5 Thyroid Gland Diseases of the thyroid gland are common. One epidemiological study (Schilddrüsen-Initiative Papillon) showed that 37.6% of women and 40.3% of men in Germany had a goiter and/or thyroid nodules. Given the high prevalence of thyroid disease a rational approach to the various diagnostic tools (laboratory tests, ultrasonography, and scintigraphy) is essential (Table 5.1). Ultrasonography of the thyroid gland is simple and inexpensive, does not involve exposure to ionizing radiation, and provides valuable information. Ultrasonography is the mainstay of diagnostic imaging of the thyroid gland: the superficial lie of the gland means that its size, shape, fine structure, and vascularity can be demonstrated using high-frequency probes (linear array transducer, 7.5–15 MHz) with excellent and unique axial and lateral image resolution (<1 mm). At present, MRI and CT scans do not achieve such high resolution and are usually omitted in the diagnostic work-up (except for retrosternal goiter). In addition to B-scan, color Doppler imaging provides useful information on thyroid perfusion, which is helpful in the differential diagnosis of inflammatory diseases of the thyroid gland and thyroid nodules. Basic diagnostic work-up of suspected thyroid disease includes hormone testing (basal TSH, T3, and T4) and high-frequency ultrasound (B-scan, color Doppler). New ultrasound techniques: • Contrast-enhanced ultrasound has evolved over the last 10 years to become a keystone technique in abdominal ultrasound (e.g., in the differential diagnosis of liver lesions). The use of contrast agents with high-frequency probes was a technical challenge until recently, so that studies on the clinical value of contrast-enhanced ultrasound in thyroid disease are still limited. Compared with color Doppler imaging, contrast-enhanced ultrasound can visualize microperfusion of thyroid parenchyma and nodules in real time with very high resolution. Apart from scientific research questions, contrast-enhanced ultrasound of the thyroid gland might be of practical relevance in individual cases, for example in assessing the success of percutaneous ethanol injection therapy (PEIT) for autonomous thyroid nodules. • Elastography provides additional information on tissue elasticity during the ultrasound examination. Although elastography has gained clinical relevance in the diagnosis of parenchymal liver diseases (noninvasive diagnosis of hepatic cirrhosis) and the differential diagnosis of tumors (breast, prostate), its value in the diagnostic investigation of the thyroid has not been sufficiently evaluated. Preliminary studies show that the hardness of thyroid nodules can be measured with elastography, which may be helpful in differentiating benign from malignant nodules. Malignant thyroid nodules are usually hard (with the exception of follicular cancer), although this measurement has its limitations with false-positive elastographic results from calcified benign nodules. Table 5.1 Diagnostic work-up of thyroid disease
• Palpation |
• Hormone tests including thyroid antibodies |
• Ultrasonography (B-scan, color Doppler, fine-needle aspiration biopsy) |
• Scintigraphy |
• Rarely: radiography— thoracic inlet views and barium swallow |
• Rarely: CT and MRI |
Topographic Anatomy
The thyroid gland, which weighs 14–18 g, is located superficially in the anterior lower neck. Its two lobes lie on either side of the trachea and are joined by a thin bridge of parenchymal tissue (the isthmus), giving the gland a butterfly shape. Children and adolescents, and ~10% of adults, may also have a pyramidal lobe (a remnant of the thyroglossal duct left after the embryonic development of the thyroid gland from the base of the tongue), which extends in a cranial direction from the isthmus. The thyroid gland is surrounded by muscles. The sternothyroid and sternohyoid muscles lie anterior to the thyroid, the sternocleidomastoid muscle is anteromedial to the gland. The longus colli muscle is located posterior and the scalene group posterolateral to the thyroid gland. The esophagus runs behind the trachea and the left lobe of the thyroid gland. The internal jugular vein and common carotid artery are located lateral to the gland. Blood supply of the thyroid gland is provided by two thyroid arteries (branches of the external carotid artery), which run to the upper and lower pole of the thyroid (superior thyroid artery and inferior thyroid artery). Venous drainage is via the capsular venous plexus and superior, middle, and inferior thyroid veins into the internal jugular vein.
Ultrasound Examination
The examination is best performed with the patient reclining the neck to give a better view of the retrosternal parts of the thyroid and of the region of the inferior parathyroid glands. Systematic examination of the thyroid gland starts in the transverse plane anteriorly in the lower third of the neck. Imaging in the transverse plane provides an axial view of the thyroid gland and the thyroid compartment.
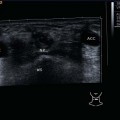
Figure 5.1 is a panoramic view of both lobes and the isthmus of the thyroid gland in the transverse plane, showing their positional relationship to the muscles and vessels. The central acoustic shadow, which is caused by the tracheal cartilage, serves for orientation and to identify the lobes of the thyroid lying lateral.
The curve of the neck usually makes it impossible to see both lobes of the gland completely at the same time in the anterior transverse view. The ultrasound probe therefore has to be moved lateral to the right and the left part, and the two lobes are scanned separately in transverse and longitudinal images. Care should be taken in this to adjust the B-mode gain correctly. Subcutaneous fat appears hypoechoic. The echogenic texture of the normal thyroid parenchyma should be hyperechoic relative to the muscles, and the vessels appear anechoic when the scanner settings are correct.
Normal Sonographic Findings
The normal thyroid gland has a smooth contour; the echo pattern of the parenchyma is homogeneous and hyperechoic compared with the surrounding muscles.
In the longitudinal plane, the craniocaudal longitudinal diameter is measured from the upper to the lower pole; in the transverse plane, the maximum width and depth diameters are determined (Figs. 5.2, 5.3).
The two thyroid lobes are measured separately. Their volumes are calculated and added together. The normal range for the total thyroid volume in adults is 8–18 mL for women and 9–25 mL for men (Table 5.2). Although the isthmus is not taken into consideration when calculating the volume, it must be examined just as carefully as the rest of the thyroid parenchyma. A thyroid volume of less than 6 mL in an adult may be associated with reduced function. Hormone status has to be assessed, and in case of low levels of T3/T4 replacement therapy might be necessary.
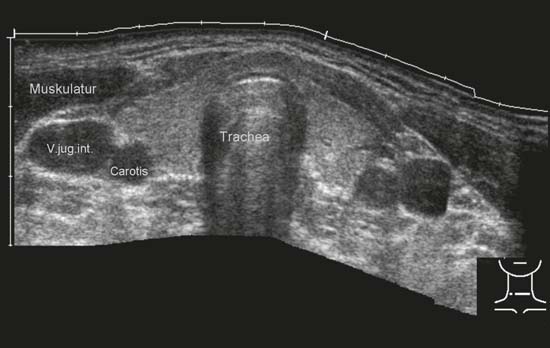
Fig. 5.1 Axial view of the thyroid gland and the thyroid compartment.
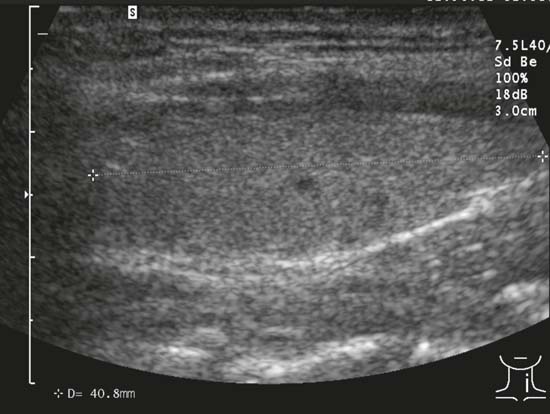
Fig. 5.2 Measurement of the craniocaudal longitudinal diameter in the longitudinal plane.
Table 5.2 Reference ranges of thyroid volumes; normal values
Age | Volume |
1–4 years | <4 mL |
6–10 years | 5–9 mL |
11–14 years | 10–15 mL |
15–16 years | <16 mL |
Women | <18 mL |
Men | <25 mL |
Sonographic measurement of the thyroid volume:
Mathematical formula of an ellipsoid (Brunn’s rotational ellipsoid):
length (cm) × width (cm) × depth (cm) × 0.479 = volume (mL)
In addition to the size of the gland, the systematic ultrasound examination includes shape (horseshoe-shaped in cross-section), contours (smooth), echogenic texture (fine, homogeneous individual echoes, hyperechoic in relation to the surrounding muscles), and movement on swallowing. Color Doppler sonography complements the B-mode real-time assessment of the thyroid. In the longitudinal view, the superior and inferior thyroid arteries can usually be found at the cranial and caudal poles of the thyroid gland. Color Doppler scans also reveal regular small vascular segments within the gland itself. Inflammatory changes in the gland may cause a marked increase in vascularity, particularly in Graves disease (as described below). Intrinsic vascularity of autonomous adenomas is an indicator of increased functional activity, while regressive nodules usually show only perinodular flow.
Pearls and Pitfalls
If the ultrasound findings are normal and the TSH is in the normal range, clinically relevant thyroid disease can almost certainly be ruled out.

Fig. 5.3 Measurement of the maximum width and depth dimensions in the transverse plane.
Ultrasound Pathology of Diffuse Thyroid Disease
Congenital Malformations
In the case of congenital hypothyroidism, ultrasound scanning can differentiate a malformation (agenesis or hypoplasia) from a diffusely enlarged thyroid gland. If there is congenital hypoplasia or aplasia of one lobe of the thyroid, the contralateral lobe is hypertrophied. Thyroid gland scintigraphy is the method of choice to demonstrate ectopic thyroid tissue (lingual goiter, intrathoracic goiter).
Goiter (Diffuse, Nodular)
A goiter is defined as an enlargement of the gland. Goiter is a common disease with a prevalence of 20%–30% in Germany. The main cause is a dietary iodine deficiency, although rare causes include inflammation and tumors. A diffuse goiter is a globally enlarged thyroid gland with smooth contours (Fig. 5.4).
If nodules can be demonstrated in the enlarged thyroid gland, it is referred to as a nodular goiter. There is a spectrum from a single nodule in an enlarged gland (uninodular goiter) through to a goiter with multiple nodules (multinodular goiter). The increasing replacement of normal tissue by nodules gives rise to irregular contours and a fuller shape (Fig. 5.5).
The lower pole of an extremely enlarged thyroid might no longer be depicted. Parts of the thyroid gland behind the clavicles or sternum cannot be assessed with ultrasound (retrosternal goiter). As a precise determination of the volume is no longer possible in this situation, the examiner has to be content with describing the findings and measuring the maximum sagittal diameters of the right and left lobes. Thyroid function cannot really be deduced from the size of the gland. Even with a small gland the patient may be euthyroid if sufficient hormone is being produced by ectopic tissue (e.g., lingual goiter). On the other hand, a patient with a greatly enlarged thyroid gland may be hypothyroid.
Tables 5.3 and 5.4 summarize the differential diagnosis of thyroid gland enlargement and clinical work-up of goiter.
Thyroiditis
Pearls and Pitfalls
The finding of a hypoechoic thyroid gland on ultrasonography is common to all inflammatory thyroid diseases.
During inflammation the thyroid gland’s normal hyperechoic echotexture (in comparison with muscle) becomes diffuse hypoechoic (Fig. 5.6). The internal echoes of the thyroid gland with inflammatory changes may be homogeneous or inhomogeneous—the ill-defined hypoechoic areas correspond to the inflammatory foci (Fig. 5.7).
The finding of a hypoechoic gland may be due to several different inflammatory conditions; the most common are Hashimoto thyroiditis, Graves disease, de Quervain thyroiditis, and postpartum thyroiditis (Table 5.5). Thyroiditis due to medication or irradiation is also possible. Acute thyroiditis occurs very rarely in immunosuppressed patients or by hematogenous spread in sepsis.
A distinction between these inflammatory conditions is not possible on the basis of B-mode scans alone. Color Doppler imaging may provide additional information on the differential diagnosis, as extreme hypervascularity of a greatly enlarged thyroid gland (vascular inferno) is usually seen in Graves disease (Fig. 5.8).
Hashimoto thyroiditis (Fig. 5.9) and de Quervain thyroiditis are less markedly hypervascular. With de Quervain thyroiditis there is local tenderness, and the hypoechoic areas are less rounded and tend to be confluent. Differentiation between Hashimoto thyroiditis, Graves disease, and de Quervain thyroiditis is based primarily on the clinical picture and laboratory tests with the determination of antibodies. Scintigraphy in the diagnosis or differential diagnosis of thyroiditis is now considered obsolete.
Graves disease is an autoimmune thyroiditis with hyperthyroidism. Clinically, exophthalmos caused by endocrine orbitopathy may be identifiable. Laboratory tests show hyperthyroidism with an increase in free T3 and T4 levels with low suppressed TSH levels. TSH receptor antibodies (TSH-R Ab) may also lead to thyroid enlargement (goiter) through a TSH-like effect, and can be detected in 90% of patients with Graves disease. Besides the increased parenchymal hypervascularity of Graves disease (Fig. 5.8), color Doppler sonography also shows an increased peak flow rate in the superior and inferior thyroid arteries.

Fig. 5.4 Diffuse goiter.
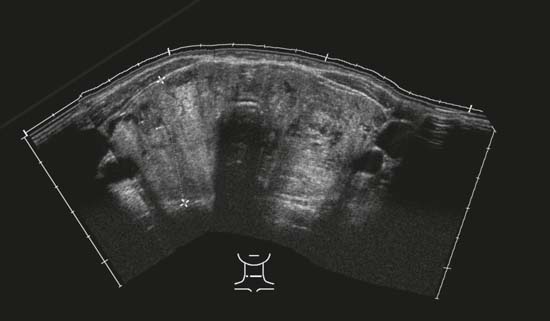
Fig. 5.5 Nodular goiter.
Table 5.3 Differential diagnosis of thyroid gland enlargement
• Goiter with or without nodules |
• Thyroiditis (autoimmune, postpartum, subacute thyroiditis, de Quervain) |
• Amyloidosis |
• Circumscribed enlargement. Differential diagnosis: tumor |
Subacute de Quervain thyroiditis is probably triggered by a viral infection of the thyroid gland and characterized clinically by the symptoms of a viral infection (fever) with localized pain and local tenderness. In addition to the standard inflammatory markers (raised erythrocyte sedimentation rates [ESR], elevated C-reactive protein [CRP]), transient hyper- or hypothyroidism is found in 50% of those affected. The ultrasound images usually show an enlarged, ill-defined thyroid gland with well-demarcated hypoechoic areas that may be confluent (Fig. 5.10).
The diagnosis is usually made on a clinical basis and confirmed with B-mode scans. In cases that are not absolutely clear, ultrasound-guided fine-needle aspiration may provide the evidence of giant cells and histiocytes that is needed to diagnose de Quervain thyroiditis.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree