15 Evaluation of Hand and Finger Masses
♦ Setup
Probe Selection
• A high-frequency linear transducer (12-17 MHz) should be used. This results in:
○ High image resolution, resulting in improved image quality
○ Limited sound beam penetrance (depth)
– Usually not a concern in the hand or finger because of the superficial nature of structures
– May require the use of a lower-frequency curved-array transducer (5-9 MHz) if visualization of deeper structures is necessary
○ Sound waves propagating parallel to the transducer face, which allows optimal assessment of linear structures such as ligaments or tendons
• The size of the structure to be imaged may predicate transducer choice. For example, a linear array hockey stick probe (Fig. 15.1a) may be ideal to assess small structures in the digits, such as the flexor tendon pulley system. A high-frequency linear array probe with a wider footplate (Fig. 15.1b) may be preferable in the remainder of the hand or wrist to provide a wider field of view, as in assessment of the carpal tunnel.

Fig. 15.1 (a) A hockey stick high-frequency 18 MHz linear probe. (b) A high-frequency 15 MHz linear array probe with a larger footplate.
Technical Factors
• A judicious amount of acoustic transmission gel should be used to facilitate contact between the probe and skin surface, allowing more efficient transmission of the sound beam and receipt of returning echoes.
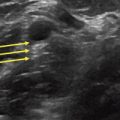
• For surface-based or superficial structures, a thick layer of transmission gel should be used (Fig. 15.2). This minimizes distortion of the soft tissue planes from probe pressure.
• Gain should be adjusted to optimize image brightness.

Fig. 15.2 Grayscale ultrasound image of a superficial complex cystic structure (arrowheads). A thick layer of acoustic transmission gel (G) was used to maintain a highly uniform image quality.
♦ Probe Positioning
• The probe should be centered over the area of interest.
• The probe should be placed parallel and perpendicular to the palpable abnormality at 90-degree intervals; this allows acquisition of static transverse and longitudinal images.
• If the lesion is large, panoramic or extended field-of-view imaging (Fig. 15.3) may be necessary to fully depict and measure the abnormality or to present a global evaluation of lesion architecture, echogenicity, and margins.
• Cine imaging, obtained by creating a single loop of contiguous static ultrasound images, can be helpful to further delineate the relationship of a mass lesion with the surrounding soft tissue structures or identify the origin of a lesion, such as a ganglion cyst.
• Dynamic maneuvers can also add useful information about lesion characteristics.
○ For example, dynamic maneuvers can suggest that a soft tissue mass is a lipoma if it is soft and pliable or that a lesion is cystic if there are free-flowing internal echoes during graded compression.
○ Transducer pressure can elicit point tenderness when scanning an abnormality.
• Doppler imaging allows assessment for the presence of blood flow, indicating the presence of lesion hyperemia (as can be seen with inflammation or tumor neovascularity).
○ Color Doppler can differentiate direction of flow.
○ Power Doppler is more sensitive to the presence of blood flow but indiscriminate to flow direction.
○ Doppler settings must be appropriately adjusted; if color gain is too low, imaging may be false-negative for the presence of flow, and if color gain is too high, falsepositive flow may be detected by actions such as probe movement.

Fig. 15.3 Panoramic grayscale ultrasound image of a well-circumscribed, anechoic superficial fluid collection representing a posttraumatic Morel-Lavallée lesion. Extended-field-of-view imaging allows complete visualization and measurement of this structure.
♦ Normal Anatomy
Fig. 15.4 shows the normal appearance of the soft tissue structures:
• Dermis and epidermis: hyperechoic
• Subcutaneous fat: hypoechoic fat with internal echogenic fibrous septa
• Fascia: thin hyperechoic interface at the interface of soft tissue structures
• Muscle: hypoechoic muscle with fine interposed hyperechoic fibroadipose septa
• Bone: very hyperechoic with posterior acoustic shadowing and posterior reverberation
• Lymph nodes: demonstrate a lobular or reniform morphology with a peripheral hypoechoic cortex and a central echogenic fatty hilum (Fig. 15.5)
○ Lymph nodes characteristically demonstrate blood flow to the hilum but should not routinely demonstrate flow within the cortex; if present, this is concerning for a pathologic process.

Fig. 15.4 Transverse (a) and longitudinal (b) grayscale ultrasound imaging of normal soft tissue structures, including the dermis and epidermis (D), subcutaneous fat (SQ), fascia (F), muscle (M), and bone (B).

Fig. 15.5 Grayscale (a) and color Doppler (b) imaging of an ovoid, well-circumscribed structure representing a normal lymph node. A characteristic echogenic central fatty hilum (arrowhead) with a vascular stalk (arrow) is evident.
♦ Pathologic Anatomy
Ultrasound Features of Cysts
• Cystic structures, especially ganglion and synovial cysts, are the most common masses in the hand and wrist, encompassing approximately 60% of hand and wrist masses.
• Simple cysts are well-circumscribed, anechoic masses with posterior acoustic enhancement (Fig. 15.6).
○ Cysts may contain thin internal septations or fine internal echoes.
○ Internal vascularity within cystic structures is usually absent on color or power Doppler.
○ Cysts may have varying degrees of peripheral (pseudocapsular) flow depending on the degree of associated inflammatory changes.
• More complex cysts may demonstrate increased echogenicity, internal debris, or a multilocular configuration.
• Cysts may alter morphology with a degree of decompression or manifest free-flowing internal echoes with graded pressure during dynamic maneuvers.
• In the setting of ganglion or synovial cysts, the cyst often demonstrates a thin neck in continuity with a joint space or tendon sheath.
• In the hand and wrist, cysts tend to occur in common locations:
○ Dorsal wrist: near the dorsal band of the scapholunate ligament
○ Volar radial wrist: adjacent to the flexor carpi radialis tendon or the radial nerve with its palmar branch
○ Flexor tendon sheath: especially around the A1 pulley of the metacarpophalangeal joint.