Foreign Bodies
Tim S. Gibbs
|
OBJECTIVES
Identify and give examples of different types of soft-tissue foreign bodies (STFBs) based on composition.
Explain sensitivity and specificity.
List the important information the sonographer should obtain from the patient interview and patient chart prior to providing a comprehensive sonography evaluation.
Differentiate the different sonographic appearances of STFBs based on composition, location, age, and artifacts.
Describe the role of the sonographer prior to, during, and following sonography-guided foreign body (FB) removal.
Explain the limitations of sonography and the advantages of other imaging modalities used to image STFBs.
KEY TERMS
foreign bodies
granuloma
hypoechoic halo
inorganic
organic reverberation
rim
sensitivity
shadowing
soft tissue
specificity
GLOSSARY
granuloma
a tumor-like mass formation that usually contains macrophages and fibroblasts and forms as a result of chronic inflammation and isolation of the infected area
a tumor-like mass formation that usually contains macrophages and fibroblasts and forms as a result of chronic inflammation and isolation of the infected area
hyperemia
an increase in the quantity of blood flow to a body part; increased blood flow as in the inflammatory response
an increase in the quantity of blood flow to a body part; increased blood flow as in the inflammatory response
in vitro
when referring to a biologic process, it is made to occur in a laboratory vessel or in a controlled experimental environment but does not occur within a living organism or in a natural setting
when referring to a biologic process, it is made to occur in a laboratory vessel or in a controlled experimental environment but does not occur within a living organism or in a natural setting
in vivo
when referring to a biologic process, it occurs or is made to occur within a living organism or natural setting
when referring to a biologic process, it occurs or is made to occur within a living organism or natural setting
occult
in reference to foreign bodies (FBs), the term refers to something hidden from view
in reference to foreign bodies (FBs), the term refers to something hidden from view
radiolucent
a tissue or material that allows transmission of X-rays and appears more dense (dark) on a radiograph; also known as nonradiopaque; for a FB, the material will often blend in and cannot be differentiated from the surrounding soft tissue
a tissue or material that allows transmission of X-rays and appears more dense (dark) on a radiograph; also known as nonradiopaque; for a FB, the material will often blend in and cannot be differentiated from the surrounding soft tissue
radiopaque
a tissue, contrast, or material that attenuates or blocks radiation; the tissue, contrast, or material will appear bright on the radiograph
a tissue, contrast, or material that attenuates or blocks radiation; the tissue, contrast, or material will appear bright on the radiograph
Conventional radiography, fluoroscopy, computed tomography (CT), magnetic resonance imaging (MRI), nuclear medicine, and sonography have been used to demonstrate the presence of foreign bodies (FBs). The purpose of this chapter is to present the sonographic scanning technique to recognize, locate, and assist in the removal of various types of soft-tissue foreign bodies (STFBs) in superficial structures. Increasing sonographer and clinician awareness and confidence to choose sonography for STFB detection, localization, and removal may result in increased diagnostic accuracy and decreased diagnostic expense.
COMPOSITION OF FOREIGN BODIES
FBs can be separated into three distinct categories based on their composition (Table 27-1). Organic material refers to biologic plant material and animal products. Inorganic materials are usually man-made products composed of minerals or made from minerals but are not animal or vegetable in origin. Metallic materials are those products with a metal alloy.
Sensitivity and Specificity
Radiographic imaging for FBs has been used for many years with some degree of success. Because radiography relies on the density of the FB, it has varied sensitivities for imaging the different types of FBs. Radiography detects 98% of radiopaque objects such as gravel, most glass, and metal1; however, radiography detects only 15% or less of radiolucent FBs such as wood, plastic, some glass, and cactus spine.2 Despite the poor sensitivity of radiography to demonstrate many organic objects and some inorganic objects, conventional radiography remains the most commonly used imaging study for the evaluation of FBs in the emergency department.3 Consequently, many FBs are missed on initial evaluation. In fact, missed FBs are the second leading cause of malpractice lawsuits against emergency medicine physicians.4,5 Wound care litigation constitutes 5% to 20% of lawsuit claims against emergency medicine physicians and results in 3% to 11% of monetary rewards.6,7
TABLE 27-1 Composition of Foreign Bodies | ||||||
|---|---|---|---|---|---|---|
|
Sonography performs well in demonstrating the FBs traditionally considered the most difficult to image on radiographic studies. In a retrospective study where radiography failed to demonstrate a STFB, sonography had a sensitivity of 95% and a specificity of 89%.8,9 In a prospective study using cadaver feet and wooden FBs, Jacobson et al.10 reported that sonography can reveal wooden FBs as small as 2.5 mm in length with 86.7% sensitivity and 96.7% specificity. At the time of this study, the resolution of the sonography equipment either makes visualizing FBs smaller than 2.5 mm more difficult or limits adequate visualization. The equipment used today are capable of resolving objects within ±1 mm. Most recently, Mecado and Hayre11 compared direct digital radiography (DDR) with sonography and concluded that sonography remains superior in identifying and detecting smaller FBs.
Sonography Equipment
Whenever possible, a 7-to-18-MHz high-resolution, linear array transducer should be used to obtain the images.12 A large-footprint transducer is generally preferable for initial FB imaging and localization, but a small-footprint transducer may be used when indicated. Maximizing image size by using a large, high-resolution monitor also facilitates FB identification. It may be difficult to identify small FBs on smaller monitors seen on some portable equipment. The visualization of superficial FBs may be facilitated by use of a water bath (Fig. 27-1). When it is necessary to increase the near field length for better visualization of the skin
surface and to place a superficial FB in the focal zone, the sonographer can use a standoff gel pad13, 14 and 15 or something as simple as a thicker layer of scanning gel10 (Fig. 27-2).
surface and to place a superficial FB in the focal zone, the sonographer can use a standoff gel pad13, 14 and 15 or something as simple as a thicker layer of scanning gel10 (Fig. 27-2).
Imaging Technology
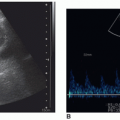
Shadowing and reverberation artifacts are helpful in both identifying and locating an FB. Newer technology does not provide any apparent improvement when imaging FBs and actually may make detection more difficult. Two of these instrumentation selections are tissue harmonics imaging (THI) and instrumentation that uses transmit beam-steering to create multiple imaging angles and then combines these microimages from different viewing angles into a single compounded image. The use of multiple imaging angles reduces shadow artifact, which is an important secondary sign in the detection of FBs (Fig. 27-3).
The same is true for THI, where shadowing is diminished or eliminated completely. Only the speckle reduction imaging (SRI) feature has helped improve image quality over normal imaging parameters (Fig. 27-4).
The same is true for THI, where shadowing is diminished or eliminated completely. Only the speckle reduction imaging (SRI) feature has helped improve image quality over normal imaging parameters (Fig. 27-4).
 FIGURE 27-4 A toothpick in the plantar surface of the foot is seen on these two images. Compare the foreign body image without speckle reduction (WO SRI) to the image with speckle reduction (W SRI). |
Color and power Doppler imaging may further increase sensitivity because the normal inflammatory reaction materializes in a hypoechoic ring around the FB as a result of hyperemic flow.16 Color Doppler parameters should be set to visualize slow flow (low velocity) to help determine if reactive hyperemia is present.16 Varying the transducer angle in relation to the FB will ensure the best color flow image is obtained with the highest Doppler shift.
EVALUATING COMPOSITION, LOCATION, AGE, AND APPEARANCE
Before beginning the imaging examination, the patient interview should be conducted and the patient’s chart reviewed. If a radiographic procedure has already been performed, the radiographs should be reviewed. The information that is helpful prior to scanning includes ascertaining the type of material, the mechanism of injury to include the point of entry, and the duration of symptoms.
Composition
The organic FB is the most difficult to locate and is rarely demonstrated on radiography; however, organic FBs are easier to locate and demonstrate on sonography. The echogenic pattern of an organic FB varies with its indwelling age. Some inorganic FBs can be difficult to image using radiography but present little challenge for sonography. Metallic FBs can be seen on radiography and sonography. Metals and most glass are radiopaque (with metals being more radiopaque than glass) and relatively easily seen with radiography (Fig. 27-5).
Location
When locating an FB, radiographs should be use if available to provide further information regarding the location, depth, and composition of the FB. When used, radiographs should be obtained in two perpendicular projections (imaging planes) in order to triangulate the location. The FB will only be radiographically visualized if its density is greater than the surrounding soft tissue.
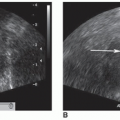
Radiographs may assist in targeting the location for initial insonation. This is especially helpful when external signs such as swelling or redness are not present. A working knowledge of the normal soft-tissue structures can assist in separating normal structures from that of the FB (Fig. 27-6A). By documenting these anatomic structures and their relationship to the FB (veins, arteries, tendons, etc.), the physician can plan the best approach for its removal to diminish postoperative complications14 (Fig. 27-6B).
The smaller the FB, the more difficult it is to visualize.17 The depth of an FB will determine the optimal frequency of the transducer. Ideally, the highest frequency possible that allows adequate depth of penetration should be utilized. Every attempt should be made to visualize the FB perpendicular to the transducer to minimize the potential errors in location and position within the soft tissue14 (Fig. 27-7). When the FB is visualized, its location should be marked on the overlying skin for the physician to use during sonography-guided FB removal.
 FIGURE 27-6 Knowledge soft-tissue structures and anatomic relationships is important to enable differentiating anatomy from a foreign body and to identify the foreign body location. A: A transverse sonogram demonstrates three linear echogenic structures (arrows). The structures are three right carpal bones but were mistaken for foreign bodies. B: A sonogram of the right hand shows the relationship of the foreign body (arrows) to an artery (A). C: Broken needle with the tip still within the vein. D: Glass fragment still present under the upper eyelid after copious irrigation.
Stay updated, free articles. Join our Telegram channel
Full access? Get Clinical Tree
 Get Clinical Tree app for offline access
Get Clinical Tree app for offline access

|