Fig. 28.1
(a–d) Radiographs of cam and pincer lesions. (a, b) AP (a) and lateral (b) X-rays demonstrating CAM lesion of right hip. (c, d) AP (c) and lateral (d) X-rays demonstrating periacetabular ossicle effectively creating pincer-type lesion of left hip. Also note adjacent CAM lesion on left femoral neck
A reduced femoral head–neck offset is best assessed on MRI using dedicated oblique axial images that are obtained parallel to the long axis of the femoral neck. Methods of quantitatively evaluating the femoral head–neck offset have been described with the “alpha” angle [9]. The alpha angle is calculated on the abovementioned oblique axial MR images of the hip. The angle is measured between a line drawn from the center of the femoral head through the central axis of the femoral neck and a second line drawn from the center of the femoral head to the anterior point where the distance from the center of the head exceeds the radius of the subchondral femoral head. It has been proposed that an alpha angle >55° predisposes a patient to cam FAI [9].
Pincer Impingement
Pincer impingement is caused by abnormal contact between the acetabular rim and the femoral neck as a result of acetabular abnormalities [1, 8, 10–12]. Hip joint abnormalities such as coxa profunda (deep socket), protrusio acetabula (acetabular fossa medial to the pelvic border, or acetabular retroversion (backward facing acetabular opening) can predispose patients to pincer impingement (Fig. 28.1c, d). In pincer-type impingement, during hip flexion, the femoral neck abuts against the acetabular labrum, resulting in compression and tearing of the labrum. Because pincer impingement involves often the entire acetabulum, as in protusio, damage to the femoral head can be seen in both the anterolateral femoral head as well as the posterior inferior femoral head. The bony acetabulum and pincer lesion act like a snowplow, skiving into the femoral articular cartilage as the hip is brought through a range of motion, especially hip flexion and internal rotation. Protrusio acetabuli and acetabular retroversion can be seen on oblique axial MRI of the hip. Acetabular retroversion results in an increase in coverage of the anterior aspect of the femoral head [13]. Acetabular depth can be quantified on the same oblique axial images that are used to calculate the alpha angle. The depth is calculated by drawing a line connecting the anterior and posterior acetabular rims and a parallel line that passes through the center of the femoral head. The distance between these two lines is the acetabular depth, with the value being positive if the center of the femoral head is lateral to the acetabular rim [14]. As would be expected, the acetabulum is significantly deeper in patients with pincer FAI. In patients with cam FAI, acetabular depth is often normal. Future research may recognize a specific value for the acetabular depth that puts a patient at increased risk for the development of pincer FAI.
Clinical Diagnosis
A thorough history should be taken from the patient with special attention focused on any history of trauma, childhood hip disorders, or previous surgery. The activity level of the patient can vary with respect to provocative maneuvers. Symptoms are common in activities that require repetitive hip flexion, but symptoms may also occur at rest, especially with periods of prolonged sitting. Recreational sports and exercise may also be provocative. Mechanical symptoms (popping, snapping, clicking) should be differentiated from snapping psoas syndrome or a snapping iliotibial band syndrome.
Classically, patients present with deep anterior hip or groin pain and potentially radiation of pain to the anterior thigh. Commonly, this pain is localized deep, and patients are unable to reproduce it with tactile pressure. Less commonly, patients may also present with lateral hip pain or pain radiating to the buttocks. The patient experiences hip or groin pain exacerbated by walking, prolonged sitting, or deep squatting. Mechanical symptoms, such as locking, catching, or clicking may be present but are fairly rare. Provocative testing elicits symptoms when the hip is passively flexed, adducted, and internally rotated (positive Anterior Impingement test) or flexed, abducted, and externally rotated (positive FABER test) [1, 3, 8].
Imaging Principles
As this text concerns itself with MRI and arthroscopy correlations, the cases will focus specifically on those aspects. The diagnosis of impingement, however, currently relies heavily on the clinical context, exam findings, and plain radiographic imaging. MRI findings are viewed by most expert clinicians as confirmatory of the diagnosis and as essential for ruling out alternative diagnoses.
Patients undergo a standard series of plain radiographs: Standing AP pelvis, long neck lateral view, and False profile view of the hip. The main purpose of the X-rays is to evaluate the bony structures for FAI or other mechanical deformity. X-rays can also be used to evaluate the presence of acetabular dysplasia as well as other pain producing pathology such as fractures and early degenerative joint disease. If the patient has failed conservative management and there is evidence of FAI in the absence of alternate diagnosis, we routinely order an MRI arthrogram.
Magnetic resonance imaging (MRI) and MR arthrography are excellent imaging modalities for showing the morphologic abnormalities of the proximal femur and acetabulum as well as the various changes seen in the hip secondary to FAI. The normal anatomy of the hip allows for a wide range of motion. The morphologic abnormalities that predispose a patient to the development of FAI result in decreased joint clearance between the femoral neck and acetabulum. MRI arthrograms can evaluate any evidence of abnormal contact, or impingement, between the femoral neck and acetabulum. Associated degenerative changes in the acetabular labrum and/or adjacent articular cartilage can also be evaluated simultaneously [2, 8, 15, 16].
MRI findings of changes secondary to FAI within the acetabulum can be seen involving the acetabular bone, labrum, and articular cartilage. Studies suggest that a majority of the abnormalities are located peripherally at the chondrolabral transition zone [17]. The cases that follow will illustrate these characteristic MRI and (if applicable) arthroscopy findings.
Case 1
A 34-year-old female presented with a 10-month history of anterior hip pain, which occurred acutely during a boot camp exercise class. She had been treated previously with physical therapy, activity modification, and rest for a lumbar spine etiology and piriformis syndrome. Diagnostic steroid and local anesthetic injection in the femoral-acetabular joint gave excellent short-term relief. See Figs. 28.2a, b and 28.3.
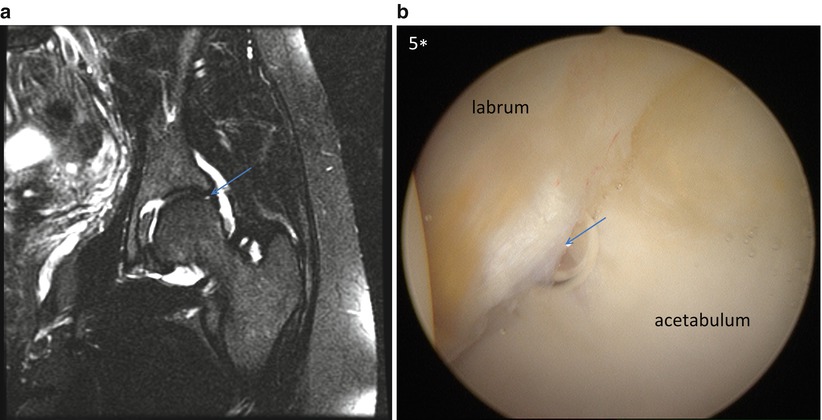
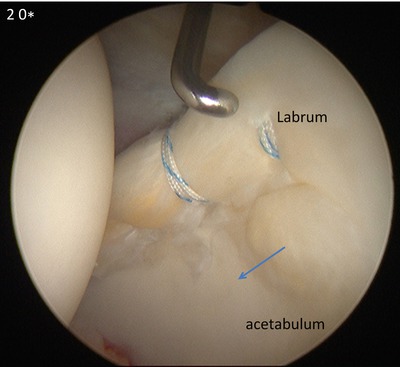
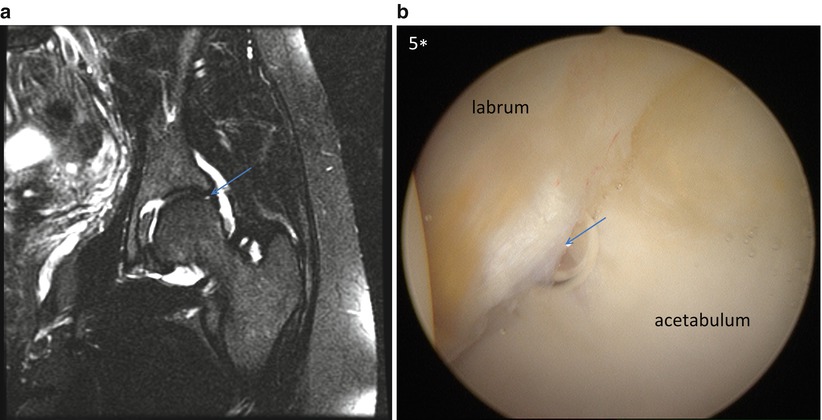
Fig. 28.2
(a, b) MRI arthrogram T2-weighted coronal image (a) demonstrating chondro-labrum separation (blue arrow) and arthroscopy image of same area (b)
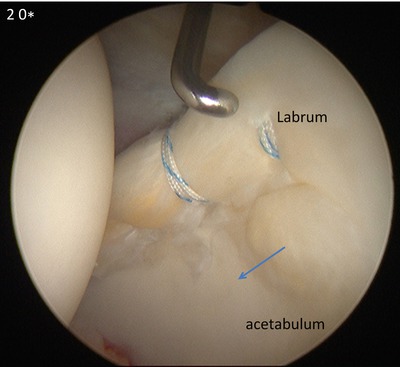
Fig. 28.3
Arthroscopy image showing repair of the labrum damage with persistent articular acetabular chondral damage due to Cam-delamination (arrow)
Discussion
This case is shown to highlight the early findings of Cam impingement in the region of shear injury at the chondro-labrum juncture in a non-arthritic patient. The articular cartilage in FAI cases can show a variety of changes. Chondral damage occurs commonly first on the acetabular side of the joint with FAI. Progression to involve the femoral head occurs only late in the degenerative process. Cartilage damage is located anterosuperiorly with cam-type FAI, due to local compression by the cam. Areas of signal hyper-intensity on MR that represent areas of chondral softening manifest early damage. Arthroscopically, this is seen as focal delamination or a “wave sign.” Eventually, this softening progresses from articular cartilage fissures to chondral fragmentation and resultant full-thickness chondral defects seen on MRI/MRA. This can be visualized arthroscopically as a partial thickness or full-thickness chondral flap. These changes are classically described as appearing in the anterosuperior aspect of the acetabulum.
Case 2
A 19-year-old Division 1 female college soccer player presents with a 5-year history of anterior left hip and groin pain. Her symptoms became progressively more painful 1 month prior to the presentation in the office. The pain was exacerbated by running and soccer performance. The team trainers diagnosed psoas tendinitis and FAI. Activity modification, sports cessation, and physical therapeutic exercise failed to relieve her pain. After physical exam and plain radiographs confirmed impingement, MRI arthrogram confirmed chondrolabral injury. Arthroscopy with correction of Cam impingement through femoral osteochondroplasty and labrum repair was performed. She returned to play 1 year following the procedure shown. See Figs. 28.4, 28.5, and 28.6.

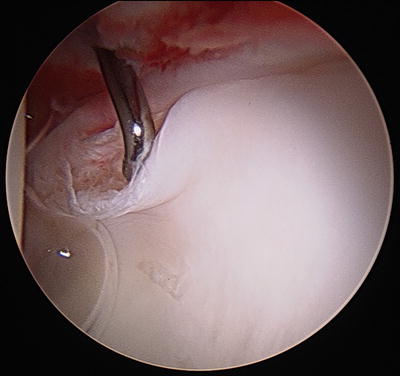
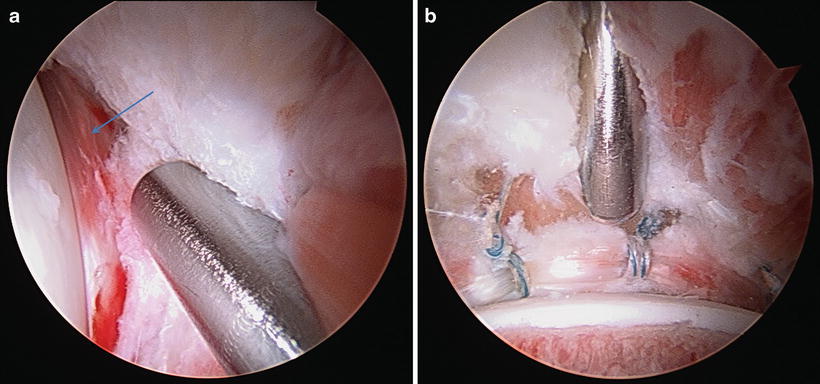

Fig. 28.4
T2-weighted MRI arthrogram image of affected hip. Note the light signal tracking between the articular cartilage and subchondral bone and the contrast signal penetrating the chondrolabral juncture (yellow arrow)
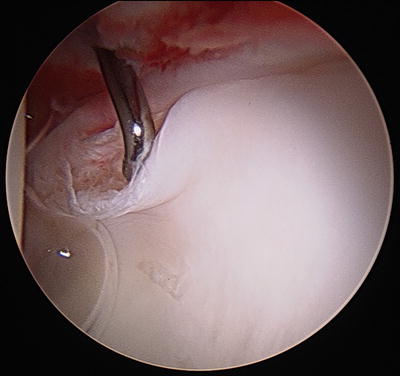
Fig. 28.5
Arthroscopy image with probe exposing the chondrolabral separation due to the Cam impingement in the same region as MRI arthrogram demonstrated signal abnormalities
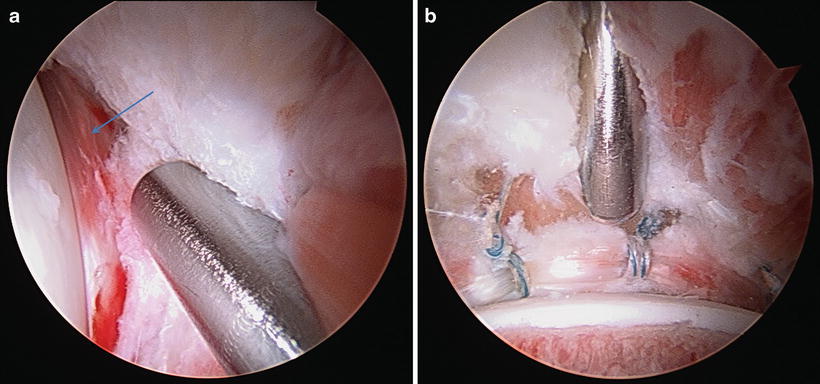
Fig. 28.6




(a, b) Arthroscopy images of the hip reduced following labrum repair and Cam decompression. a demonstrates bruising in the labrum (arrow) consistent with pincer pattern damage. This type of injury is frequently not appreciable on MRI
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree








