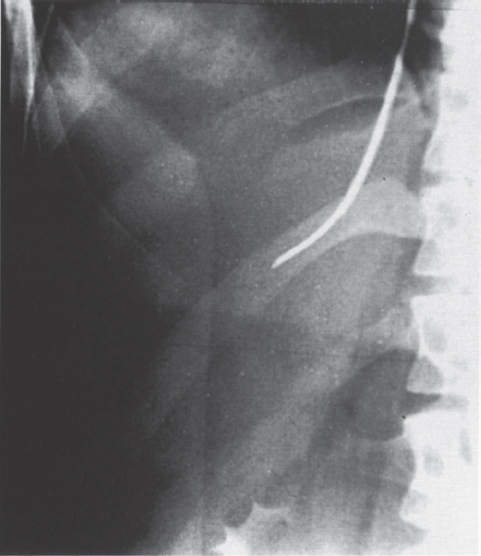
Etiology Through cross-sectional imaging and angiographic/hemodynamic studies, the radiologist plays a significant role in the evaluation of the patient with advanced liver disease. A team approach is required to manage complex cases involving deteriorating liver function. The interventional radiologist continues to be directly involved by reducing elevated portal pressure through the application of the transjugular intrahepatic portosystemic shunt (TIPS) procedure. In this chapter, we briefly discuss (1) the definition of the terms cirrhosis and portal hypertension, (2) the etiology of portal hypertension, (3) the angiographic (hernodynamic) evaluation of patients with portal hypertension, and (4) the role of TIPS in treating patients with advanced liver disease. Cirrhosis is a pathologic diagnosis. A biopsy (Fig. 1–1) demonstrating hepatic fibrosis confirms the diagnosis. Portal hypertension is a clinical diagnosis. The hemodynamic changes observed in patients with portal hypertension require an understanding of the blood supply to the liver. Approximately 75% of the hepatic blood supply originates from the portal venous system, with the remainder coming from the hepatic artery. The spleen and gastrointestinal tract are the primary sources from which portal venous blood originates. Blood drains from the portal veins, through hepatic sinusoids, and into the hepatic veins.1–4 To understand and simplify the hemodynamic alterations observed in patients with portal hypertension, an appreciation of the level of obstruction to hepatic blood flow is necessary. Understanding the level of obstruction explains the clinical findings. Obstruction may occur in the following locations: (1) before blood enters the liver, (2) in the liver itself, or (3) after blood leaves the liver. The increased resistance to blood flow through the liver at any point along this sequence results in portosystemic collaterals. Portosystemic collaterals (Fig. 1–2) often bring the patient to immediate medical attention in the form of life-threatening esophageal variceal bleeding. A partial list of other less impressive, but clinically important, portosystemic collaterals includes the following: (1) re-canalized paraumbilical vein, (2) spontaneous splenorenal shunt, (3) other splenic collaterals, and (4) hemorrhoidal veins. Multiple other physiologic changes are associated with advanced liver disease, including ascites and coagulopathy. As mentioned, the portosystemic collaterals that bring the patient to immediate medical attention are bleeding esophageal varices. After hemodynamic stabilization in an intensive care setting, endoscopy is often performed, followed by variceal sclerotherapy or banding. Multiple endoscopic procedures frequently are required to treat the patient effectively. In patients with portal hypertension who are awaiting hepatic transplantation and have failed sclerotherapy and banding, the TIPS procedure has been used effectively.5–7 To define more fully the hemodynamic alterations seen in patients with portal hypertension, obstruction to hepatic blood flow may be seen before blood reaches the hepatic sinusoids; this is called presinusoidal portal hypertension. Obstruction to blood flow at the level of the sinusoids is termed sinusoidal portal hypertension. If obstruction occurs as blood exits the hepatic sinusoids, the patient is said to have postsinusoidal portal hypertension. A mixed pattern frequently is found in patients with advanced liver disease. FIGURE 1–1. Anteroposterior (AP) spot film obtained during transvenous hepatic biopsy. A 16-gauge Colapinto transjugular liver biopsy needle (Cook, Inc., Bloomington, IN) was placed through a protective 9F angled sheath. In this image, the needle tip exits the sheath, leaves the right hepatic vein, and enters hepatic parenchyma. In patients with advanced liver disease, thrombocytopenia, and coagulopathies, such a technique provides an alternative method for obtaining hepatic tissue. In such patients, the conventional percutaneous transhepatic biopsy often is associated with significant risks of hemoperitoneum and other bleeding complications. The etiology of portal hypertension is varied, resulting in obstruction at (1) presinusoidal, (2) sinusoidal, (3) postsinusoidal, or (4) mixed levels. The four levels of obstruction may be simplified angiographically (hemodynamically) and functionally into (1) presinusoidal or (2) postsinusoidal obstruction. Any disease that reduces portal vein flow before it reaches the hepatic sinusoids results in the same hemodynamic change (presinusoidal). The disease process may be intrahepatic or extrahepatic. Similarly, despite multiple etiologies, sinusoidal and postsinusoidal causes of portal hypertension are hemodynamically similar. Disease processes affecting the sinusoids or the outflow of blood from the hepatic sinusoids result in the same hemodynamic or angiographic findings (postsinusoidal).

Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree



