(1)
Department of Nuclear Medicine, Kuwait University, Safat, Kuwait
6.1.1 Major Structures
6.1.2 The Nephron
6.1.3 Renal Vasculature
6.4 Major Diseases
6.4.3 Urinary Tract Infection
6.4.5 Vesicoureteral Reflux
6.4.6 Testicular Torsion
Abstract
The urinary system consists of a pair of kidneys, which remove substances from the blood, form urine, and help regulate various metabolic processes; a pair of tubular ureters, which transport urine away from the kidneys; a saclike urinary bladder, which serves as urine reservoir; and a tubular urethra, which conveys urine to the outside of the body.
6.1 Anatomical and Physiological Considerations
6.1.1 Major Structures
The urinary system consists of a pair of kidneys, which remove substances from the blood, form urine, and help regulate various metabolic processes; a pair of tubular ureters, which transport urine away from the kidneys; a saclike urinary bladder, which serves as urine reservoir; and a tubular urethra, which conveys urine to the outside of the body.
Kidneys are paired bean-shaped retroperitoneal organs situated in the posterior part of the abdomen on each side of the vertebral column against the psoas major muscle. The upper pole of each kidney lies at the level of the twelfth thoracic vertebra, and the lower pole lies opposite the third lumbar vertebra (Fig. 6.1). The right kidney is usually slightly more caudal in position. The weight of each kidney ranges from 120 to 170 g in the adult male and from 115 to 155 g in the adult female. It is approximately 11 × 6 × 2.5 cm. The concave medial surface of each kidney has a slit-like aperture called the hilum, through which the renal pelvis, the renal artery and vein, the lymphatics, and a nerve plexus pass into the kidney. The organ is surrounded by a tough fibrous capsule.


Fig. 6.1
A diagram illustrating main surface renal anatomy
On cut sections (Fig. 6.2), two distinct regions can be identified: a pale outer region, the cortex, and a darker inner region, the medulla. In humans, the medulla is divided into 4–18 striated conical masses, the renal pyramids (average 8). The base of each pyramid is positioned at the corticomedullary boundary, and the apex extends toward the renal pelvis to form a papilla. On the tip of each papilla are 10–25 small openings that represent the distal ends of the collecting ducts. The apex of each medullary pyramid is capped by a funnel-shaped minor calyx. The minor calyx receives the urine from the kidney and passes it to the extrarenal collecting system.
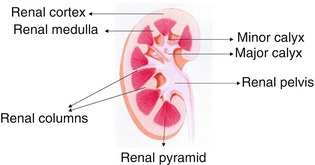
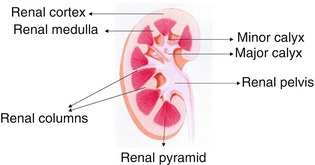
Fig. 6.2
A diagram illustrating cross section of the kidney
Since renal blood flow of approximately 400 ml/100 g is much higher than that of any other well-perfused organs such as the heart and brain, kidney tissue is prone to be exposed to significant amount of any potentially harmful circulating substances. Additionally glomerular capillaries are vulnerable to hemodynamic injury, in contrast to other capillary beds, because glomerular filtration is dependent on high intra- and trans-glomerular pressure. The organization of nephron’s microvasculature facilitates the spreading of glomerular injury to tubulointerstitial compartment in disease, exposing tubular epithelial cells to abnormal ultrafiltrate. Accordingly, the concept of the nephron as a functional unit applies not only to renal physiology but also to the pathophysiology of renal diseases.
6.1.2 The Nephron
The main functions of the kidneys are the maintenance of water, electrolyte, and acid–base balance, elimination of waste products, and regulation of blood pressure. The functional unit of the kidney is the nephron, which consists of a glomerulus and a tubule. The glomerulus consists of a network of capillaries derived from the afferent glomerular arteriole. This can be broadly divided into several portions: the proximal tubule, loop of Henle, distal tubule, and collecting tubule.
Urine is formed as a result of glomerular filtration, tubular reabsorption, and tubular secretion [1]. The glomerular capillary tuft acts as a filter for plasma. The glomerular filtration rate (GFR) is dependent largely on the hydrostatic and colloid osmotic pressure in the glomerular capillaries and the hydrostatic pressure in Bowman’s space. Filtered fluid enters the tubule. The proximal tubule plays a key role in reabsorbing filtered solutes. About half to two thirds of the sodium, chloride, and potassium are reabsorbed in this segment. Reabsorption of solutes is accompanied by passive osmotic diffusion of water. The loop of Henle, consisting of a descending limb and an ascending limb, is the site of reabsorption of about 25 % of the filtered solutes. Reabsorption occurs primarily in the “thick” ascending limb, where the epithelial cells are thick and metabolically very active. It is in this section that “loop” diuretics such as furosemide exert their effects (see later). The reabsorbed solutes enter the medullary interstitium and contribute to its hypertonicity.
The distal tubule transports sodium, chloride, and potassium, but not water, from its proximal part, similar to the loop of Henle. At the very beginning of the distal tubule is the macula densa, a region of specialized cells in close proximity to the juxtaglomerular (JG) cells in the afferent arteriole that store renin. In response to changes in sodium and chloride concentration in this portion of the tubule, the macula densa sends signals to the JG cells to release renin.
6.1.3 Renal Vasculature
In the human, each kidney is supplied normally by a single renal artery, although the presence of one or more accessory renal arteries is not uncommon. The renal artery enters through the hilum of the kidney and branches successively into the interlobar arteries, arcuate arteries, interlobular arteries, and afferent arterioles. Each afferent arteriole eventually branches into the glomerular capillaries. The distal glomerular capillaries merge to form the efferent arteriole. Efferent arterioles subdivide to form peritubular capillaries in the cortex or the vasa recta in the medulla. Changes in the afferent or efferent arteriolar tone play an important role in regulating the GFR.
6.1.4 Juxtaglomerular Apparatus
The afferent arteriole has specialized smooth muscle cells called juxtaglomerular (JG) cells that store renin and stretch receptors that respond to changes in arteriolar pressure. Renin is released as a result of decreased stretch of the arteriolar wall when arteriolar pressure is decreased, when the sodium and chloride content of this part of the tubule is low and in response to systemic baroreceptor stimuli.
6.2 Renal Radiopharmaceuticals
Renal radiopharmaceuticals can be described in two broad classes—those that are excreted rapidly into the urine and those that are retained for prolonged periods in the renal parenchyma.
(a)
The rapidly excreted radiopharmaceuticals are used in dynamic imaging studies to assess individual renal function and include:
1.
99mTc-mercaptoacetyltriglycine (MAG3), which is the agent of choice, is 90 % protein bound and excreted almost exclusively by the renal tubules. High renal-to-background count ratios provide excellent images and permit visualization of poorly functioning kidneys.
2.
99mTc-diethylenetriamine penta-acetic acid (DTPA) which was the most popular radiopharmaceutical in its category prior to the introduction of 99mTc-MAG3. It shows little protein binding (about 5 %) and is excreted exclusively by glomerular filtration. Renal uptake of 99mTc-DTPA is limited because only 20 % of the renal blood flow is filtered by the glomeruli. The 20 % extraction fraction is considerably lower than that of 99mTc-MAG3 and yields lower renal-to-background uptake ratios. However, it is less costly and may be used as an alternative to 99mTc-MAG3, particularly if a quantitative estimate of GFR is also needed.
(b)
The slowly excreted radiopharmaceuticals include 99mTc-dimercaptosuccinic acid (DMSA) and 99mTc-glucoheptonate. Prolonged cortical retention of these radiopharmaceuticals allows the assessment of parenchymal morphology, and since accumulation occurs only in functioning tubules, uptake can be quantified to assess accurately the differential renal function. The preferred agent, technetium-99 m-DMSA, is 90 % protein bound and accumulates in functioning tubules. Since very little of the radiotracer is excreted, interference from collecting system activity, particularly on delayed images, is minimal. A total of about 40 % of the administered amount is accumulated in the renal cortex.
6.3 Renal Scintigraphy
According to the types of renal radiopharmaceuticals, renal scintigraphy can be of dynamic or static nature.
Dynamic studies are obtained using the rapidly excreted radiopharmaceuticals, while static studies are obtained utilizing slowly excreted tracers. Dynamic studies start by rapid acquisition of image frames upon injection of the tracer to follow activity in passing through the blood vessels till reaching the kidneys to evaluate the blood flow. This phase is followed by another series of imaging frames every 10–20 s of the kidney over a period of approximately 30 min to evaluate the kidney functional handling of the radiotracer. This phase will be then computer processed to generate time-activity curve (renogram) for both kidneys to illustrate the uptake, buildup, and excretion of the radiopharmaceutical by each kidney and generate the percent contribution of each kidney to the total renal function (split or differential renal function).
Static studies using slowly secreted radiopharmaceuticals particularly 99mTc-DMSA are acquired 3 h after intravenous injection of the radiotracer and optionally up to 24 h based on the individual case and the kidney function. These studies are predominantly used to accurately determining the split renal function and in cases of urinary tract infections to evaluate the pathological changes including cortical scars. Anterior, posterior, and left and right posterior oblique planar views are obtained routinely with optional SPECT. Using the anterior and posterior views, the split renal function is calculated by the geometric mean of the background-subtracted kidney counts.
6.3.1 Principles of Interpretation
6.3.1.1 Dynamic Studies
Assessment of function on dynamic studies is based on a number of criteria, including initial cortical uptake of the radiotracer, cortical retention, first visualization of the collecting system, and time to peak cortical activity. These parameters however may be affected by the state of hydration. An adequate assessment should include analysis of both images and time-activity curves.
6.3.1.1.1 Cortical Uptake
The first minute after radiotracer administration represents the vascular delivery phase. The next 2 min constitutes the parenchymal phase. Uptake in the kidney during this interval (between 1 and 3 min after radiotracer injection) is proportional to its function, using either tubular or glomerular agents.
6.3.1.1.2 Cortical Retention
The cortical retention of radiotracer, quantified by expressing renal counts at 20–30 min on the time-activity curve as a percentage of the peak uptake, is a measure of the rapidity with which the radiotracer is excreted by the kidney. As renal function deteriorates, the percentage retained increases. An apparent increase in retention may occur with urine stasis in the collecting system.
6.3.1.1.3 First Visualization of Collecting System
The interval between radiotracer administration and excretion of activity into the collecting system (pelvis and/or calyces) is a measure of cortical function. Delayed appearance of the collecting system is associated with impaired function.
6.3.1.1.4 Time to Peak
This parameter is measured from the time-activity curve, although an accurate estimate may not be possible in the absence of a peak, which is often the case in significant renal dysfunction.
6.3.1.2 Static Studies
Scintigraphy with 99mTc-DMSA or 99mTc-glucoheptonate is done between 3 and 24 h after radiotracer administration. It is usually used to detect renal parenchymal defects such as those of pyelonephritis, scars, and infarcts. Since only functioning tubular cells accumulate these radiopharmaceuticals, the total renal uptake is a measure of individual renal function. Relative renal function can be also measured.
6.4 Major Diseases
6.4.1 Renovascular Hypertension (RVH)
Approximately 3 % of hypertension is renovascular in origin. The incidence is higher in a selected hypertensive population and may be as high as 30–40 %. Renal artery stenosis generally is due to atherosclerotic plaques or fibromuscular dysplasia, the latter occurring in younger individuals. Significant stenosis that would trigger the activation of the renin-angiotensin system and lead to the development of renovascular hypertension has been defined as a reduction in intraluminal diameter by 50 % or greater. However, the degree of anatomically defined renal artery stenosis does not always correlate with the presence of renovascular hypertension.
6.4.1.1 Pathophysiology
The renin-angiotensin system serves in the maintenance of systemic blood pressure in such conditions as hypotension and shock. In significant renal artery stenosis, however, activation of the renin-angiotensin system is limiting a fall in GFR but causing systemic (renovascular) hypertension. Systemic blood pressure is maintained primarily by increase in vascular tone and retention of sodium and water, while a sharp reduction in GFR is prevented by increase in the glomerular capillary hydrostatic pressure.
Glomerular capillary hydrostatic pressure is modulated by the tone of the afferent and efferent glomerular arterioles. Increased tone in the efferent arteriole or decreased tone (increased flow) in the afferent arteriole raises capillary hydrostatic pressure and GFR, while decreased tone in the efferent arteriole or increased tone (decreased flow) in the afferent arteriole lowers GFR.
The first step in the activation of the renin-angiotensin system is the release of renin by the renal JG cells by several mechanisms though (1) signals from baroreceptors (“stretch” receptors) in the afferent arteriole modulated by prostaglandins, (2) chemoreceptor signals from the macula densa (located in the initial portion of the distal tubule) related to decreased sodium and chloride in the distal tubule and modulated by prostaglandins and adenosine, and (3) increased sympathetic activity due to activation of systemic cardiopulmonary and carotid sinus baroreceptors by hypotension [2, 3].
Renin released as a result of these stimuli converts circulating angiotensinogen, an alpha2 globulin produced by the liver, to angiotensin I, a decapeptide. Angiotensin I is then converted to the active octapeptide form, angiotensin II, by an angiotensin–converting enzyme (ACE), found in the vascular endothelium, and the bulk of this conversion occurs in the pulmonary vascular bed. Angiotensin II is also produced in the kidney. Angiotensin II is a powerful vasoconstrictor.
Angiotensin II raises systemic blood pressure primarily by increasing vascular tone and stimulating the synthesis and secretion of aldosterone from the zona glomerulosa of the adrenal cortex, which promotes sodium and water reabsorption from the renal tubules.
6.4.1.2 Scintigraphy for RVH
6.4.1.2.1 Basis
The scintirenographic diagnosis of renovascular hypertension is based on the demonstration of changes in renal physiology following the administration of an ACE inhibitor [4–6]. As noted above, angiotensin II, formed by the activation of the renin-angiotensin system, helps maintain GFR by increasing the tone of the efferent glomerular arteriole which, in turn, raises the glomerular capillary hydrostatic pressure. These changes are reversed by ACE inhibitors, which block the conversion of angiotensin I to angiotensin II. Consequently, there is a sharp drop in GFR and in proximal tubular urine flow.
Decreased GFR and tubular flow after the administration of an ACE inhibitor will result in decreased uptake and prolonged cortical retention of 99mTc-DTPA. Since renal blood flow generally is not significantly changed, 99mTc-MAG3 shows only prolonged cortical retention without decreased uptake. Rarely, uptake of 99mTc-MAG3 may actually decrease, presumably due to a fall in blood pressure below a critical level required to maintain perfusion in the stenotic kidney. The general principles of ACE inhibitor renography also apply to patients receiving chronic treatment with angiotensin II receptor antagonists [7].
6.4.1.2.2 Interpretation
Scintigraphic studies are generally interpreted by comparing a baseline examination with the one performed after the administration of an ACE inhibitor. Both the images and the time-activity curves are evaluated using the traditional parameters of function discussed earlier, and the following changes after ACE inhibition are considered significant for renovascular hypertension [6, 8]:
1.
Increase in cortical retention by at least 15 %
2.
Delay in collecting system visualization by at least 2 min
3.
Decrease in initial cortical uptake by at least 10 %
4.
Increase in time to peak by at least 2 min
6.4.1.2.3 Factors Influencing ACE Inhibitor Scintigraphy
ACE inhibitor renography is subject to a number of variables that may result in false-positive or false-negative studies.
1.
Hypotension or a marked change in blood pressure after ACE inhibitor administration is often associated with bilateral symmetrical renal retention of the radiotracer.
2.
Dehydration with or without diuretics.
3.
Chronic ACE inhibitor therapy may potentially lower scintigraphic sensitivity and should be discontinued before the test. Alternatively, if the ACE inhibitor cannot be discontinued, scintigraphy may be performed while the patient is on therapy. If renal function appears symmetrical, renovascular hypertension is unlikely and a baseline study need not be done. However, if function is asymmetrical, the ACE inhibitor should be discontinued before the baseline study.
4.
Aspirin and other nonsteroidal anti-inflammatory agents such as indomethacin may decrease the sensitivity of the test. These drugs decrease prostaglandin activity and therefore indirectly decrease renin-angiotensin activity. This is particularly true with the use of DTPA, and MAG3 is preferred in patients who take nonsteroidal anti-inflammatory drugs [9].
5.
Calcium channel-blocking drugs are commonly used in renovascular hypertension. Although their effect on GFR is not as pronounced as that of ACE inhibitors, these drugs have been implicated as a cause of false-positive studies [10]. The mechanisms responsible for this finding are not entirely clear. Perhaps a marked decrease in GFR resulting from the combined effect of both calcium channel blockers and captopril may explain the above findings.
6.4.2 Urine Outflow Obstruction
Urinary tract obstruction may be complete or partial, and it may occur at various locations including the ureteropelvic junction (UPJ), ureterovesical junction (UVJ), and bladder outlet. The clinical consequences are quite dramatic and predictable in an acute and complete obstruction, but not in a partial and chronic one, exemplified by UPJ obstruction in children. Chronic UPJ obstruction, however, may eventually lead to renal cortical atrophy.
Hydronephrosis may be due to obstruction or to such nonobstructive conditions as vesicoureteral reflux, urinary tract infection, and congenital dysmorphism. It may be temporary with spontaneous resolution in infants and young children, or intermittent, or progressive with eventual stabilization.
6.4.2.1 Diuretic Renography
Furosemide, used for the scintigraphic evaluation of urine outflow for diagnosis of urinary tract obstruction, and other loop diuretics block the reabsorption of sodium, chloride, and potassium in the thick ascending limb of the loop of Henle. Increased tubular sodium decreases water reabsorption by an osmotic effect. Additionally, decreased sodium reabsorption into the medullary interstitium reduces its osmolarity, which in turn reduces water reabsorption from the collecting tubules.
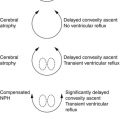
Diuretic renography [11–13] is based on the principle that increased urine flow resulting after furosemide administration causes rapid “washout” of the radiotracer from the unobstructed collecting system (Fig. 6.3), but delayed washout if obstruction is present (Fig. 6.4). While furosemide generally is administered intravenously after filling of the pelvocalyceal system, administration at the time of or prior to radiotracer administration also has been used. The washout half-time following diuretic injection is determined from the time-activity curve. A half-time of 10 min or less is considered normal, 10–20 min equivocal, and more than 20 min abnormal. However, overreliance on the washout half-time may not be justified because a number of factors may influence the diuretic renogram including renal dysfunction, dehydration, inadequate furosemide dosage, and atonic pelvis (redundant tissue).
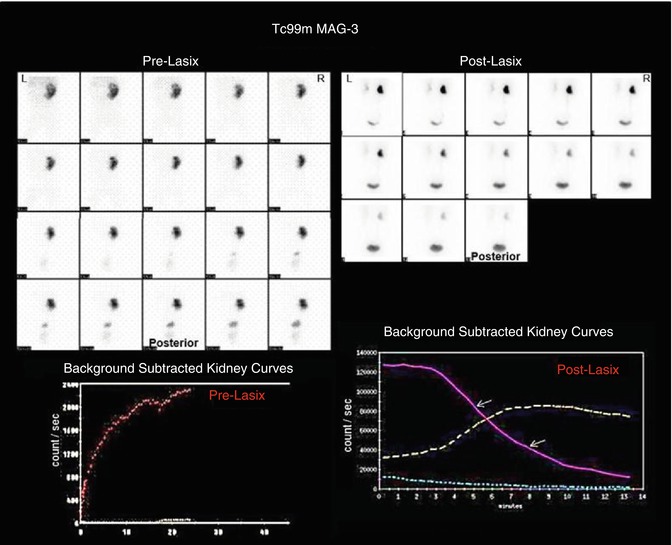
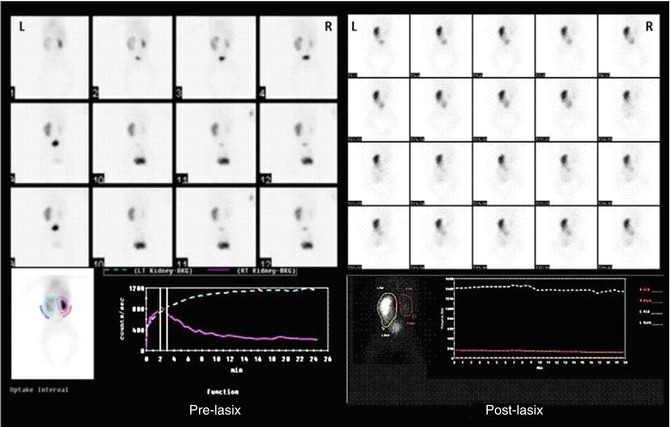
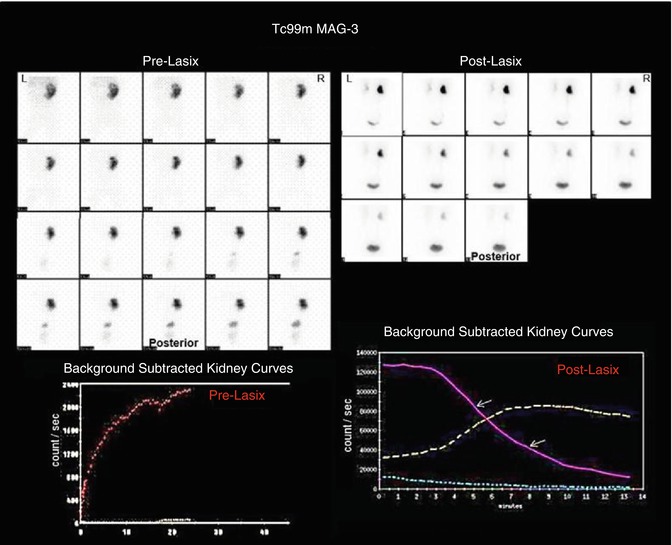
Fig. 6.3
A radionuclide diuretic renography study illustrating holdup of activity in the right functioning kidney by the end of pre-Lasix study with rapid washout on post-Lasix study which is clearly illustrated on the time-activity curve. These exemplify the nonobstructed pattern
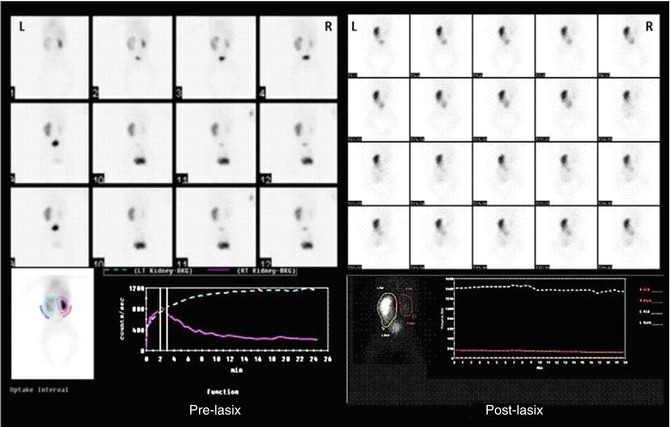
Fig. 6.4
A diuretic renography study in an adult patient illustrating obstructive pattern in the left side. Note the left kidney time-activity curve which shows no clearance before Lasix and no response to Lasix
A number of steps may be taken to optimize the radionuclide evaluation of urinary tract obstruction. Since preservation of renal function is the overriding concern, it has been suggested that evaluation of renal cortical function should be the primary focus of scintigraphic assessment. Additionally, since renal impairment or its progression is unpredictable, a single study in the infant with UPJ obstruction is of limited value. Instead, periodic scintigraphic assessments at intervals of 3 months are more desirable. Undue reliance on a single post-diuresis washout half-time also appears unwarranted for the reasons noted earlier. If methodology is standardized, periodic evaluation as for functional assessment may improve the predictive ability of the washout parameter as well. An increasing washout time probably is more meaningful than a single “positive” study [11].
6.4.3 Urinary Tract Infection
6.4.3.1 Pathophysiology
Urinary tract infections (UTIs) are particularly important in the pediatric age-group as it is one of the most common diseases in children. The overall incidence of UTIs in children ranges between 1.5 and 2 % [12, 13]. In the neonatal period, UTIs are relatively rare and are usually caused by bacteria from the blood stream. The incidence in newborns is higher for boys, while girls are affected (1 %) more than boys (0.3 %) between the ages of 1 and 5 years [12, 13]. The incidence increases up to 5 % among girls of school age. The most common age for UTIs in girls is 7–11 years, as a result of bacteria—usually a pathogenic strain of Escherichia coli—ascending the urethra.
Many predisposing factors affect the incidence and the severity of the disease in different age-groups. These factors include individual susceptibility, bacterial virulence, and the host’s anatomical abnormalities such as presence of vesicoureteral reflux (VUR), obstruction, stasis, or stones (Table 6.1). However, UTIs may occur also in healthy children with an anatomically normal urinary tract. Individual susceptibility may be variable and can be related to familial or hereditary factors.
Table 6.1
Factors predisposing to and affecting the severity of UTI in children
Individual susceptibility |
Bacterial virulence |
Host’s anatomical abnormalities |
Presence of reflux |
Obstruction and stasis |
Hydronephrosis with or without pelviureteral junction obstruction |
Horseshoe kidney |
Crossed renal ectopia |
Renal duplication with ectopic ureters |
Urethral polyps or diverticula |
Posterior urethral valves or ureterocele |
Chronic pyelonephritis results from recurrent or persistent renal infection. It occurs almost exclusively in patients with major anatomical anomalies, including urinary tract obstruction, renal dysplasia, or, most commonly, vesicoureteral reflux (VUR) in young children.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree