“Incidentalomas” are a common part of daily practice for radiologists, and knowledge of appropriate management guidelines is important in ensuring that no potentially clinically relevant findings are missed or are lost to follow-up in asymptomatic patients. Incidental findings of the brain, spine, thyroid, lungs, breasts, liver, adrenals, spleen, pancreas, kidneys, bowel, and ovaries are discussed, including where to find guidelines for management recommendations, how to follow them, and medical-legal considerations.
Key points
- •
“Incidentalomas” are common part of daily practice for radiologists, and knowledge of appropriate management guidelines ensures no potentially clinically relevant findings are lost to follow-up.
- •
Awareness of appropriate guidelines, how to follow them, as well as management and medical-legal considerations, is the ideal approach for incidentalomas in daily practice.
- •
Management guidelines are available for incidentalomas of the brain, thyroid, lungs, liver, adrenals, spleen, pancreas, kidneys, and ovaries, on cross-sectional imaging.
- •
No established management guidelines are presently available for incidentalomas of the spine, breast, or bowel, to our knowledge.
Introduction
Incidental imaging findings identified in a patient who is asymptomatic or undergoing diagnostic testing for unrelated reasons, termed “incidentalomas,” have become commonplace in a radiologist’s daily practice, regardless of what part(s) of the body the imaging that they interpret includes. , The demand for additional imaging of initially detected incidentalomas continues to grow, and this can result in substantial patient anxiety, particularly when there is clinical uncertainty regarding the best approach for management. As a result of this, in addition to detection and diagnosis, radiologists should take an active role in management recommendations of these incidentalomas. This practice can ensure that concerning findings are not lost to follow-up, and that completely benign findings are not overinvestigated. However, keeping up to date with the latest guidelines for every type of incidentaloma in each organ system can be an increasingly daunting task for any radiologist. The purpose of this chapter is to provide a general review on the current management of incidental findings on cross-sectional imaging, including what guidelines to use and how to follow them, as well as management and medical-legal considerations. Incidental findings of the brain, spine, thyroid, lungs, breasts, liver, adrenals, spleen, pancreas, kidneys, bowel, ovaries, and uterus are discussed, with the greatest focus on the current American College of Radiology (ACR) White Papers relevant to each organ system. This introductory article sets the stage for the multiple articles that follow, and that cover incidentalomas in specific organ systems and scenarios in greater detail.
Incidental findings on computed tomography and MR imaging of the brain
What Guidelines to Use and How to Follow Them
In terms of incidental findings of the brain, we focus on the pituitary, with the ACR White Paper entitled “Management of Incidental Pituitary Findings on CT, MR imaging, and 18 F-Fluorodeoxyglucose PET.” The most common incidental pituitary findings are Rathke cleft cysts and pituitary adenomas, with less common incidentals (or unexpected findings) including epidermoid cysts, metastases, infarctions, or hemorrhage. When large enough, suprasellar or parasellar masses, such as craniopharyngiomas or meningiomas, can mimic primary pituitary masses. The main factors that will affect the need for further imaging of a pituitary incidentaloma include the imaging characteristics, its size, any mass effect, and endocrine function. In terms of imaging characteristics on computed tomography (CT) and MR imaging, if the finding is that of a simple cyst, no further imaging follow-up is required, as this is most likely a Rathke cleft cyst. Meanwhile, a solid or mixed-solid cystic pituitary mass most likely represents a pituitary adenoma. A solid or mixed-solid cystic focus measuring 10 mm or smaller also does not require imaging follow-up. However, any solid or mixed-solid cystic mass measuring larger than 10 mm should have a follow-up pituitary MR imaging in 6 to 12 months. Otherwise, any solid or mixed cystic solid mass should undergo endocrine workup, whereas pituitary masses of any composition causing mass effect or invasion of surrounding structures requires neurosurgical and/or endocrine consultation.
Management and Medical-Legal Considerations
The main considerations for follow-up imaging of incidental pituitary findings are related to growth and hemorrhage (pituitary apoplexy), which are predominantly seen in solid or mixed-solid cystic masses >10 mm. , Clinical implications of growth or hemorrhage include the risk of hypopituitarism, visual field deficits, or ophthalmoplegia. Although a small portion of pituitary microadenomas (≤10 mm) have been found to have microhemorrhage (3%), this was much lower than the rate in pituitary macroadenomas (>10 mm, 20%). Furthermore, patients with pituitary apoplexy resulting in compressive symptoms all had underlying pituitary macroadenomas, whereas patients with pituitary microadenomas who underwent hemorrhage were asymptomatic. Otherwise, the reported prevalence of incidental neoplasms on brain MR imagings in general was 0.7%. , The prevalence of non-neoplastic findings was 2.0%, most commonly arachnoid cysts (0.5%) and aneurysms (0.35%). Established guidelines exist for the management of intracranial aneurysms, published by the American Heart Association, the American Stroke Association, and the European Stroke Organization, which are beyond the scope of this article. ,
Incidental spine findings on computed tomography and MR imaging
There are no well-established guidelines that radiologists may follow for incidental findings of the spine on CT and MR imaging, to our knowledge. A review of incidentalomas in spinal cord imaging reported on the following potential incidental findings of the spinal cord and nerve roots: syringohydromyelia, ventriculus terminalis, lipoma of the filum terminale, perineural cysts, cerebrospinal fluid flow artifacts, and enhancement of radicular vein and vein of the filum terminale. In addition, the following incidentalomas of the vertebral body and posterior arch were also reported on: vertebral hemangioma, butterfly vertebra, block vertebra, benign notochord cell tumor, bone island/enostosis, and incomplete vertebral fusion/cleft of C1. The development of management guidelines for potentially clinically relevant spine incidentalomas is warranted. For example, in rare cases of ventriculus terminalis, notochord cell tumors, and vertebral hemangiomas, underlying malignancy or aggressive/malignant features should be excluded, and an intravenous (IV) contrast-enhanced examination may be warranted. A prevalence of upward of 22% has been reported for incidentalomas detected on MR imaging of the spine, although this included extraspinal findings.
Imaging of incidental thyroid nodules
What Guidelines to Use and How to Follow Them
For imaging and management guidelines of incidental thyroid nodules, use of the ACR White Paper entitled “ACR Thyroid Imaging, Reporting, and Data System (TI-RADS)” is recommended, along with a dedicated explanation for the lexicon, as well as a user’s guide from the TI-RADS committee. This guideline is applied for incidental thyroid abnormalities identified in head and neck imaging of asymptomatic adults without risk factors for thyroid cancer. Both CT and MR imaging examinations are limited in determining whether a thyroid nodule is benign or malignant. As such, management of incidental thyroid nodules is divided into assessment with dedicated thyroid ultrasound versus no dedicated follow-up. If an incidental thyroid finding is identified on CT or MR imaging, any of the following criteria warrant further assessment with a dedicated ultrasound: suspicious imaging features (local invasion, abnormal lymph nodes); patient younger than 35 years and size ≥1.0 cm; or patient age ≥35 years and size ≥1.5 cm. Based on the dedicated thyroid ultrasound findings, a TI-RADS score is assigned, which in combination with size of the abdominality, determines whether further ultrasound follow-up or a fine-needle aspiration (FNA) is needed. The TI-RADS score ranges from TR1 (benign) to TR5 (high suspicion of malignancy), and it is based on size, echogenicity, shape, margin, and the presence of echogenic foci.
Management and Medical-Legal Considerations
Incidental thyroid nodules in adults are quite common, and are reportedly seen in up to 16% to 18% of CT and MR imaging examinations of the head and neck. The estimated rate of thyroid incidentalomas found to be malignant ranges from 19% to 28%. However, failure to diagnose thyroid malignancies smaller than 2 cm is unlikely to affect morbidity and mortality. A study of 401 patients with incidental thyroid nodules on CT or MR imaging found that thyroid nodules were mentioned in the radiology reports of 375 patients (94%), and in the impression section of the reports in 138 patients (37%). In total, 26 (19%) of 138 patients received additional workup, and patients with the findings mentioned in the impression were 14 times more likely to have further assessment. Only one papillary thyroid cancer was missed to the authors’ knowledge in this study.
Incidental lung nodules on computed tomography: current Fleischner Society and other guidelines
What Guidelines to Use and How to Follow Them
The Fleischner Society guidelines are recommended for the management of incidental lung nodules on CT, the most recent of which is the “Guidelines for Management of Incidental Pulmonary Nodules Detected on CT Images: From the Fleischner Society.” These recommendations apply to incidental pulmonary nodules seen on CT in patients ≥35 years old, and importantly they do NOT apply to patients undergoing lung cancer screening, those with immunosuppression, or those with known primary lung cancer. Management recommendations are dependent on nodule type, size, and stability over time. Furthermore, risk factors for malignancy also influence management, with patients clinically stratified into low-risk or high-risk groups based on smoking history, age, and upper lobar location of the nodules. Guideline recommendations include chest CT follow-up intervals at 3 to 6 months and 6 to 12 months, as well as an optional 12-month follow-up. Concerning nodules may warrant recommendations for PET/CT and/or tissue sampling, whereas nodules smaller than 6 mm in low-risk patients do not require any further follow-up.
Management and Medical-Legal Considerations
Incidental lung nodules are common, with reported prevalence rates of 8.5% in a study of 248 trauma patients undergoing thoracic CT assessment, whereas screening chest CT examinations in older patients with a smoking history had reported lung nodule prevalence rates of 23%, of which 2.7% were malignant. Meanwhile, a study of 243 patients undergoing abdominal CT demonstrated incidental lung nodules in 39% of patients, of which only 8.4% were mentioned in the final patient report. Of note, in populations at high risk of lung cancer, the prevalence of cancer was 0.1% to 1.0% for smaller than 5 mm, 1% to 30% for 5 to 10 mm, and 30% to 80% for larger than 10 mm CT-detected nodules. Furthermore, multiple trials have demonstrated a statistically significant mortality benefit for low-dose screening chest CT in patients at higher risk for lung cancer.
Incidental breast findings on computed tomography and MR imaging
There are no well-established consensus guidelines for incidental findings of the breasts on CT and MR imaging. A practical guide proposes a management algorithm for commonly encountered incidental findings in the breasts on CT in patients without previous mammographic evaluation. Macrocalcifications and macroscopic fat were defined as benign findings, skin thickening, and rounded masses were defined as indeterminate findings, and masses with irregular shape or spiculated margins, masslike enhancement, and axillary adenopathy were defined as highly suspicious features. For definitively benign findings, no further workup is recommended, while suspicious features warrant diagnostic breast imaging. If indeterminate findings are present without suspicious features, correlation with prior relevant imaging examinations, if available, is recommended. If there is documented stability for a period of at least 2 years, no further workup is recommended. Otherwise, further diagnostic breast imaging is recommended. Of note, when breast malignancy is suspected, the presence of skin thickening, nipple retraction, local invasion, and axillary adenopathy may be better assessed on CT than mammography. A study of 11,462 women undergoing liver MR imaging identified breast incidentalomas in 292 patients (3%), and dedicated breast imaging was recommended for 192 of these patients (66%). A total 10 incidental breast malignancies (3% of all breast incidentalomas) were identified.
Incidental liver findings on cross-sectional imaging
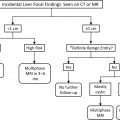
What Guidelines to Use and How to Follow Them
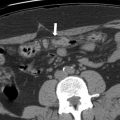
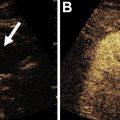
Multiple guidelines are available for assessment of liver findings on cross-sectional imaging. In asymptomatic adult patients for whom a CT was requested for an unrelated reason, the ACR White Paper titled “Management of Incidental Liver Lesions on CT” is recommended for use. , Guideline recommendations include no further workup, a follow-up hepatic MR imaging in 3 to 6 months, a hepatic MRI examination now, or immediate biopsy. , Management options are based on size of the identified abnormality, imaging features, and patient risk for hepatic malignancy (eg, cirrhosis, known malignancy, hepatic dysfunction). , However, these guidelines should not be applied for imaging examinations to evaluate a known or suspected liver nodule or mass or other hepatic abnormality. , The Liver Imaging Reporting and Data System (LI-RADS) may be applied in the context of the diagnosis of hepatocellular carcinoma (HCC) with CT or MR imaging in patients with or at high risk for HCC. The LI-RADS guidelines should specifically be applied in patients with cirrhosis, chronic hepatitis B virus, or current or prior HCC. The LI-RADS scores range from LR-1 (definitely benign) to LR-5 (definitely HCC), as well as LR-TIV (malignancy with tumor in vein) and LR-M (probably or definitely malignant, not HCC-specific).
Management and Medical-Legal Considerations
For incidentalomas in asymptomatic patients undergoing liver CT for different reasons, a nodule smaller than 1 cm in a low-risk patient is considered benign and does not require further follow-up, whereas 3-month to 6-month follow-up with MR imaging is recommended in high-risk patients. , For any other focal liver findings with benign features, no further workup. For those with suspicious features, generally, prompt MR imaging is recommended in low-risk patients, whereas prompt MR imaging or biopsy may be recommended in high-risk patients. , Flash-filling nodules larger than 1.5 cm in low-risk patients and larger than 1.0 cm in high-risk patients warrant further assessment with MR imaging. , In the context of the LI-RADS, the prevalence of malignancy by category was reported as 14% in LR-2, 40% in LR-3, 80% in LR-4, 97% in LR-5, 92% in LR-TIV, and 93% for LR-M.
Incidental adrenal findings on computed tomography
What Guidelines to Use and How to Follow Them
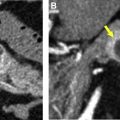
Use of the ACR White Paper titled “Management of Incidental Adrenal Masses” is recommended for management of incidental adrenal masses on CT or MR imaging. Management of adrenal incidentalomas is divided into benign nodules/masses that do not require follow-up, and intermediate nodules/masses requiring further workup. Management recommendations are guided by size, density, and imaging features, such as the presence of fat and calcifications. Further workup options include imaging follow-up with a dedicated adrenal CT (and in limited cases, MR imaging) protocol, PET/CT, biopsy, or resection. This is based on size, growth on follow-up, history of malignancy, and imaging features (including density on nonenhanced CT and washout characteristics on adrenal protocol CT ).
Management and Medical-Legal Considerations
Incidental adrenal masses are common, reported in up to 3% to 7% of adults. Malignancy has been reported in up to 0.5% of adrenal incidentalomas. A study of 1149 patients diagnosed with adrenal incidentalomas found that most (68%) were nonfunctional. Adrenal protocol CT demonstrated a sensitivity of 100% and specificity of 95% in differentiating benign from malignant adrenal nodules. In general, an incidental adrenal nodule measuring smaller than 1 cm in the short axis, or one with benign features, including macroscopic fat, hemorrhage, a cyst, or features consistent with adenoma, do not require further imaging follow-up. For incidental adrenal masses that are larger than 4 cm with indeterminate features or are new/growing compared with previous imaging, resection should be considered if there is no cancer history, whereas biopsy or PET/CT is recommended if there is known cancer. Incidental adrenal nodules/masses that show ≥1 year stability are considered benign and do not require follow-up. Incidental adrenal nodules/masses with indeterminate imaging features measuring 1 to 2 cm are likely benign and may have a follow-up adrenal CT in 12 months, whereas an adrenal incidentaloma measuring ≥2 cm and smaller than 4 cm should undergo an adrenal protocol CT.
Incidental splenic findings on cross-sectional imaging
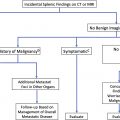
What Guidelines to Use and How to Follow Them
For the management of incidental splenic findings, the ACR White Paper titled “Managing Incidental Findings on Abdominal and Pelvic CT and MR imaging, Part 3” is recommended. Recommendations are based on imaging characteristics, clinical history, and findings on prior imaging. Management categories include no further workup, follow-up imaging, evaluation with PET/CT, MR imaging, and/or biopsy. No follow-up imaging is needed if an incidental finding or findings demonstrates benign features or 1-year stability. Follow-up imaging, specifically an MR imaging in 6 months, is recommended for a finding with indeterminate imaging features with no history of cancer, or for a nodule smaller than 1 cm in a patient with a history of cancer. Further evaluation with PET/CT, MR imaging, and/or biopsy is recommended if it demonstrates suspicious features, growth over time, or one that measures ≥1 cm in a patient with history of cancer. Suspicious imaging features include heterogeneity, enhancement, irregular margins, necrosis, parenchymal/vascular invasion, and growth over time. Benign imaging includes findings of a simple cyst, hemangioma, or a nodule/mass that otherwise appears homogeneous, measuring less than 20 Hounsfield units in density, with smooth margins.
Management and Medical-Legal Considerations
Most incidentally discovered splenic masses are benign and of no clinical significance. Biopsy of splenic masses is rarely recommended, usually in cases of suspected angiosarcoma or in a patient with history of known malignancy with concern for metastasis or lymphoma. A study assessed 379 patients with splenic incidentalomas divided into 3 groups: patients with known malignancy (145 patients), patients with constitutional symptoms and/or abdominal pain (29 patients), and asymptomatic patients (205 patients). The incidence of malignant splenic masses was 49 (34%) of 145 patients with known malignancy, 8 (28%) of 29 of patients with constitutional symptoms and/or abdominal pain, and 2 (1%) of 205 in asymptomatic patients.
Incidental pancreatic cysts on cross-sectional imaging
What Guidelines to Use and How to Follow Them
Use of the ACR White Paper titled “Management of Incidental Pancreatic Cysts” is recommended for guideline recommendations of cystic pancreatic incidentalomas. The most commonly seen pancreatic cystic tumors/masses include intraductal papillary mucinous neoplasms, serous and mucinous cystadenomas, solid pseudopapillary epithelial neoplasms, and pseudocysts. Management options include no further workup, 1-year follow-up, 2-year follow-up, endoscopic ultrasound with FNA, and surgical consultation. Management recommendations are based on multiple factors, including size, interval growth, and imaging features, as well as patient age and clinical history (eg, pancreatitis).
Management and Medical-Legal Considerations
Prevalence rates of cysts within the pancreas of 1.0% to 2.6% on CT and 13.5% to 15.9% on MR imaging have been reported. In a study of 1038 patients, radiologists recommended follow-up imaging in 13.5% of cases of incidental pancreatic cysts identified on CT and MR imaging. Radiologists appropriately adhered to the ACR guidance principles in 47.4% of the cases, and there was significant variation in recommendations across different radiologists. MR imaging was the most frequently recommended imaging modality for follow-up. Moreover, most incidental pancreatic cysts were smaller than 2 cm (72.6%), whereas only 9.1% measured larger than 3 cm.
Incidental renal findings on cross-sectional imaging
What Guidelines to Use and How to Follow Them
Utilization of the ACR White Paper titled “Management of the Incidental Renal Mass on CT” is recommended for incidental renal masses in asymptomatic adult patients without conditions that predispose them to renal neoplasms, or a primary malignancy that may metastasize to the kidneys. , Management recommendations include no further workup, further assessment with CT or MR imaging, or urologic consultation for management and/or biopsy. , The recommendations are based on size, attenuation, enhancement, heterogeneity, growth, morphologic change, and the complexity of cystic masses, incorporating the Bosniak classification system. Multiple management pathways are provided for the following scenarios for incidental renal masses: noncontrast CT, IV contrast-enhanced CT, cystic renal mass (Bosniak classification), solid renal mass or too small to characterize, and renal mass containing fat. ,
Management and Medical-Legal Considerations
Most incidental renal masses are benign cysts, for which the prevalence increases with age. Benign renal cysts may be seen in up to 40% of patients undergoing an abdominal CT. In a study of 5383 patients in the emergency department undergoing CT for renal colic, a prevalence rate of 3.1% was reported for “significant” incidental renal findings, defined as findings for which the radiologist explicitly stated follow-up imaging was required. This study also confirmed the positive correlation between patient age and the prevalence of significant incidental findings; 80-year-old patients were 4 times more likely than patients aged 18 to 30 to have significant incidental findings.
Incidental bowel findings on computed tomography
There are no well-established consensus guidelines for bowel incidentalomas on CT, to our knowledge. A previous systematic review of incidental findings in imaging diagnostic tests reported a prevalence of 25% for incidental findings of the gastrointestinal and genitourinary systems seen on diagnostic imaging examination. Incidental findings within the gastrointestinal system were classified as “major”, “moderate”, or “minor” depending on their clinical significance. A variety of incidentalomas related to the bowel were reported, including but not limited to diverticular disease, hernias, intestinal polyps, and bowel wall thickening. Although a more standardized approach for follow-up is warranted, the systematic review found up to 64% of incidental findings within the gastrointestinal and genitourinary systems had some form of clinical follow-up or clinical confirmation of the diagnosis.
Incidental adnexal findings on cross-sectional imaging
What Guidelines to Use and How to Follow Them
For management guidelines of adnexal findings on cross-sectional imaging, use of the ACR White Paper titled “Management of Incidental Adnexal Findings on CT and MR imaging” is recommended, which is an update of the ACR White Paper titled “Managing Incidental Findings on Abdominal and Pelvic CT and MR imaging, Part 1.” , These management guidelines apply to incidental adnexal masses measuring larger than 1 cm in asymptomatic postmenarchal women. , The guidelines do not apply in women at high genetic risk for ovarian cancer, in women who develop related symptoms, or in findings that are stable for ≥2 years, as this excludes malignancy. , Adnexal incidentalomas may be placed into 1 of the following 3 categories: (1) simple-appearing cyst smaller than 10 cm, (2) uncertain diagnosis or simple cyst larger than 10 cm, or (3) features characteristic of other diagnosis. , A simple-appearing cyst smaller than 10 cm may have recommendations for no further follow-up, further characterization with ultrasound, or follow-up imaging with ultrasound depending on cyst size, imaging features, and menopausal status. , For an uncertain diagnosis or simple cyst larger than 10 cm, an ultrasound or MR imaging is recommended for further characterization. , Features characteristic of a specific diagnosis, such as a hemorrhagic cyst, fibroma, leiomyoma, hydrosalpinx, peritoneal inclusion cyst, or suspected malignancy, often require further assessment with ultrasound, MR imaging, or gynecologic assessment, with few exceptions. ,
Management and Medical-Legal Considerations
Although it is understood that incidental adnexal simple cysts have a very low risk of malignancy, there are justifications for some adnexal cysts warranting short-interval follow-up in asymptomatic patients. , One is the risk of incorrect characterization of the incidental finding as a simple cyst, whereas the second is that some simple adnexal cysts may represent slow-growing benign ovarian neoplasms (cystadenomas). , A study conducted in 2869 women older than 50 years undergoing CT colonography screening identified indeterminate adnexal findings in 118 women (4.1%), with a mean size of 4.1 cm. A total of 80 women underwent further imaging workup, and final surgical pathology of excised masses included 14 cystadenomas, 3 teratomas, 2 endometriomas, 2 cases of hydrosalpinx, and 1 fibroma. , No ovarian malignancies had been detected based on further imaging workup and surgical excision. ,
Summary
Incidentalomas are common part of daily practice for radiologists, and knowledge of appropriate management guidelines is important in ensuring no potentially clinically important or relevant findings are missed or lost to follow-up in asymptomatic patients. Although familiarization with the latest guideline recommendations for every type of incidentaloma throughout the body may be an increasingly daunting task for any radiologist, awareness of the guidelines available, how to follow them, and where to access them, may be the ideal approach. Hopefully this article, and the more focused articles that follow, will also provide the practicing radiologist with a useful update on a multitude of scenarios that incidental findings are detected on cross-sectional imaging examinations of multiple organ systems in the human body.
Clinics care points
- •
Incidental imaging findings, or “incidentalomas”, may vary from benign findings with no follow-up required to more clinically significant findings for which require additional imaging and/or intervention.
- •
Radiologists play an important role in making recommendations for the appropriate management of incidentalomas seen on diagnostic imaging.
- •
Utilization of the most up to date guidelines for management of incidentalomas is key to ensuring clinically significant incidental findings receive the appropriate follow-up, and completely benign findings are not over-investigated.
- •
This chapter provides a general review of on the current management of incidental findings on cross-sectional imaging, including what guidelines to use and how to follow them, as well as management and medical-legal considerations.
Disclosure
Dr M.N. Patlas receives an honorarium from Springer. The remaining coauthors have nothing to disclose.
References
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree