(1)
Department of Radiology, John H Stroger Jr Hospital of Cook County, Chicago, IL, USA
Infection
Diagnosis
Pelvic Inflammatory Disease (Infection of the Upper Female Genital Tract: Endometrium, Fallopian Tubes, and Ovaries)
Imaging Features
Salpingitis, pyosalpinx, tubo-ovarian abscess, and endometritis
Early:
1.
Mild pelvic edema with haziness of the pelvic fat and thickening of the uterosacral ligaments.
2.
Salpingitis—inflammatory thickening, enhancing fallopian tubes which are not dilated.
3.
Oophoritis—enlarged ovaries with indistinct contours and periovarian fluid or polycystic appearance.
4.
Endometritis—thick hypoechoic endometrium with increased vascularity by US. CT also shows thick endometrium with increased enhancement.
Advanced:
1.
Pyosalpinx—distention of obstructed fallopian tubes with echogenic fluid by US and enhancing walls by CT.
2.
Tubo-ovarian and pelvic abscess—thick-walled solid-cystic mass, septations, complex fluid, and rarely gas collection.
3.
Reactive changes in the adjacent sigmoid colon and small bowel with wall thickening and ileus. The ureters may be obstructed.
Diagnosis
Early PID
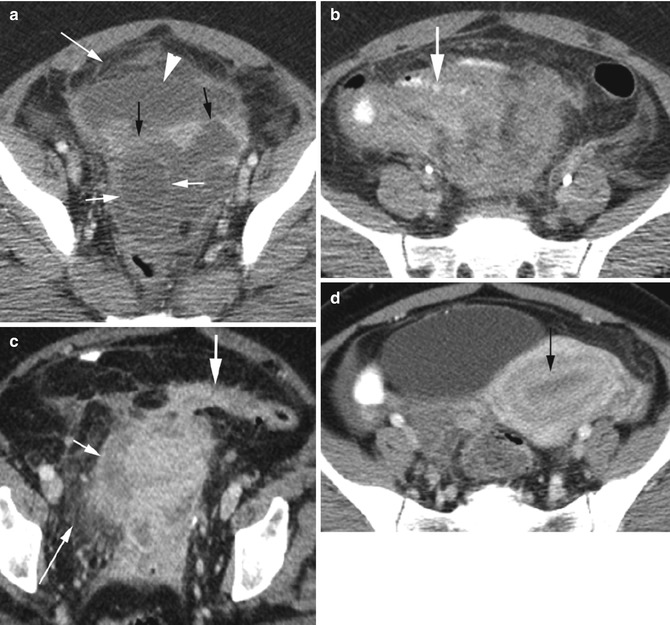
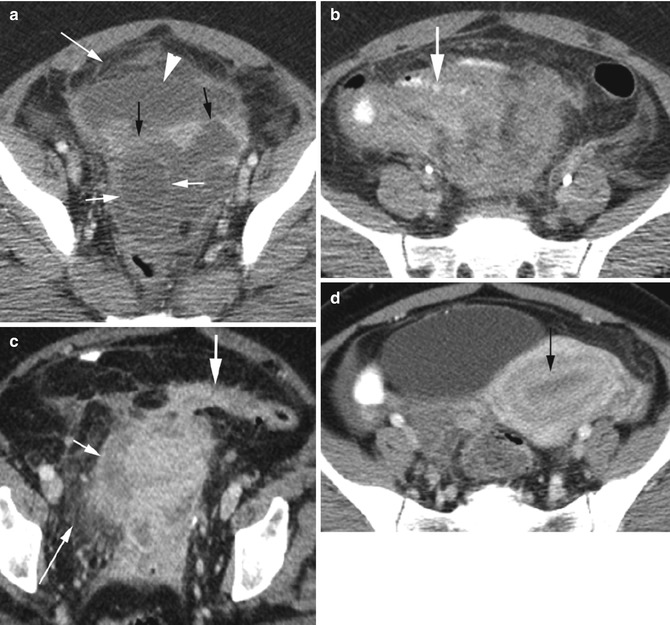
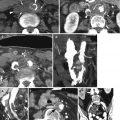
Fig. 18.1
Early pelvic inflammatory disease in different patients. Axial CT (a) shows thickening of the broad ligaments (black arrows), oophoritis of the right ovary (short white arrows) which is enlarged with indistinct borders, diffuse pelvic fluid collection (arrowhead), and diffuse haziness of pelvic fat (long white arrow). (b) Reactive wall thickening of the distal small bowel (thick arrow). (c) Reactive wall thickening of the sigmoid colon (thick arrow). Mild salpingitis as seen by dilated, thick-walled right fallopian tube (short arrow) and diffuse inflammatory changes with haziness of pelvic fat (long arrow). (d) Endometritis with thick enhancing endometrium (arrow) with simple endometrial fluid
Diagnosis
Hydrosalpinx and Pyosalpinx
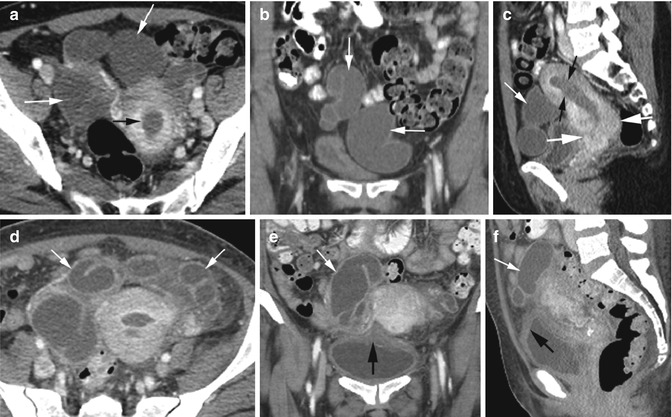
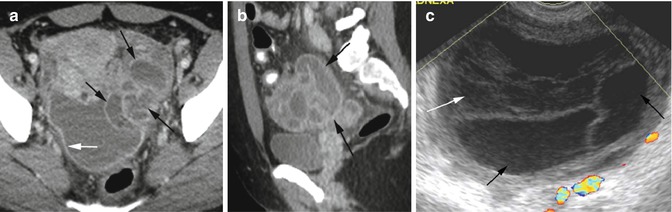
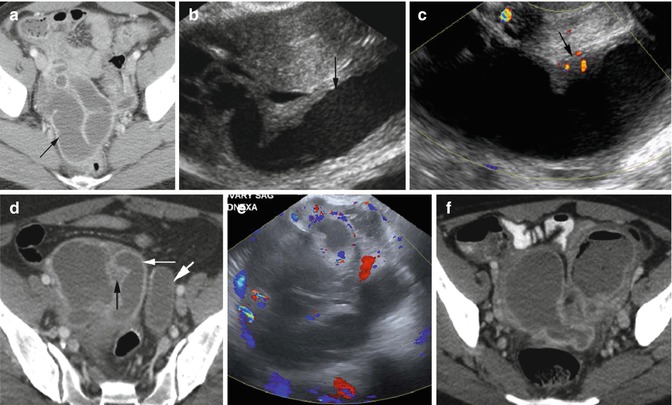
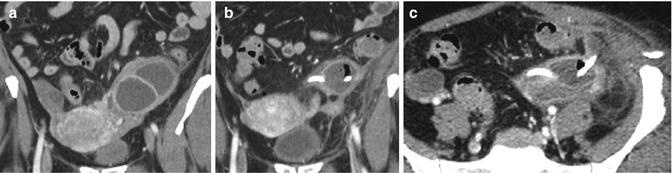
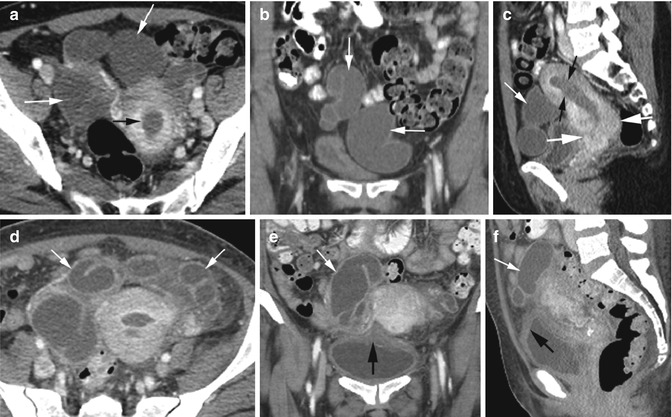
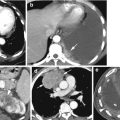
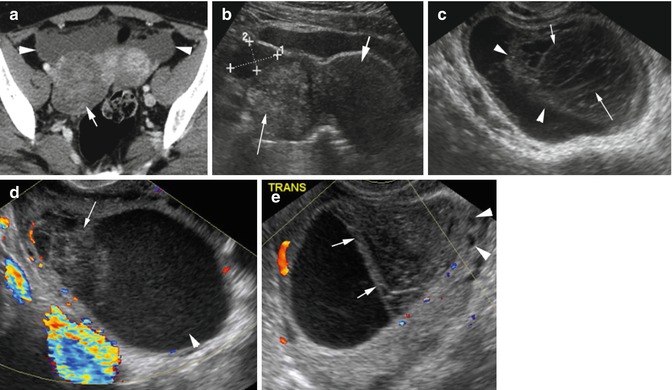
Fig. 18.2
Hydrosalpinx from chronic obstruction of the cervix by adenosquamous carcinoma. CECT (a) axial, (b) coronal, and (c) sagittal reformatted images show dilated bilateral fallopian tubes without wall thickening or enhancement (white arrows). Fluid distending the endometrial canal (black arrows) due to outlet obstruction. Soft tissue mass is identified constricting the cervical canal (thick white arrows). (d–f) Pyosalpinx with leukocytosis and clinical signs of infection following chemo- and radiation therapy of the same patient. CECT (d) axial, (e) coronal, and (f) sagittal reformatted images show PID with wall thickening of the previously seen hydrosalpinx (white arrows), diffuse increased density of pelvic adipose tissue between the fallopian tubes, and cystitis with thick-walled bladder (thick arrow)
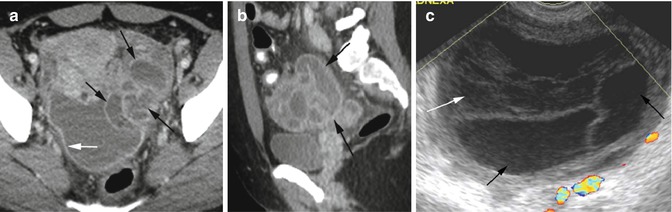
Fig. 18.3
Advanced PID with pyosalpinx and focal peritonitis. CT axial (a) and sagittal reformatted (b) images show conglomeration of the dilated left fallopian tube (black arrows) with enhancing thick wall and fluid in posterior cul-de-sac surrounded by enhancing peritoneum (white arrow). (c) Endovaginal ultrasound of the left adnexa shows dilated fallopian tube (black arrows) with adjacent echogenic fluid (white arrow) as seen in CT
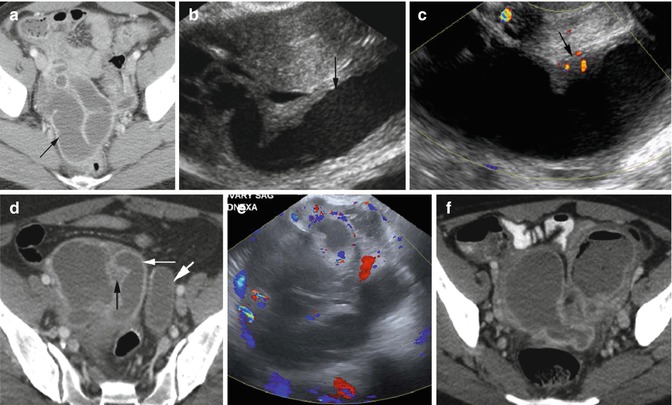
Fig. 18.4
Pyosalpinx in three patients. (a–c) First patient with gonorrhea: (a) Axial CT shows dilated right fallopian tube with thick enhancing wall (arrow). (b) Endovaginal grayscale US examination shows the right fallopian tube is distended with echogenic fluid (arrow). (c) Color Doppler study shows increase color flow within the thickened tubal wall. (d–f) Second patient with right lower quadrant pain: (d) Axial CT shows right-sided pyosalpinx with dilated thick enhancing walls (thin white arrow) and increased fat stranding (black arrow). The left fallopian tube shows hydrosalpinx (thick arrow) with no wall enhancement. (e) Color Doppler US of the right adnexa shows dilated right fallopian tube with increased flow around it. Third patient: (f) Axial CT shows bilateral pyosalpinx with gas and fluid in the left fallopian tube post chromopertubation
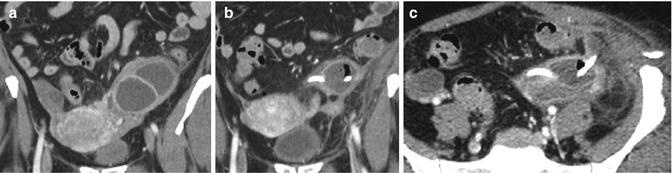
Fig. 18.5
Pyosalpinx with drain. (a) Coronal reformatted CT shows dilated thick-walled left fallopian tube. (b, c) Coronal reformatted and axial CT at a later date show insertion of drainage tube with gas within the fallopian tube
Diagnosis
TOA
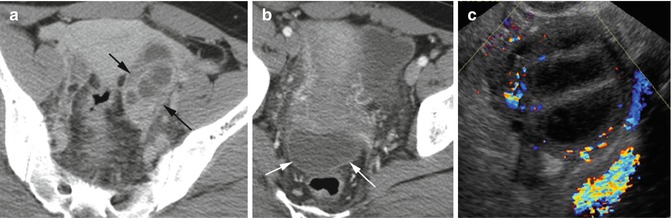
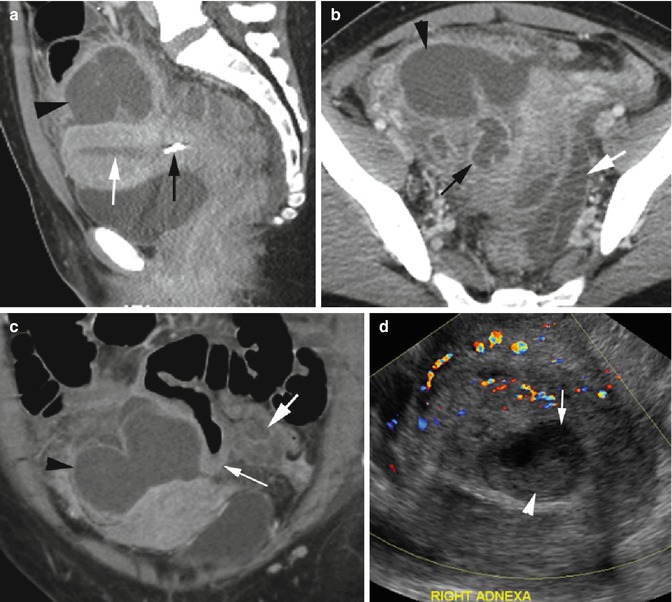
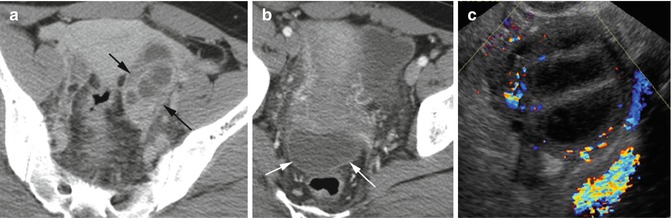
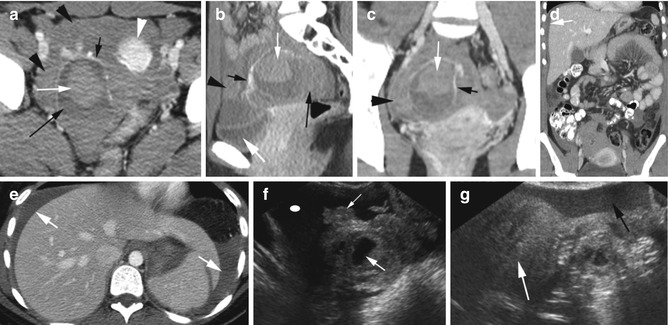
Fig. 18.6
Tubo-ovarian abscess from advanced PID. CT axial (a) shows multiple thick-walled fluid collections in the left adnexa (arrows). (b) shows posterior cul-de-sac fluid collection with enhancing peritoneum (arrows). (c) Endovaginal color Doppler US shows thick-walled cystic collection with thick septations in the left adnexa with increased vascularity
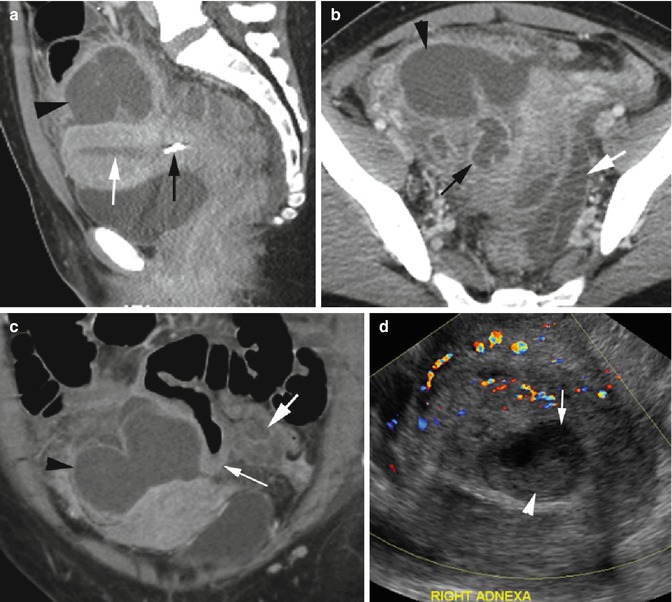
Fig. 18.7
