Fungal infections of the central nervous system (CNS) frequently occur in the immunocompromised or debilitated host. Imaging findings are non-specific but may be organized into extra-axial, parenchymal, and vascular categories. Furthermore, knowledge of fungal morphology may predict the imaging manifestations with large, hyphal species having a predilection for brain parenchymal involvement, while small, unicellular organisms typically result in meningitis. Advanced imaging techniques such as diffusion-weighted imaging, MR perfusion and MR spectroscopy, when combined with clinical findings, may help in differentiating fungal disease from other mimckers such as pyogenic infection or cystic metastases.
- •
The increasing incidence of central nervous system (CNS) fungal infections is thought to be related to the AIDS epidemic, an increase in transplants, and resistance to antifungal agents.
- •
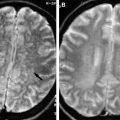
MRI, given its superior contrast resolution relative to CT imaging, remains the preferred imaging modality in the evaluation of CNS infection.
- •
Imaging findings of fungal disease are nonspecific but may be organized as parenchymal (granulomas, cerebritis, and abscess), extra-axial (meningitis, sinusitis), and vascular (vasculitis, mycotic aneurysm).
- •
In general, morphology may predict imaging manifestations: large, hyphal organisms ( Aspergillus) commonly involve the brain parenchyma, whereas small unicellular organisms ( Candida , Cryptococcus) commonly cause meningitis.
- •
Advanced imaging techniques, including diffusion-weighted imaging, MR perfusion, and MR spectroscopy, may aid in differentiating fungal from pyogenic or neoplastic disease.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree