Prevention
There are essentially three forms of prevention:
Primary prevention: Primary prevention aims to actually prevent the occurrence of a disease, thus decreasing its incidence. Colonoscopy is a good example of this: polyps, which are (at this stage) benign lesions with a high risk of malignancy, can be removed, so that colon cancer does not develop. Avoiding the use of hormone replacement therapy during menopause is an example of primary prevention of breast carcinoma. However, imaging per se does not qualify as primary prevention.
Secondary prevention: Secondary prevention aims to reduce the mortality of a disease that has already developed. This is most successful when a carcinoma is discovered at an early stage (early detection), which is made possible in practice through imaging examinations.
Tertiary prevention: The aim of tertiary prevention is also to reduce mortality (improving overall survival) and the impact of manifest disease. Follow-up care is a form of tertiary prevention.
10.2 Early Breast Cancer Detection (Secondary Prevention)
In most cases, breast cancer is a slow-growing tumorous process. Depending on the tumor grade, one can assume an average tumor doubling time of between 150 and 300 days. This rather low growth rate is an essential premise for the systematic application of imaging diagnostics with the objective of early tumor detection. It is also the basis for the usually recommended examination interval of 1 to 2 years. Assuming a high-quality examination strategy with a high sensitivity for the detection of breast cancer, a breast carcinoma should not reach an advanced tumor stage within this interval. Exempt from this are the inherently highly aggressive breast carcinomas with extremely high proliferation rates, which fortunately represent the exception to the rule.
The goal of an effective breast cancer early detection strategy must be to detect breast cancer at a prognostically favorable stage. In essence, there are two different tumor constellations to be considered in this regard:
Early detection at the DCIS tumor stage: The diagnosis of intraductal breast carcinoma, in and of itself, implies an early diagnosis even though the tumor occasionally may extend over several centimeters by the time the diagnosis is made. As a localized disease of the breast, an intraductal tumor does not extend into the locoregional lymph nodes or disseminate to generate remote metastases. In considering DCIS, however, it is important to note that—especially in the group of DCIS with a low proliferation rate—a high proportion of tumors will not grow beyond the mammary duct to threaten the woman during her lifetime. For this reason, the issue of potential overdiagnosis with the associated overtreatment of the patients thus affected is an area of ongoing discussion.
Early detection at an invasive tumor stage with tumor size less than 10 mm: An invasive breast carcinoma is considered to be detected early if it has a diameter of less than 1 cm when discovered. Breast cancers at such stages (pT1a, pT1b) exhibit an extremely low rate of metastasis to locoregional lymph nodes or parenchymatous organs, so that the long-term survival rate is usually excellent (over 95%). Here there is no controversy regarding overdiagnosis, because untreated invasive carcinoma usually leads to death.
Note
Although DCIS is considered a very early, noninvasive breast cancer, it may already be several centimeters in size when detected.
In addition to the clinical breast examinations (by inspection and palpation), other means for the early detection of breast cancer generally include the established imaging examination techniques of mammography, breast ultrasonography, and breast MRI.
Inspection and palpation: Study data demonstrate that periodic inspection—and in particular palpation of the female breast —does not offer any survival advantage, because breast cancers discovered by this approach already average 2 to 3 cm in size. However, Women who regularly examine their breasts are also more consistent in their participation in early detection imaging programs.
Take Home Point
Used as the sole method for breast cancer detection, breast self-examination cannot decrease the breast cancer mortality rate.
Mammography: X-ray mammography is the only imaging technique that has been shown to reduce the mortality of breast cancer in a quality-controlled and population-based mass screening program. The relevant data, originating from the United Kingdom in the 1970s, has demonstrated a reduction in mortality of 30% through the implementation of mammographic screening in a group of women who had not previously had mammography.
Take Home Point
General recommendations call for the use of mammography in quality-assured screening programs. Recommendations to attend screening vary across countries and organizations. In general, it is recommended that women begin mammography screening at an age 40 to 50 years, at an interval of once every 1 to 2 years.
Breast ultrasonography: Breast ultrasonography is not appropriate for use as the sole examination method in the early detection of breast cancer. Nevertheless, it represents an important supplementary method to compensate for the limitations of other imaging methods. In younger women, however, it is the primary method of choice.
Take Home Point
Sonography is not suitable for use as the sole diagnostic method in the early detection of breast cancer.
Breast MRI: Data from studies in the last 10 years document the great significance of breast MRI in the detection of early and small carcinomas, in particular. In this regard, MRI is clearly superior to all the other imaging examination methods, provided that high technological and methodological standards are assured and the radiologists who do the evaluation have sufficient expertise.
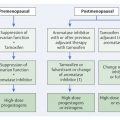
In European statistics, approximately 25% of all of diagnosed breast carcinomas are detected within the mammography screening program. The remaining 75% are diagnosed either within individualized and risk-adapted early detection frameworks or after the diagnostic work-up of clinical symptoms (▶ Fig. 10.1).

Fig. 10.1 Detection rate of breast cancer within and outside of screening programs. Red bars = carcinomas detected within the screening program in the 50- to 69-year-old group of participants. Yellow bars = rate of interval carcinomas (ca. 30%). Green bars = carcinomas found in women not participating in screening (ca. 30% of women 50–69 years old with an assumed participation rate of 70%). Blue bars = carcinomas detected in women outside the screening age range; i.e. women under 50 years and over 70 years.
10.2.1 Mammography Screening
“Screening” refers to a systematic testing strategy aiming to identify a particular characteristic within a defined number of specimens or people.
Note
The goal of breast cancer screening programs is to reduce the breast cancer mortality rate in a sustained manner by diagnosing malignant tumors of the breast at the earliest possible and prognostically most favorable stage.
History
Comprehensive mammography screening programs have been operating in various countries for over 40 years. The Netherlands, Sweden, Norway, and Finland implemented an organized, mass screening program for women without symptoms in 1974, and the United Kingdom in 1979. Canada has also had an organized program for many years. Studies have demonstrated that a 25–30% decrease in mortality is possible through the institution of a quality-controlled screening program. It should be noted, however, that in many of these countries there had been no previous mammographic examinations in the population before the introduction of mammography screening. This was not the case for the population in Germany when screening was introduced in 2005.
In general, mammography screening programs are population-based, quality-controlled and well-structured. They typically offer women between the ages of 50 and 69 years biennial participation in a program for early detection of breast cancer on the basis of an invitational system. For women under the ages of 40 to 50 years, screening mammography has not been shown to offer any advantages because of the higher percentage of false -positive findings in younger women. This can, at least in part, by the higher breast tissue density in younger women, which limits the overall sensitivity of the X-ray imaging. Data substantiate that the incidence of interval carcinomas in this group (women 40 to 49 years old) in the first screening round is approximately 50%. Mammography screening programs are subject to a comprehensive quality assurance program in terms both of equipment and technical aspects and of the training of the radiologist and the radiologic technologist personnel. The relevant quality-assurance measures are evaluated regularly.
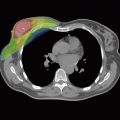
The screening mammography images are assessed by at least two specially trained reviewers, who evaluate the images independently. If at least one of the reviewers determines that the mammography requires clarification, then a final assessment is made by way of a consensus conference under the direction of the physician responsible for the program. ▶ Fig. 10.2 illustrates a typical overall structure of a national mammography screening program, using Germany as an example.

Fig. 10.2 Structure of a mammography screening program, using Germany as an example.
(From the 2008–2009 evaluation report of the Kooperationsgemeinschaft Mammographie [Mammography Cooperative, Berlin] 2012, modified.)
For mammography screening programs, it is assumed that the effect on mortality reduction will be detectable, at the earliest, after a period of at least 10 years. The analysis of surrogate performance parameters enables earlier evaluation of the effectiveness of the program and also allows possible side effects to be registered and minimized. The results are published regularly.
Criteria for a Screening Program
Screening programs designed to examine a large group of people to detect a disease at an early stage make sense only if certain criteria are met:
The illness must constitute a relevant public health concern.
The illness must be treatable, that is, have distinctly improved treatment outcome when detected early.
The screening examination method used should exhibit a high degree of sensitivity so as to detect the disease as reliably as possible.
The screening examination method used should exhibit a high degree of specificity so as to recognize healthy people as such and to protect them from overdiagnosis.
The screening examination method used should be time- and cost-effective.
The screening examination method used should have as little a negative impact as possible on those examined.
Advantages
The existence of a screening program motivates women who would not otherwise do so to undergo early detection mammography.
The screening quality specifications usually distinctly improve the quality of the examination devices used and also of the participating medical and technical radiology assistants and physicians. The quality requirements and the mandated periodic advanced training courses are instrumental in this regard.
Disadvantages
False-positive screening results can cause unnecessary concern and anxiety to patients. Additional costs may be incurred due to the necessity for further examination procedures to clarify any such ambiguous findings. With false-negative findings, the goal of screening has been completely missed since, in spite of a screening examination having been performed, a malignant tumor that is present has not been detected. In the case of mammography screening, this is particularly true for women with high tissue density, for whom the sensitivity of mammography falls to 30 to 40% when no complementary examination procedure is used.
It is a subject of debate whether some women may be diagnosed at an early breast cancer stage without any resulting extension of their lifespan. Rather there is often a reduction in the quality of life due to the diagnosis of “breast cancer” and the subsequent therapy that in retrospect was unnecessary therapy (for example, low-grade DCIS). Tumors may indeed be detected earlier without this leading to an increase in the life expectancy, resulting in an increase in the patient’s time with a diagnosed disease and all the subsequent disadvantages (for example, metastasized breast carcinoma).
Patient Information
Given the potential disadvantages of a screening program, it is essential for individuals considering screening to be appropriately and accurately informed of both its advantages and its disadvantages. Only so informed can they decide for themselves whether they wish to participate in a screening program.
Terminology Used in Screening
Invitation rate: the percentage of eligible women invited to participate in a mammography screening program (including self-invitees).
Background incidence: the incidence of invasive tumors to be expected in the target population in the absence of an active screening program.
Interval carcinoma: breast cancer (invasive or in situ) detected after a negative screening examination (including diagnostic work-up, if performed) and before the next regular screening appointment.
Incidence (rate): the number of new occurrences of a particular disease in a population group of a defined size (usually per 100,000) during a determined time (usually one year).
Longitudinal evaluation: comparison of outcomes in one region over several time intervals.
Mobile mammography unit: semitrailer or van with built-in mammography unit for mobile use.
Mammography facility: a stationary facility or mobile unit that is approved to perform mammography as part of the mammography screening program.
Multidisciplinary case conference: a conference in which all existing study results for a patient are reviewed and correlated, and the future management of the patient is discussed and decided upon. Meeting participants include all the physicians who were involved in the patient’s diagnosis and treatment, including nonmedical personnel, as appropriate. This includes, in particular, the physician in charge of screening, pathologist, reviewer, radiology specialists, surgeon, cooperating hospital radiologist or pathologist, and the treating family doctor or gynecologist.
Performance indicator: a parameter used to evaluate the process quality (in the mammography screening program, the performance indicators include all the steps of the examination chain: the invitation process, the findings, and the diagnostic work-up).
PPV I (▶ Table 10.1): the positive predictive value of abnormal findings at screening: the percentage of all positive screening examinations (usually BI-RADS 0, 3, 4, and 5) that result in a tissue diagnosis of cancer within a defined time period (= true-positive examinations/positive screening examinations).
PPV II (▶ Table 10.1): the positive predictive value of examinations resulting in the recommendation for tissue diagnosis: the percentage of all diagnostic and screening examinations (BI-RADS 4, and 5) that result in a tissue diagnosis of cancer within a defined time period (= true-positive examinations/positive examinations recommending tissue diagnosis).
Cross-sectional evaluation: comparison of outcomes from different regions within a specified time interval.
Recall: invitation to a woman who has participated in mammography screening to return for diagnostic work-up after the mammographic reading because of a suspicious finding on mammography; or due to a clinical suspicion, when there is no mammographic suspicion (clinical recall); or if it is determined that there is a deficiency in the diagnostic image quality and repeat imaging is recommended, when there is no mammographic or clinical suspicion (technical recall).
Recall rate (abnormal interpretation rate): the percentage of all screening examinations interpreted as positive (usually BI-RADS 0, 4, and 5) resulting in an invitation for the woman to return for diagnostic work-up (= positive examinations/all examinations).
Surrogate parameter: a parameter for short and mid-term assessment and monitoring of the effectiveness and quality of a screening program used before the actual efficacy in mortality reduction can be ascertained and analyzed.
Certification and recertification of the screening facilities (using Germany as an example): comprehensive evaluation of the screening facilities including the participating personnel and the organizational structures, with regard to the quality of the structure, process, and results, by means of published protocols on behalf of the German National Association of Statutory Health Insurance Physicians (the certification takes place after issuing the license and before the onset of the public service mandate; the recertification takes place for the first time after 6 months, and subsequently at regular intervals of 30 months following the public service mandate).
Parameter | Reference range | Screening results | |
Initial examination | Follow-up examination | ||
Participation rate (%) | >70 | 53.7 | |
Recall (%) | <7 | 6.1 | 3.0 |
Breast cancer detection rate (cases per 1,000 participants) (‰) | No data | 8.2 | 5.6 |
Proportion DCIS (%) | 10 / >15 | 19.5 | 19.8 |
Proportion invasive carcinoma ≤10 mm (%) | ≥25 / ≥30 | 30.0 | 34.9 |
Proportion invasive carcinoma <15 mm (%) | 50 / >50 | 51.3 | 57.2 |
Proportion invasive carcinoma, lymph node negative (%) | >70 / >75 | 74.8 | 79.0 |
Proportion carcinoma, UICC stage ll+ (%) | <30 / <25 | 28.9 | 24.2 |
Proportion carcinomas confirmed preoperatively (%) | 90 / >90 | 91.7 | |
PPV I (%) | No data | 14.8 | |
PPV II (%) | No data | 49.4 | |
Abbreviations: PPV, positive predictive value; UICC, Union for International Cancer Control. Source: Kuhl CK, Schrading S, Weigel S, et al. Die “EVA”-Studie: Evaluierung der Leistungsfähigkeit diagnostischer Verfahren (Mammographie, Sonographie, MRT) zur sekundären und tertiären Prävention des familiären Mammakarzinoms—Zwischenergebnisse nach der ersten Hälfte der Förderungsperiode. Rofo 2005;177(6):818–827. | |||
10.2.2 Individualized Examination Concepts
Individualized and risk-adapted examination schemes produce a higher rate of early breast cancer detection, but they also involve higher costs than a comprehensive mammography screening program.