Tubo-ovarian abscess (TOA) following IUD removal and retained fragment. (a) Sagittal reformatted CT shows a piece of retained IUD in the lower uterine segment (thin black arrow) with fluid (thin white arrow) in the endometrial cavity. (b) Axial CT shows large TOA with complex fluid collection in the right adnexa (arrowhead) surrounding the pyosalpinx (black arrow). Pyosalpinx on the left side (white arrow) is more dilated. (c) Coronal reformatted CT shows a large TOA on the right side (arrowhead) and a smaller one on the left (thick white arrow) with thick-walled small bowel (thin white arrow) in between. (d) Color Doppler ultrasound shows increased vascularity of the solid area in the right adnexa surrounding the abscess cavity (thin arrow) with echogenic debris (arrowhead)
Diagnosis
Endometritis
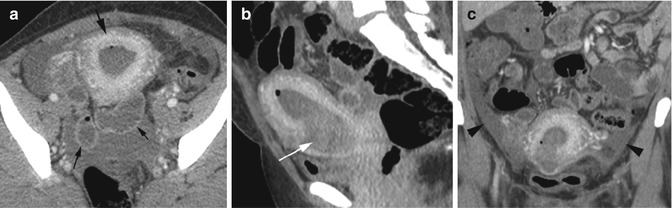
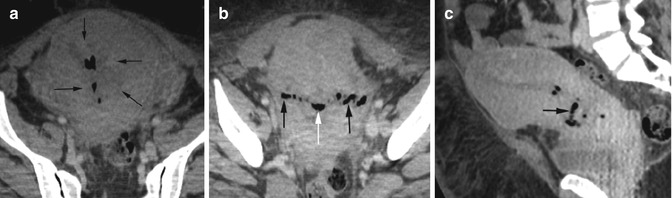
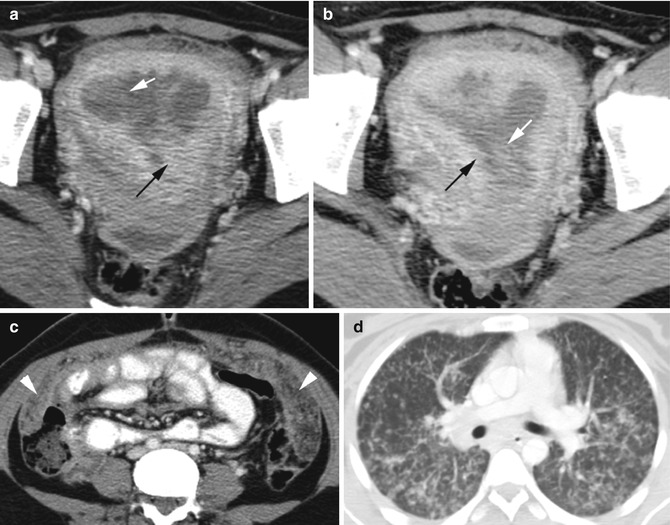
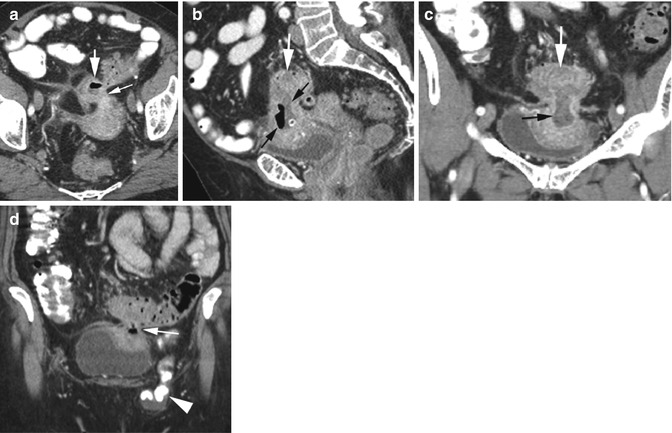
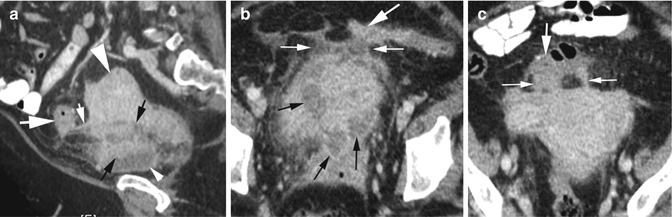
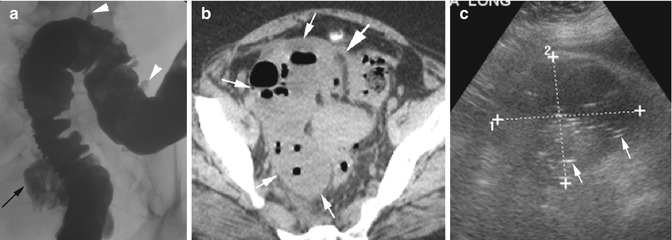
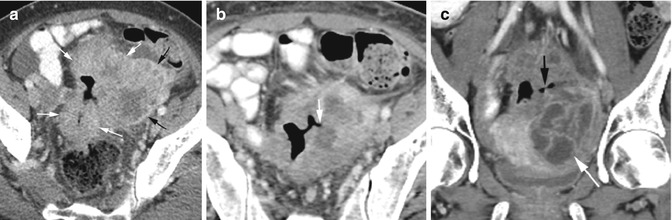
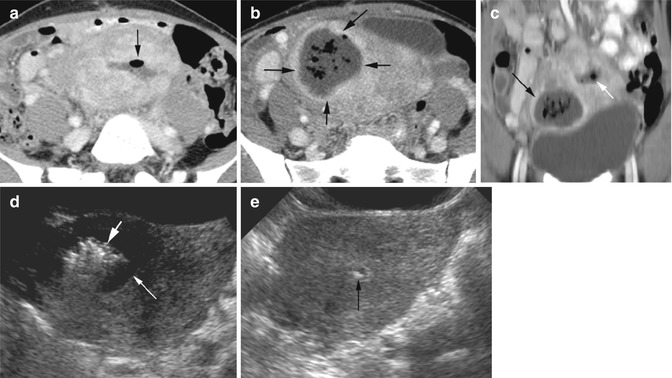
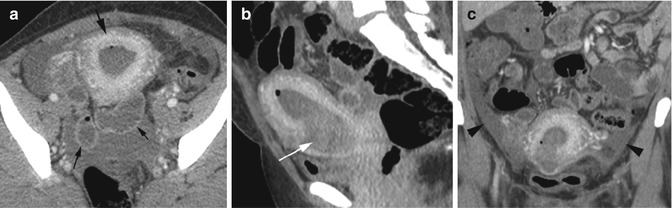
Fig. 18.8
Endometritis with septic shock post dilatation and curettage. CT axial (a), sagittal (b), and coronal (c) reformatted images show thickened avidly enhancing endometrium (thick black arrow). The endometrial cavity is distended with heterogeneous hemorrhagic fluid (white arrow) and small focus of gas. Surrounding small bowel loops show reactive ileus (thin black arrows). A small amount of ascites is seen in the lower abdomen and pelvis, but the peritoneum is not enhancing (arrowhead), indicating absence of peritonitis
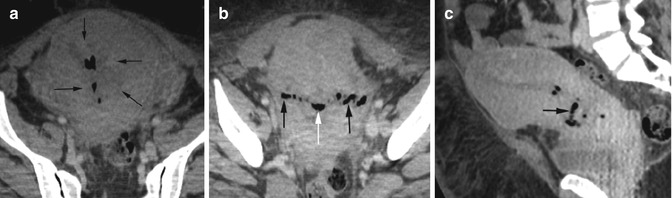
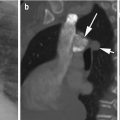
Fig. 18.9
Endometritis. Patient with chorioamnionitis had crash C-section with wound and endometrial infection following surgery. CT axial image (a) shows gas and irregular heterogeneous fluid collection in the endometrial cavity (arrows). (b) The gas linearly arranged in the surgical myometrial wound (black arrows) is continuous with endometrial gas (white arrow). Sagittal reformatted image (c) shows gas and fluid in the endometrial cavity extending to the anterior myometrium in the lower uterine segment (arrow)
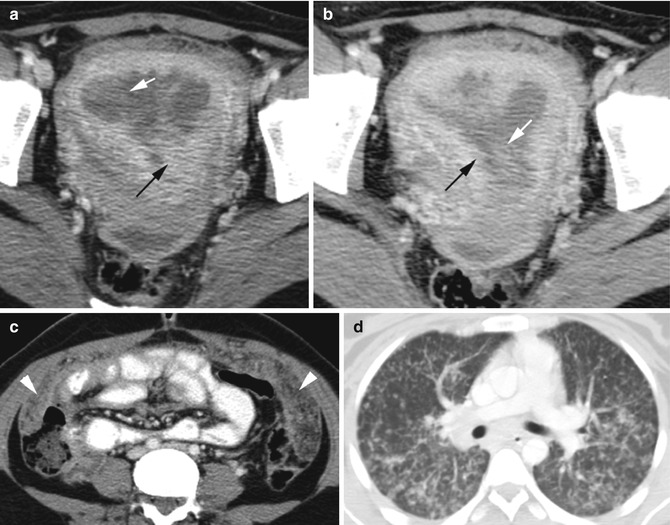
Fig. 18.10
Tuberculous endometritis: Axial CT (a, b) of uterus at different levels shows distended endometrial cavity with heterogeneous fluid (white arrow). The endometrium is thick and irregular (black arrow). (c) Axial CT in the mid-abdomen shows thick omentum with increased markings (arrowheads). (d) Lung bases show miliary TB in random distribution of nodules
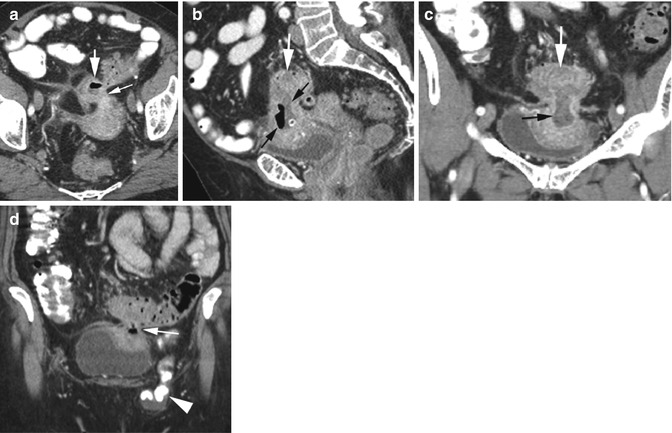
Fig. 18.11
Diverticulitis with fistula to uterus. CT axial (a), sagittal (b), and coronal (c, d) reformatted images show large fistula (thin white arrow in a, d) with fluid and gas (black arrows) extending from the sigmoid colon (thick white arrows) to the fundus of the uterus. Small bowel hernia is seen in the left inguinal canal (arrowhead in d)
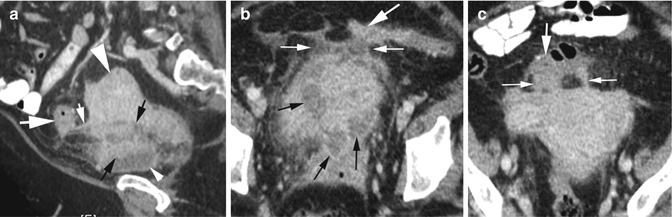
Fig. 18.12
Diverticulitis resembling PID in uterovesical pouch. Sagittal reformatted CT (a) shows a tract (thin white arrow) from the sigmoid colon (thick white arrow) into the anterior cul-de-sac, the space between the uterus (thick arrowhead) and bladder (thin arrowhead) which is filled with irregular soft tissue density and fluid (thin black arrows). (b, c) Axial CT shows the same heterogeneous multiloculated fluid collection (black arrows) in the anterior cul-de-sac. Linear tracts (thin white arrows) are again seen from the colon (thick arrow) extending inferiorly to the fundus of the uterus
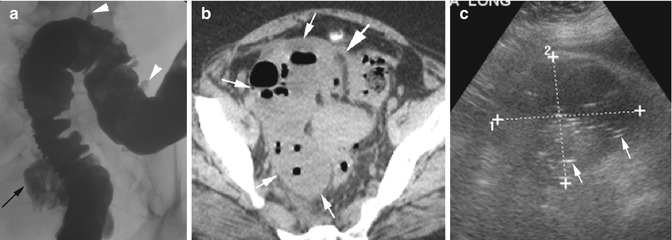
Fig. 18.13
Diverticulitis with fistulous communication with ovarian cyst. (a) Barium enema examination shows extravasation of contrast from the distal sigmoid colon (black arrow). Multiple diverticula are also present in the rest of the sigmoid colon (arrowheads). (b) Axial CT shows a large mass in the right adnexa with multiple air-fluid collections (thin arrows) with a connection to the colon (thick arrow). (c) Grayscale endovaginal US reveals a large heterogeneous mass in the right adnexa (cursors) with numerous echogenic foci of gas collection (arrows). At surgery, a 5 cm right adnexal inflammatory cystic mass replacing the ovary was seen with fistula with the sigmoid colon
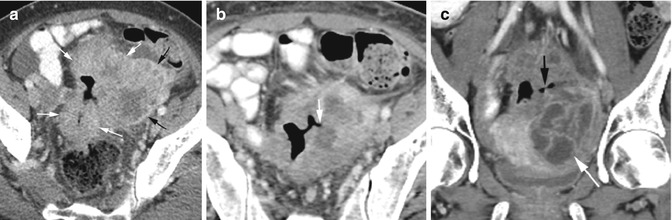
Fig. 18.14
Sigmoid cancer infiltrating to the left ovary with TOA. (a) Axial CT shows sigmoid colon cancer with wall thickening (white arrows). The sigmoid mass is extending to the left ovary (black arrows) with central necrosis and displaced follicles. (b) Axial CT shows fistulous tract to the left ovary (arrow) from the affected sigmoid colon. (c) Coronal reformatted image shows the fistula (black arrow) over the left TOA (white arrow)
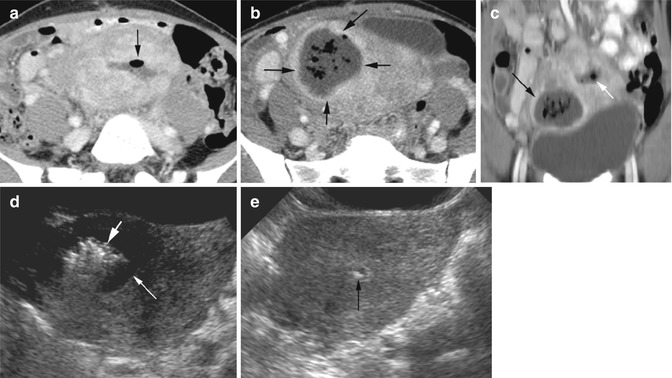
Fig. 18.15
Post-myomectomy infection and endometritis. CT (a) axial image shows fluid and gas collection in the endometrial cavity (arrow). (b) Axial image at a lower plane and (c) coronal reformatted image show a thick-walled intramural abscess with fluid and gas collection at the myomectomy site (black arrows) in the anterior body of the uterus separate from the endometrial fluid and gas (white arrow in c). Grayscale endovaginal US (d) shows intramural pocket of fluid (thin arrow) and high echogenic gas collection (thick arrow) within the uterus on the right. (f) Echogenic focus in the endometrial cavity (arrow) due to gas as seen in the CT study
Diagnosis
Hemorrhagic Ovarian Cyst
Imaging Features
US:
1.
Can appear as solid nodule with concave outer margin and with no internal vascularity
2.
Reticular pattern from fibrin strands
3.
Can have a fluid level
CT:
1.
High density within cyst, homogeneous or heterogeneous
2.
Can have hematocrit level
3.
Can rupture into the peritoneal cavity and cause hemoperitoneum
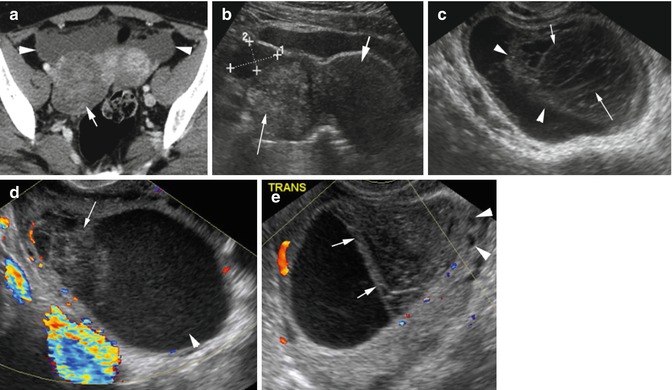
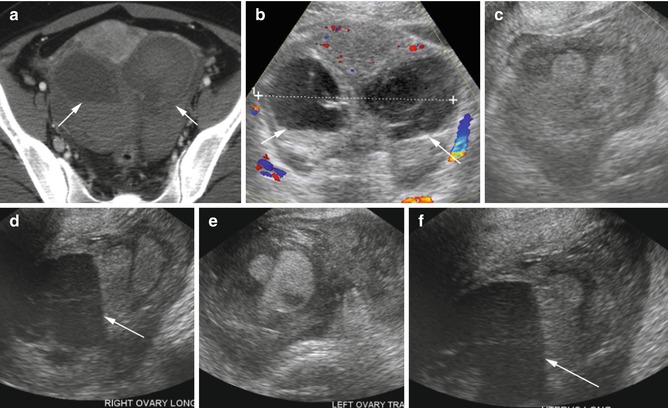
Fig. 18.16
Acute hemorrhage in the ovary in two patients with acute pelvic pain. Patient 1: (a) Axial CT shows heterogeneous density of the right ovary cyst (arrow) with small hemoperitoneum (arrowheads). (b) Transverse grayscale US is similar to the CT image. The right ovary is filled with echogenic clot (thin arrow) with small adjacent hemorrhagic fluid (cursors). The uterus (thick arrow) is less echogenic than the hemorrhage. Second patient with bilateral acute hemorrhage in ovary cysts: (c) Grayscale US shows retracted clot (arrowhead) with fibrin strands giving a lacy pattern (arrow) in the right ovary. (d) Color Doppler study shows no flow within the clot. The retracted portion has heterogeneous echogenicity (arrow) while the rest of the cyst has low echogenic hemorrhage (arrowhead). (e) The left ovary shows clot retraction with flat-free surface (arrow). The hemorrhagic cyst is displacing the follicles (arrowheads) of the rest of the ovary
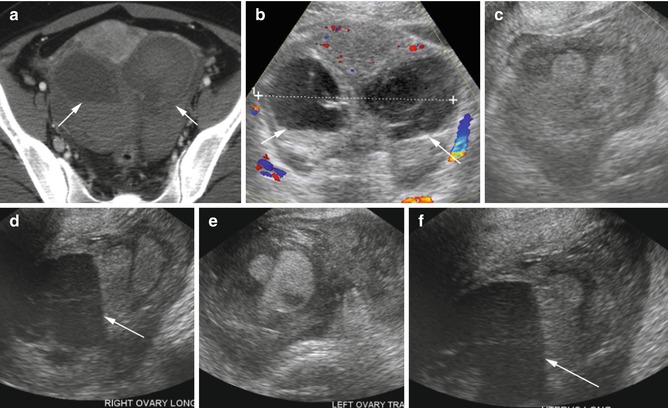
Fig. 18.17
Acute hemorrhagic ovarian cyst in a patient with systemic lupus erythematosus. (a) Axial CT image shows high-attenuating acute hemorrhagic fluid with hematocrit level in both ovaries (arrows also in b). (b) A transverse image from endovaginal sonogram shows similar findings to the CT. (c–f) Transverse and longitudinal images of the right and left ovaries, respectively, show heteroechoic hemorrhage in both ovaries with hematocrit level (arrows)
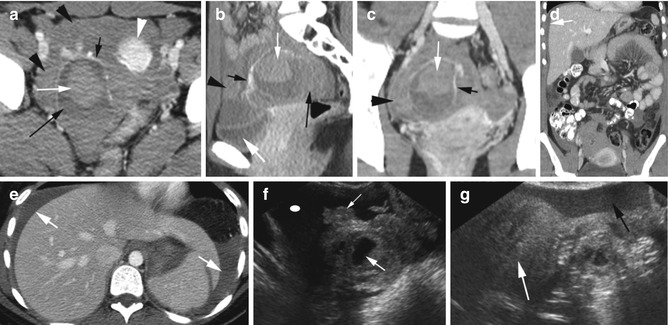
Fig. 18.18
Ruptured corpus luteum cyst in two patients. Patient 1: CT axial (a), sagittal (b), and coronal (c) reformatted views show a large corpus luteum cyst with prominent vessels on the cyst wall (short black arrow) which are continuous with the uterine artery (short black arrow in b, c). Large thrombus is within the cyst (thin white arrow) and hemorrhagic fluid posterior to the thrombus (long black arrow). Sentinel clot (black arrowheads) is surrounding the uterus (white arrowhead) and corpus luteum cyst and is of higher density than urine in the bladder (thick white arrow). Coronal reformatted (d) and axial (e) CT show hemoperitoneum in both paracolic gutters (arrows) extending to the subphrenic spaces. Patient 2: Endovaginal US (f) shows the corpus luteum cyst (thick white arrow) surrounded by echogenic thrombus (thin arrow) with peripheral sonolucent fluid (ellipse). (g) Sentinel echogenic clot (white arrow) is surrounded by low-level echogenic hemoperitoneum (black arrow)
Diagnosis
Endometrioma
Imaging Features
1.
Complex cyst with diffuse low- to medium-level internal echoes with ground-glass appearance
2.
Can have fluid/fluid or fluid-debris levels
3.
Unilocular or multilocular with thin or thick septations
4.
Can have mural irregularity and echogenic foci in the walls, rarely with internal vascularity from endometrial tissue
5.
Rarely can be anechoic, heterogeneous echogenicity or calcification
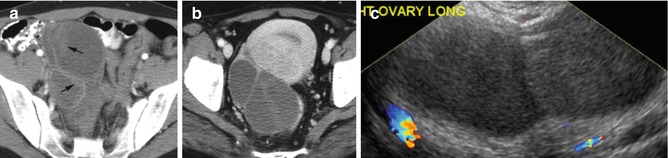
Fig. 18.19
Endometriomas in three different patients. Axial CT (a, b) shows multilocular cyst in the right adnexa with mural irregularity from adherent thrombus or fibrin in the walls (arrows in a). (c) Endovaginal US shows multilocular cyst with uniform low-level echoes
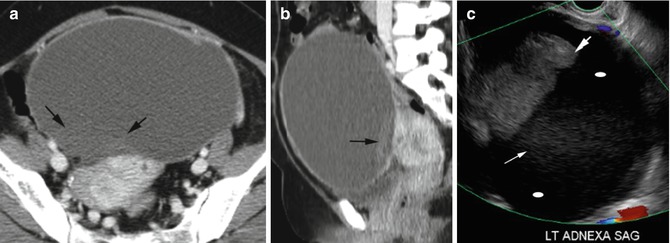
Fig. 18.20
Endometrioma with heterogenicity. CT (a) axial and (b) sagittal reformatted images show a large low-density cyst with focal-dependent higher-density (arrows) debris. (c) Endovaginal US shows complex cyst in the left adnexa with nonvascular solid area (thick arrow) like dermoid, low-level echoes (thin arrow) and anechoic regions (ellipse)
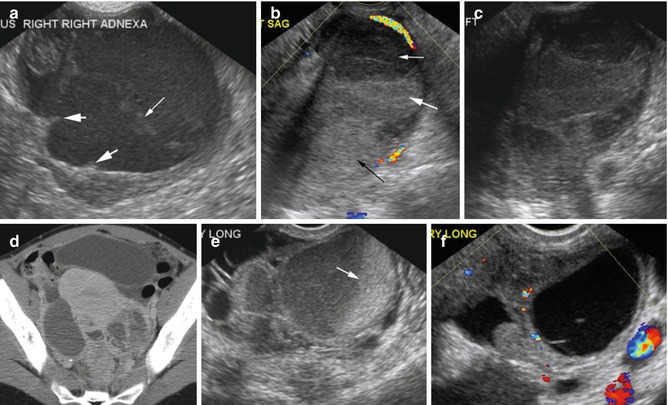
Fig. 18.21
Endometriomas. Case 1: (a) endovaginal US shows a large complex cyst with septation (thin arrow) and wall nodularity (thick arrow). Case 2: US (b–d) axial CT show multilocular left adnexal endometrioma with varying degrees of echogenicity (arrows). Case 3: endovaginal US (e, f) images show an echogenic endometrioma with fluid/fluid level in the right adnexa (arrow) and anechoic endometrioma in the left adnexa
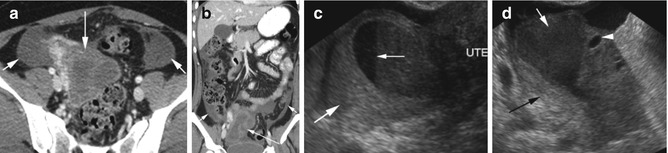
Fig. 18.22
Ruptured endometrioma. (a, b) Axial and coronal reformatted CT show multiloculated cyst of the right adnexa (long arrow) with hemoperitoneum in bilateral paracolic gutters (short arrows). Endovaginal US (c) shows fluid/fluid level in the endometrioma (thin arrow) with surrounding echogenic hemorrhage (thick arrow). (d) Low-level internal echoes in the endometrioma (white arrow) displacing follicles in the ovary to the left (arrowhead) and echogenic hemorrhage posterior to it (black arrow)
Diagnosis
Mature Teratoma or Dermoid
Imaging Features
1.
Can be purely cystic, mixed mass with components of all three germ layers, noncystic mass mainly with fatty tissue
2.
Get Clinical Tree app for offline access

US:
(a)




Cystic mass with densely echogenic mural nodule (dermoid plug) which may produce distal shadowing
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree