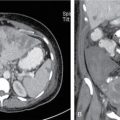
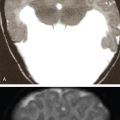
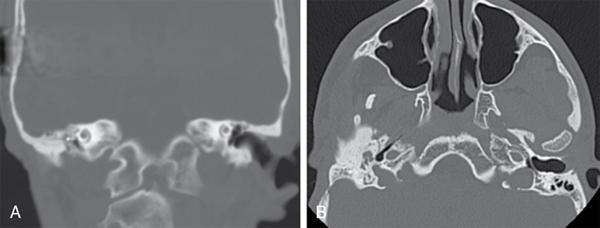
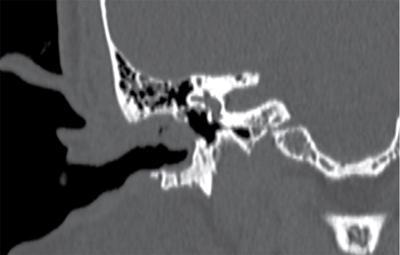
Amol Gautam External ear plays significant role in the conduction of sound and is involved by various pathologies. Cross-sectional (MDCT and MRI) imaging has revolutionized the way physicians look at complex anatomy and pathologic processes of temporal bone. MDCT is the modality of choice for different external ear pathologies and middle and inner ear are also evaluated well. MRI is performed for internal auditory canal, CP angle cisterns and seventh-eighth nerve pathologies. Combination of MDCT and MRI is needed prior to cochlear implant. External ear plays significant role in the conduction of sound and is involved by various pathologies. Cross-sectional (MDCT and MRI) Imaging has revolutionized the way physicians look at complex anatomy and pathologic processes of temporal bone. MDCT is the modality of choice for different external ear pathologies and middle and inner ear are also evaluated well. MRI is performed for internal auditory canal, CP angle cisterns and seventh-eighth nerve pathologies. Combination of MDCT and MRI is needed prior to cochlear implant. Please refer to Chapter 3.30 for temporal bone imaging anatomy. Auricle: Develops from ectoderm of first and second branchial arch. Begins at 40–45th day and fully formed by fourth month in utero. External Auditory Canal: Develops from first and second branchial arch grooves and begin around sixth month and completes its formation by seventh month. Approach to lesions of the EAC: differential diagnosis include Developmental abnormalities of the EAC most commonly occur due to defects of the first and second branchial arches and first branchial cleft during embryogenesis as well as in association with abnormalities of the external ear. EAC atresia (ranges from membranous atresia to complete bony occlusion) is rare, has an incidence of 1 in 10,000 to 20,000 births and is bilateral in one-third of patients. It more commonly affects the right ear. It has multiple syndromic associations like Treacher Collins, Goldenhar, and Pierre Robin, and may be complicated by congenital or secondary cholesteatoma. Patients present with conductive hearing loss, microtia or hypoplastic pinna is a common association. The outer and middle ear are embryologically separate from the inner hence, associated inner ear anomaly is rare. On imaging, the EAC can demonstrate various degrees of bony or membranous atresia, with absence or dysplasia of the tympanic segment of the temporal bone. In congenital bony atresia, there is a bony plate at the level of the tympanic membrane, with variable EAC pneumatization. The malleus and incus may be fused to the bony plate (Fig. 3.31.1). Treatment includes the use of bone-anchored hearing aids although operative intervention is sometimes required. Preoperative imaging with HRCT is important to exclude associated cholesteatoma or to look for aberrant facial nerve course, vascular structures to facilitate surgical planning. First branchial cleft anomalies are rare (∼7%) and arise along the embryologic tract of the first branchial cleft, from the tragus (upper end opening) to the angle of the mandible (lower end opening). They include cysts, sinuses and fistulas, typically present within or near the parotid gland or EAC. Also they can present as a recurrent abscess in the preauricular skin. CT and MR imaging findings show a cystic structure or soft-tissue tract in the peri-parotid region, usually with a visible connection to the EAC, shows variable degree of enhancement related to infection or inflammation, difficult to distinguish from cystic parotid masses if a tract to EAC is not seen. Preauricular sinuses can be complex and have a variable relationship to the facial nerve; therefore, preoperative MRI is required for further assessment. Sinograms also can be done. First branchial cleft cysts can respond rapidly to antibiotic treatment. Surgical excision is curative. Cerumen is the most commonly seen ‘lesion’ within the EAC on imaging and can be a source of conductive hearing loss when impacted. It is composed of sebaceous and ceruminous secretions, desquamated skin, bacteria, and depilated hair, and it serves to clean, lubricate, and protect the ear. On imaging seen as a soft tissue nonadherent to the EAC wall with a surrounding rim of air, central focus of gas, a strand-like appearance, and characteristic changes in appearance on consecutive studies. Aggressive soft-tissue lesions isolated to the EAC can mimic cerumen, and features, such as nondependent adherence to the EAC wall or infiltrative behaviour, can help differentiate. Benign tumors isolated to the EAC are rare. They include vascular (e.g., hemangioma, vascular malformation), skin and glandular (e.g., nevus, cylindroma, epidermoid cyst), minor salivary gland (e.g., pleomorphic adenoma), and neuronal (e.g., schwannoma). These lesions have typically smooth margins and lack soft tissue edema or bone erosion, hence the need for otoscopy for diagnosis. Imaging is vital to exclude invasion by masses that obstruct the EAC and thus limit clinical evaluation. The treatment is surgical excision, typically via sleeve resection. Ceruminoma, or ceruminous adenoma, is a benign neoplasm of ceruminous glands that occurs only in the EAC. Imaging features are nonspecific however determination of the extent of these lesions is important as they are considered potentially malignant and thus should be managed more aggressively than purely benign lesions with wide local excision and, potentially, radiation therapy. Malignant ceruminomas can potentially erode bone. Superficial angiomyxomas are rare, benign tumours. They form part of Carney’s complex and occasionally affect the EAC in isolation with a polypoid mass occluding the canal and causing deafness. Show no specific imaging findings although avid contrast enhancement is seen due to its vascular nature. Keratosis obturans (KO) is an abnormal accumulation of desquamated keratin with chronic inflammation of subepithelial tissues thereby leading to occlusion and expansion of the bony portion of the EAC. KO is usually seen in younger patients less than 40 years old and can be bilateral in upto 50 per cent of patients. Clinically these patients present with conductive hearing loss due to occlusion of EAC and severe acute otalgia. KOs is the most important differential diagnosis for EAC cholesteatoma as the treatment is different for both. KO is more common than primary EAC cholesteatoma. On imaging seen as a bilateral, circumferential soft-tissue within EAC (rather than localized in EAC cholesteatoma) with a thickened tympanic membrane (which is normal in EAC cholesteatoma) causing its expansion and without bone erosion thus differentiating it from cholesteatoma; Whereas permeatal or mastoid surgery is typically required for EAC cholesteatoma, a less invasive approach can be adopted for KO (often life-long micro-suctioning of debris) (Fig. 3.31.2).
3.31: External ear
Introduction
Embryology
Congenital abnormalities
EAC atresia
First branchial anomalies
Benign: Nonaggressive (soft tissue abnormality without bone erosion)
Cerumen
Benign tumors
Angiomyxoma
Keratosis obturans
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree