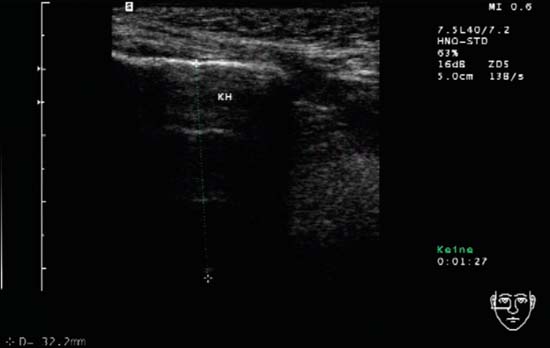
11 Paranasal Sinuses and Midface Ultrasonography offers a rapid, safe, first-line assessment and is also useful for a preliminary evaluation in cases of trauma. Exposure to ionizing radiation from X-rays can be avoided in both children and pregnant women. A-mode (amplitude modulation in ultrasound) scanning was previously regularly used. It represents the time required for the ultrasound signal to hit a tissue interface and return the signal to the transducer; the greater the reflection at the tissue interface, the larger the signal amplitude on the screen. However, this mode has been increasingly superseded by B-scan imaging, which has become widely available. The superficial frontal and maxillary sinuses are usually accessible. The eyeball can be used as a fluid-filled medium that enables the visualization of structures lying behind it as the ethmoid cells and orbit. Of course, normal and pathological structures within the eyeball are also accessible ( Ultrasonography of the nose and sinuses has a few distinct features in comparison with soft-tissue imaging of the neck. Physically, ultrasound waves traverse the anatomical target area (air-filled spaces surrounded by bone) to only a limited extent. In normal maxillary and frontal sinuses, the layers of the cutis (8–10 mm) and the transition from skin to anterior wall of the sinus can be seen, behind which there is usually a total reflection. Assessment is possible only in the case of pathological conditions, which allow the “posterior wall echoes” to be seen. This usually occurs at a depth of about 40 mm in the maxillary sinus and of 20 mm in the frontal sinus. The examination of the paranasal sinuses is best carried out with the upper body upright. Additional head positions with hyperextension and anteflexion of the neck may distinguish fluid or effusion from other pathological conditions. Examination of the maxillary and frontal sinuses is always performed in the transverse and longitudinal planes. It is particularly important to make a comparison of the findings on the right and left side. The starting point of a maxillary sinus examination is at the level of the infraorbital nerve; the frontal sinus examination starts with the transducer position between the eyebrows. Insonation frequency (as low as possible), penetration depth (± 60 mm), and gain (high) should be adjusted beforehand (Fig. 11.1). As mentioned above, ultrasound wave transmission in the depths of the sinuses is possible in the presence of an inflammatory process with secretions and mucosal swelling within the lumen of a paranasal sinus (sinusitis). If the entire sinus cavity being examined is filled (with pus or mucus) by such a process, the sound is not completely reflected at the anterior wall but is transmitted further to the posterior wall, where it is once again reflected to give a visible “posterior wall echo.” The posterior wall of the maxillary sinus has a U- or V-shaped configuration. Depending on the viscosity of the process inside the lumen it appears hypoechoic to anechoic with sparse isolated internal echoes (Figs. 11.2, 11.3). Fluid secretions, if not filling the lumen completely, may become visible by anteflecting the head, and disappear after reclination. Cysts and mucoceles lying against the anterior wall may be seen as rounded space-occupying lesions (Figs. 11.4, 11.5, 11.6, 11.7). In the case of an acute exacerbated inflammatory process, destruction of osseous structures is possible and consecutive swelling of neighbouring soft tissue is observed. Structures lying behind air-filled areas are not visible. An isolated process at the posterior wall of the air-filled sinus will escape detection. Benign tumors of the paranasal sinuses, such as mycetomas and adenomas, are visible on ultrasound images only in isolated cases and are sometimes difficult to distinguish from inflammatory changes Fig. 11.1 Maxilla, right, transverse. The ultrasound probe is held in the transverse plane beneath the orbit; the image shows the typical normal findings. The first echogenic band can be seen at a depth of 1 cm and forms the border between the anterior maxillary sinus wall and the soft tissue layer. Equidistant below this, but less extensive, are other echogenic reflexes (caliper) in the maxillary sinus (KH). These reflexes are artifacts and are generated by multiple-reflection echoes. They should not be confused with a posterior wall echo.
Anatomy
 Video 11.1).
Video 11.1).
Inflammatory Changes
Sinusitis
Benign Tumors
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree