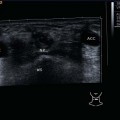
7 Extracranial Nerves The extracranial nerves are only partly accessible to ultrasonography. The only cranial nerve regularly displayed on ultrasound imaging is the vagal nerve, the cervical part of which can be easily identified between the carotid artery and the internal jugular vein (Figs. 7.1, 7.2). It descends from the skull base along the lateral wall of the internal carotid artery; after the division of the common carotid artery it runs in the caudal cervical part between the internal jugular and the common carotid artery. As a general rule, the components of the brachial plexus can be seen in level V. They are located laterally to the anterior scalene muscle and appear as hypoechoic oval structures as they are displayed obliquely cut (Fig. 7.3). Therefore, they should not be confused with lymph nodes lying in groups. Ultrasound visualization of the brachial plexus is increasingly used in plexus anesthesia. There are no definite landmarks to facilitate the positive identification of the other cranial nerves, such as the hypoglossal, facial, and accessory nerves. It is therefore not possible to classify them in relation to a pathological process in the vicinity. In thin people or in patients whose anatomy has been altered by surgery, it is possible to see the spinal cord within the spinal canal in the transverse and longitudinal views of the spine ( The clinical picture of carotidynia, a painful syndrome in the neck with tenderness over the carotid bifurcation, is rare. Despite controversy over the existence of this syndrome, changes are often seen on ultrasound examination when the relevant clinical symptoms and signs are present. At the carotid bulb, the maximum site of local tenderness, patients exhibit a hypoechoic thickening of the carotid artery wall, sometimes in two layers of the wall. This causes a slight narrowing of the lumen and leads to a pronounced outward enlargement of the vessel (Fig. 7.4). Paragangliomas are neuroendocrine tumors that arise from extra-adrenal paraganglionic cells of the autonomic nervous system. In the neck, they can be found in the region of the infra- and supralaryngeal ganglia, along the path of the vagus and carotids, as well as beyond ultrasound access in the jugulotympanic area. In B-mode, carotid paragangliomas found in the bifurcation appear as an oval tumor, oval structures with smooth outlines (Fig. 7.5). The echotexture is inhomogeneously hypoechoic with internal reflections of greater echogenicity (Fig. 7.6). The main ultrasound feature of cervical paragangliomas is the marked hyperperfusion regularly seen in color-coded duplex sonography (CCDS) (Fig. 7.7; Afferent arteries (feeders) branch offfrom the internal and external carotid arteries into the lesion ( Pearls and Pitfalls If a lesion consistent with a paraganglioma is seen on ultrasound examination, the carotid bifurcation on the other side must be looked at very carefully. Bilateral and multilocular tumors have been reported in 3%–26% of cases. Further imaging by PET scanning may be required. The two main entities in this rare class of tumor are neurofibromas and schwannomas. Both of these neurogenic tumors regularly show distal acoustic enhancement, helping to distinguish them from lymph nodes in the individual case. Neurofibromas are nonencapsulated, hypoechoic, inhomogeneous masses in the immediate vicinity of the nerves from which they arise and they may have irregular outlines (Figs 7.8, 7.9, 7.10
Anatomy
 Video 7.1).
Video 7.1).
Inflammatory Changes
Benign Tumors
Paragangliomas
 Videos 7.2, 7.3). This extreme vascularity goes by the graphic description of color/ power Doppler “inferno.”
Videos 7.2, 7.3). This extreme vascularity goes by the graphic description of color/ power Doppler “inferno.”
 Video 7.4). On sonographic palpation, the forceful pulsations are often perceptibly transmitted to the transducer.
Video 7.4). On sonographic palpation, the forceful pulsations are often perceptibly transmitted to the transducer.
Neuromas
![]()
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree