conjugate pneumococcal vaccine for children, which was licensed in 2000. This decrease in incidence has extended to not only children but also adults, presumably secondary to herd immunity. However, other pneumococcal serotypes not covered in the vaccine are now being seen with increased frequency in certain locations. Mortality rates attributable to pneumococcal meningitis have remained the same at around 21% for adults and 8% for children. Other pathogens such as Neisseria meningitidis (0.6/100,000), Group B streptococcus (0.3/100,000), and Listeria monocytogenes (0.2/100,000) occur less frequently.
The patient’s age and immune status affects the organism most likely to be present in bacterial meningitis ( Table 1 ). While pneumococcus remains the most common in all age groups, organisms such as Listeria are more likely to be observed in older and immune-compromised patients. Group B streptococcus and gram-negative organisms such as Escherichia coli are most common in neonates who develop meningitis related to exposure to urogenital flora at the time of birth. Outbreaks of meningococcal meningitis occur under conditions of crowding. Clusters of cases have been reported on college campuses and with religious gatherings such as the Hajj. For the Hajj, vaccination programs have been initiated such that visitors are required to have received the quadrivalent meningococcal vaccine, which has decreased the incidence of invasive infection substantially. However, pilgrims often can still become colonized with N meningitidis and can therefore transmit the organism to household contacts on their return home, which has led to outbreaks in several European countries. In 2000 there were 25 cases per 100,000 pilgrims to the Hajj from Singapore. In addition, there was a subsequent attack rate of 18 cases per 100,000 in household contacts who were exposed to returning pilgrims. Therefore, there are now recommendations for household contacts of at-risk travelers to also receive the meningococcal vaccine.
| Pathogen | Risk Factor | Incidence |
|---|---|---|
| Streptococcus pneumoniae | Day care, HIV infection | Most common |
| Neisseria meningitidis | Crowded conditions | Outbreaks |
| Haemophilus influenzae | Significantly less common after vaccination | |
| Listeria monocytogenes | Immune compromise, elderly | Less common |
| Group B streptococcus | Neonates | Decreased with antenatal detection of group B streptococcus |
| Escherichia coli | Neonates | Less common |
| Mycobacterium tuberculosis | Exposure, older age, immune compromise | Rare |
The performance of a lumbar puncture is the first step in the evaluation of any patient suspected of meningitis or encephalitis. Imaging of the brain is often indicated in patients with neurologic deficits, immune-compromising conditions, or decreased level of consciousness. In one study, 45% of patients with bacterial meningitis met criteria for CNS imaging. If a mass lesion is present, there is risk for brain herniation at the time of cerebrospinal fluid (CSF) withdrawal.
Viruses
CNS infections caused by viruses are often referred to as aseptic meningitis because traditional bacterial cultures from the CSF are negative. Patients tend to present in a subacute fashion with headache and fever. There are many viruses that can cause aseptic meningitis ( Table 2 ). A study performed in Finland analyzing consecutive adult patients with aseptic meningitis found that 26% of cases were related to enteroviruses, 17% to herpes simplex virus (HSV)-2, and 8% related to varicella zoster virus (VZV). Of patients with encephalitis, VZV was found in 12% of cases and HSV-1 in 9%, with tick-borne viruses identified in 9%. In 44% of patients, a specific cause was not confirmed. Because viral culture is difficult and insensitive, molecular testing via the polymerase chain reaction (PCR) from CSF has greatly aided in the diagnosis of meningitis caused by viruses. With these techniques it has been shown that more than 90% of cases of aseptic meningitis are caused by enteroviruses in other studies. Enterovirus infection typically occurs in the summer to fall months and is most common in children, although it is also the most common cause of aseptic meningitis in adults. Outbreaks have been identified in various locations globally, including a large outbreak described in Taiwan in patients who also had associated hand-foot-and-mouth disease.
| Pathogen | Risk Factor | Incidence |
|---|---|---|
| Enteroviruses | Warm weather | Most common |
| Herpes simplex virus | Presence of latent virus | Common |
| Varicella zoster virus | Presence of latent virus, immune compromise | Occasional |
| West Nile virus | Mosquito borne | Outbreaks, declining in USA |
| La Crosse virus | Mosquito borne | Rare |
| Dengue | Mosquito borne | Regional outbreaks |
| Human herpesvirus 6 | Immune compromise | Rare |
| Lymphocytic choriomeningitis | Exposure to contaminated rodent excreta | Rare |
| Powassan virus | Regional tick exposure | Very rare |
| Chikungunya virus | Regional mosquito exposure | Regional outbreaks |
| Rabies | Exposure to infected animals | Rare |
| Japanese encephalitis | Summer, Southeast Asia | Regional |
| Mumps | Setting of outbreak | Very rare |
| HIV | Unprotected sexual exposure | Rare |
| Adenovirus | Outbreaks | Rare |
| Influenza | Seasonal epidemics | Rare |
Viral CNS infections often also can cause encephalitis. This situation occurs when there is infection of the brain parenchyma with associated inflammation, which is accompanied by changes in mental status and behavior, and sometimes reduced level of consciousness. Overall, it is estimated that there are 10.5 to 13.8 per 100,000 hospitalizations for children and 2.2 per 100,000 hospitalizations for adults for acute encephalitis syndrome. In one review, from 1950 to 1981 in Minnesota, there were 7.4 per 100,000 hospitalizations for encephalitis, with a specific virus identified in 25% of the cases. Early in the study period mumps and arboviruses were most common. The epidemiology of viral meningitis and encephalitis has been significantly altered by vaccination. In the 1940s and 1950s, mumps virus was encountered as a cause of viral meningitis in 15% of cases. Occasional outbreaks of mumps still occur; however, meningitis caused by this virus is now rare. In the Minnesota study, no cases of mumps-related encephalitis occurred after 1972.
Viruses transmitted by arthropod vectors that cause encephalitis and meningitis have become more common in recent years. During the summer of 1999, West Nile virus was recognized as having caused a widespread epidemic that began in New York City and eventually spread across the United States along bird-migratory routes. In 2002 there were 2942 cases of neuroinvasive West Nile disease, which represented 71% of the cases of viral meningoencephalitis reported. The incidence of West Nile–associated meningitis peaked in the late summer months during the years of increased incidence. As immunity has developed and the susceptible reservoir of bird populations has decreased, the incidence of West Nile encephalitis has decreased substantially in recent years. In 2009 there were only 373 cases of encephalitis or meningitis reported.
There are a variety of other arthropod-transmitted viruses that can cause meningitis and that have certain geographic distributions. St. Louis encephalitis, La Crosse virus, and Eastern Equine encephalitis are endemic within the United States and are observed to cause disease sporadically, from 0.01 to 0.04 cases per 100,000. Dengue is caused by a group of 4 viruses transmitted by mosquitoes and is a common cause of viral meningitis in tropical areas, particularly in South and Central America. The World Health Organization estimates that 50 million people are infected by dengue yearly. In the Americas in 2007 there were 890,000 cases reported, with 26,000 cases complicated by dengue hemorrhagic fever. In recent history dengue has not been endemic in the United States; however, in 2009 28 cases of dengue were identified in individuals who either traveled to or lived in Key West, Florida. Thus, as with West Nile virus, emerging pathogens are able to become endemic in new geographic locations including the United States.
Reactivation or new infection with herpes viruses can also lead to infection in the CNS. The diagnosis of these infections has also been transformed by the ability to apply molecular techniques such as the PCR, although occasional false-negative results may be obtained. HSV-2 most commonly causes meningitis and can be associated with primary infection while HSV-1 can cause necrotizing encephalitis with significant neurologic sequelae. In a study performed in Sweden, there were 2.2 cases per million population of HSV-1–related encephalitis per year. Attributable mortality was 14%, with 21% of surviving patients having developed a seizure disorder as sequelae. HSV-1 has also been linked to a recurrent, benign lymphocytic meningitis known as Mollaret meningitis, which is considered to be rare. In this syndrome patients present with recurrent aseptic meningitis in which HSV-1 DNA has been found in some patients. In immune-compromised patients with solid organ transplantation or stem cell transplantation, human herpesvirus 6 (HHV-6) can cause meningitis or encephalitis when latent virus reactivates. Similarly, VZV can cause meningitis or encephalitis in immune-compromised patients when reactivation occurs in the setting of zoster or disseminated disease in those who are susceptible to primary infection.
Other less commonly encountered viruses are listed in Table 2 and include lymphocytic choriomeningitis virus, which can occur after exposure to contaminated rodent excreta. HIV infection can cause an aseptic meningitis–type syndrome at the time of acute infection and should be considered in patients with risk factors such as recent high-risk sexual contact. Neurologic disorders including aseptic meningitis have been described in up to 12% of patients who develop the acute retroviral syndrome associated with the acquisition of HIV infection. The clinician also must be aware of outbreaks that are occurring in various geographic areas to which patients may have traveled or where they reside. Powassan virus is transmitted by ticks and can cause encephalitis. This rare virus has been found to cause disease mostly in Maine, Vermont, and New York, where 7 cases were reported between 1999 and 2005. In an outbreak of Chikungunya virus on La Reunion Island from 2005 to 2006, out of 274 patients evaluated 70% had symptoms of headache. CNS symptoms have been reported rarely, but CNS pleocytosis has not been observed with this infection. Meningitis has rarely been reported as a complication of influenza. A large study conducted in Great Britain identified only 0.01% (21) of more than 141,000 patients with influenza-like illness who had developed this complication.
Infection with the rabies virus leads to severe encephalitis and carries a very high mortality rate. The incidence of human infection with rabies has declined substantially in the United States, from 33 cases in 1946 to 3 cases in 2006. Most cases of rabies occur after exposure to infected wild animals such as bats, skunks, raccoons, or foxes. In other locations globally, unvaccinated domestic dogs remain a significant reservoir for transmission. Postexposure prophylaxis can be life-saving in circumstances of high-risk animal bites. Japanese encephalitis is another serious viral infection that is transmitted by mosquitoes in South East Asia during the late summer and fall months. The annual incidence is estimated to be 30,000 to 50,000 cases in endemic areas, with 10,000 to 15,000 associated deaths. Vaccination is available to travelers who are at particularly high risk during times of peak transmission.
Fungi
CNS infections caused by fungi are generally considered to be rare and are mostly restricted to immune-compromised patients ( Table 3 ). Fungal organisms tend to cause chronic lymphocytic meningitis with a prolonged course of symptoms. The most common fungal organism encountered that causes CNS infection is Cryptococcus neoformans . This organism is a form of yeast with a large characteristic polysaccharide capsule that has a particular predilection for infection of the CNS. Patients infected with HIV with CD4 + T-cell counts of less than 100/μL have a reported incidence of infection of 6% to 13%. Prolonged corticosteroid use consisting of greater than 20 mg prednisone per day also is a risk factor, particularly for those with solid organ transplantation. It has been estimated that 20% of patients who develop cryptococcal meningitis have no underlying risk factor.