Figure 12.1.1
Unilateral renal agenesis. A: Transverse view of the fetal abdomen demonstrates the left kidney (arrowheads). No kidney is seen on the right. B: Coronal view of the abdomen demonstrates the left kidney (arrowheads). No right kidney is seen. C: Coronal view of the abdomen with color Doppler demonstrates the left renal artery (arrowhead) arising from the aorta (arrow). No right renal artery is seen. D: View of the abdomen in another fetus with unilateral renal agenesis demonstrates that, on the side with the absent kidney, the adrenal gland (arrowheads) is lying in a cephalocaudal orientation.
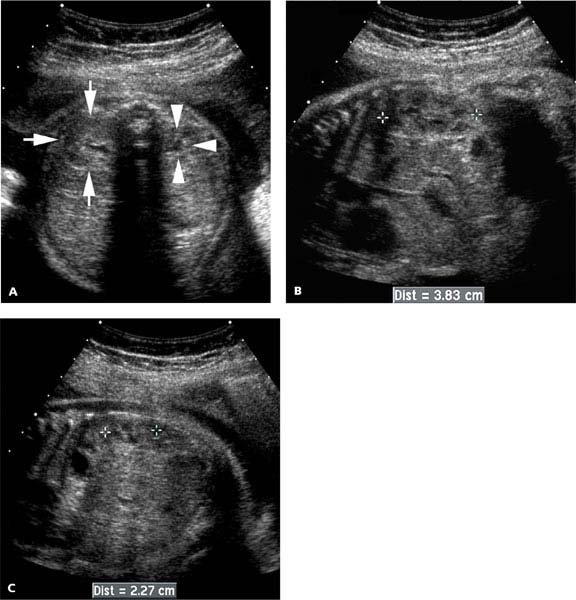
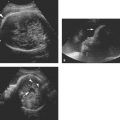
Figure 12.1.2
Unilateral hypoplastic kidney. A: Transverse view of the fetal abdomen demonstrates one normal-sized kidney (arrows) and one small kidney (arrowheads). Measurements (calipers) of the (B) right and (C) left kidney confirm the size discrepancy.
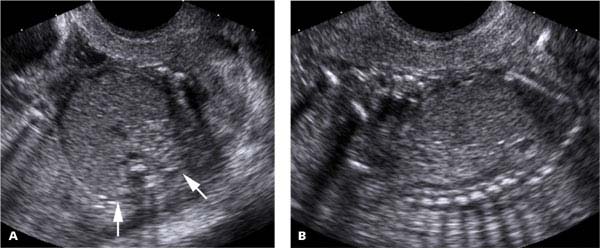
Figure 12.1.3
Bilateral renal agenesis. A: Transverse view of the fetal abdomen demonstrates no kidney in either renal fossa (arrows). There is no amniotic fluid seen around the abdomen. B: Sagittal view of the fetus demonstrates severe oligohydramnios, with virtually no fluid around the fetus.
12.2. Hydronephrosis: Overview
Description and Clinical Features
Hydronephrosis refers to dilation of the fetal renal collecting system. It can result from urinary tract obstruction, vesicoureteral reflux, or deficient musculature in the walls of the urinary tract and abdomen (prune belly syndrome). The most common site of urinary tract obstruction is at the ureteropelvic junction (UPJ). Obstruction may also occur within the ureter, at the ureterovesical junction, or in the urethra.
Sonography
Visualization of a small amount of fluid in the renal pelvis is a normal finding on a second- or third-trimester sonogram (Figure 12.2.1). Hydronephrosis is diagnosed when the collecting system is abnormally distended. More specifically, hydronephrosis should be diagnosed when the renal calyces are dilated (Figure 12.2.2) or the anteroposterior diameter of the renal pelvis (measured on a transverse view through the kidney) is 7 mm or more before 20 weeks (Figure 12.2.3), or 10 mm or more after 20 weeks gestation. Because hydronephrosis can develop at any time during pregnancy, it is prudent to label a kidney with a renal pelvis of 4–6 mm before 20 weeks or 5–9 mm after 20 weeks as possibly or borderline hydronephrotic. While most cases of borderline hydronephrosis resolve later in pregnancy (Figure 12.2.4), some cases progress to definite hydronephrosis (Figure 12.2.5).
When hydronephrosis is diagnosed, the contralateral kidney should be evaluated to determine whether the hydronephrosis is unilateral or bilateral. The renal parenchyma should be examined for evidence of dysplasia. Imaging of the ureters and bladder is important to determine the lowest extent of urinary tract dilation. The amniotic fluid volume should be assessed because the fluid volume provides information about urine output and renal function. A careful search should be made for other fetal anomalies because the presence of one fetal anomaly increases the risk of other anomalies and because of the possible association between hydronephrosis and trisomy 21.
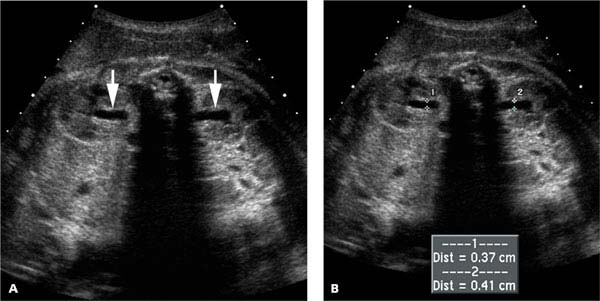
Figure 12.2.1
Normal fluid in the renal pelvises. A: Transverse view of the fetal abdomen at 36 weeks gestation reveals a small amount of fluid in the renal pelvises (arrows). B: The anteroposterior measurement of the renal pelvises (calipers) is approximately 4 mm on each side.

Figure 12.2.2
Hydronephrosis diagnosed on the basis of calyceal dilation. Image of a fetal kidney demonstrates calyceal dilation (arrowheads), as well as excess fluid in the renal pelvis (*).
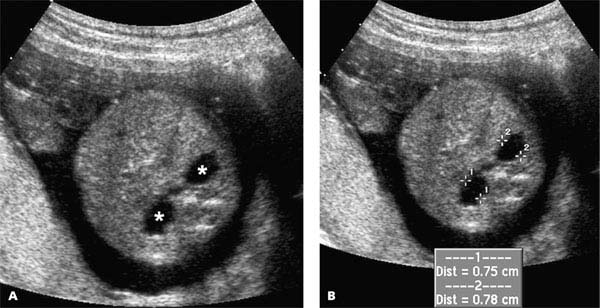
Figure 12.2.3
Hydronephrosis diagnosed on the basis of dilation of the renal pelvis. A: Both renal pelvises are fluid filled and distended (*’s) in this 19-week fetus. B: The anteroposterior diameters of the renal pelvises (calipers), measured on a transverse view of the abdomen, are 7.5 and 7.8 mm. Both measurements are abnormally large for this gestational age.
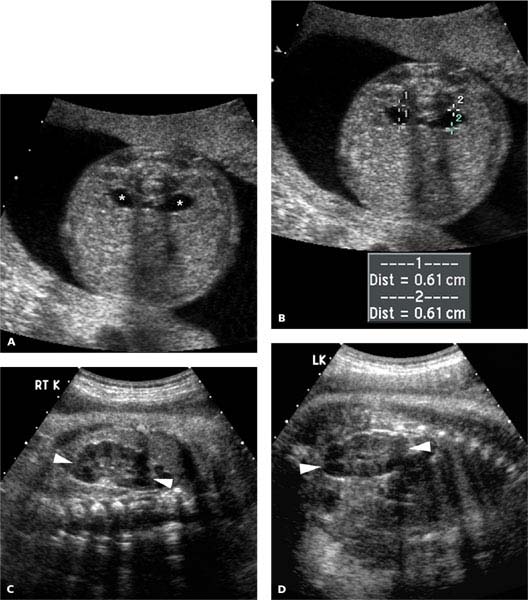
Figure 12.2.4
Borderline hydronephrosis that subsequently resolves. A: Fluid is seen in both renal pelvises in this 22-week fetus (*’s). B: The anteroposterior diameter of both renal pelvises (calipers) is 6.1 mm, representing borderline hydronephrosis. At 39 weeks, both (C) the right and (D) the left kidneys appear normal (arrowheads).

Figure 12.2.5
Borderline hydronephrosis that progresses to definite hydronephrosis. A: There is more fluid in the right renal pelvis (arrow) than the left (arrowhead) in this 19-week fetus. B: The measurement of the right renal pelvis, 4 mm, indicates borderline hydronephrosis, while measurement of the left side, 2.7 mm, is normal. C: At 32 weeks, there is definite hydronephrosis on the right, as evidenced by a 13.9 mm renal pelvis (calipers), and (D) caliectasis (arrowheads).
12.3. Ureteropelvic Junction Obstruction
Description and Clinical Features
Ureteropelvic junction obstruction, obstruction at the junction between the renal pelvis and the proximal ureter, is the most common cause of hydronephrosis in the neonate. It is bilateral in 30% of the cases and occurs more often in males than females. Progression to renal dysplasia is unusual but may occur if there is severe, long-standing obstruction.
Sonography
The sonographic diagnosis of UPJ obstruction is made when there is hydronephrosis without hydroureter. It may be either unilateral (Figure 12.3.1) or bilateral (Figure 12.3.2). The amniotic fluid volume is typically normal, but there may be oligohydramnios if the obstruction is severe and bilateral. Development of dysplasia in a kidney with UPJ obstruction is uncommon but should be suspected if the parenchyma is abnormally echogenic or contains cysts.
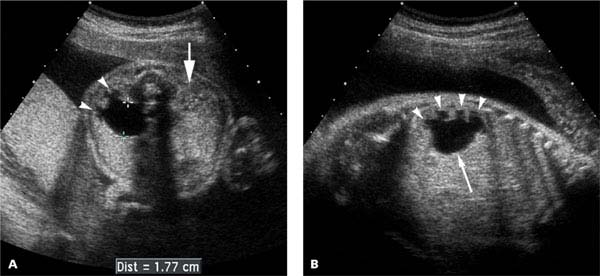
Figure 12.3.1
Unilateral ureteropelvic junction obstruction. A: Transverse view through the fetal abdomen demonstrates dilation of the renal pelvis (calipers), measuring 17.7 mm in anteroposterior diameter, as well as dilation of calyces (arrowheads) in the kidney. The contralateral kidney (arrow) appears normal. B: Coronal view through the abnormal kidney demonstrating dilation of the renal pelvis (arrow) and calyces (arrowheads), with no ureteral dilation.
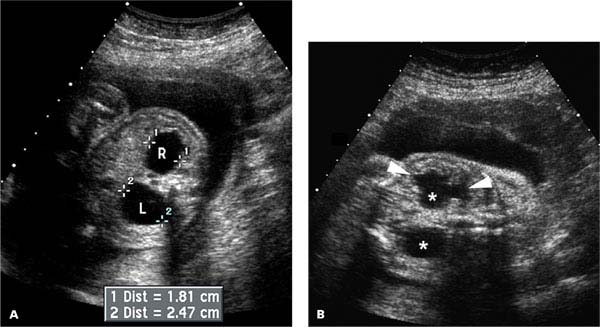

Figure 12.3.2
Bilateral ureteropelvic junction obstruction. A: Transverse view through the fetal abdomen demonstrates dilation of both renal pelvises, measuring 18.1 mm on the right and 24.7 mm on the left (calipers), and normal amniotic fluid volume. B: Coronal view of the fetal abdomen demonstrates dilated renal pelvises bilaterally (*’s), dilated calyces (arrowheads) in one of the kidneys, and no evidence of dilated ureters. C: The fetal bladder (arrow) is not distended. The combination of findings – bilateral dilated renal pelvises, nondilated ureters, nondilated bladder, and normal amniotic fluid volume – is indicative of bilateral UPJ obstruction.
12.4. Vesicoureteral Reflux and Primary Megaureter
Description and Clinical Features
Urine normally flows in a unidirectional manner through the ureter from the kidney into the bladder. Ureteral peristalsis propels the urine toward the bladder, and the shallow angle at which the ureter traverses the bladder wall is a configuration that acts as a valve preventing retrograde flow of urine from the bladder back into the ureter.
Two types of problems can arise in the ureter. First, reflux of urine from the bladder into the ureter can occur if the ureter has an abnormally steep, short course through the bladder wall. Reflux is often bilateral and is more common in males than females. Vesicoureteral reflux often resolves spontaneously in utero or within the first 1–2 years of life. If it is present at birth, the infant is at risk of urinary tract infections until it resolves. Appropriate management after birth, in most cases, is to treat with prophylactic antibiotics until resolution of reflux. Surgical correction is reserved for those cases that are severe at birth or fail to resolve.
The second type of problem that can affect the ureter is an abnormality that interferes with the flow of urine through the ureter. The most common such abnormality is an aperistaltic distal ureteral segment that causes a functional obstruction. This abnormality, termed primary megaureter, generally has a good prognosis. In mild cases, no intervention is required, and in more severe cases, it is correctable by surgical resection of the affected segment. Webs and strictures are less common ureteral abnormalities that can obstruct flow through the ureter.
Sonography
The prenatal sonographic findings of vesicoureteral reflux and primary megaureter are similar, both characterized by hydronephrosis and hydroureter (Figures 12.4.1 and 12.4.2). In severe cases, the ureter is markedly dilated and tortuous. Milder cases may be misdiagnosed as UPJ obstruction or missed altogether because the hydronephrosis or hydroureter can be intermittent.
The distinction between vesicoureteral reflux and primary megaureter cannot usually be made in utero, because these two entities have the same sonographic findings. Instead, the specific diagnosis is made after birth, by means of voiding cystourethrography and intravenous pyelography.
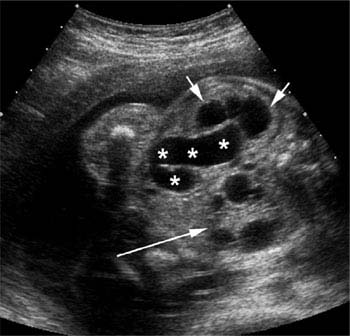
Figure 12.4.1
Primary megaureter. Transverse view through the fetal abdomen demonstrates dilated calyces (short arrows) and a dilated tortuous hydroureter (*’s), proven postnatally to represent a primary megaureter. The contralateral kidney is multicystic dysplastic (long arrow).
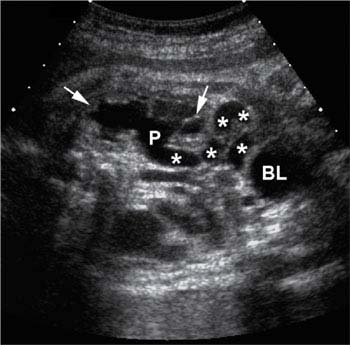
Figure 12.4.2
Primary megaureter or vesicoureteral reflux. Coronal view through the fetal abdomen demonstrates dilated calyces (arrows), dilated renal pelvis (P), dilated tortuous hydroureter (*’s), and normal-sized urinary bladder (BL). The fetus died shortly after birth, so distinction between primary megaureter and vesicoureteral reflux was never made.
12.5. Posterior Urethral Valves and Urethral Atresia
Description and Clinical Features
The major cause of urethral obstruction is posterior urethral valves, which occurs almost exclusively in males. Another cause is urethral atresia, which occurs in both males and females.
Prognosis is poor if the obstruction is complete, because the fetus is likely to have bilateral renal dysplasia and pulmonary hypoplasia. The latter occurs for the same reason that it does in fetuses with bilateral renal agenesis: lack of urine output leads to severe oligohydramnios and thereby to pressure of the uterine wall on the fetal thorax, which restricts pulmonary growth. Renal dysplasia occurs because the kidneys develop in the setting of high output pressure. In some cases, prognosis can be improved by prenatal treatment, percutaneously placing a shunt catheter from the fetal bladder to the amniotic fluid space.
Sonography
The sonographic findings that are consistently seen with urethral obstruction include bilateral hydronephrosis, dilated bladder, and oligohydramnios. Other findings that are often present include renal cortical dysplasia, bilateral hydroureters, thick bladder wall, and dilated posterior urethra, which appears as a projection from the bladder base (Figures 12.5.1 and 12.5.2).
The high pressure in the renal collecting system may lead to calyceal rupture. When this occurs, fluid is seen in the perinephric space (Figure 12.5.3) or as free intraperitoneal fluid (ascites).
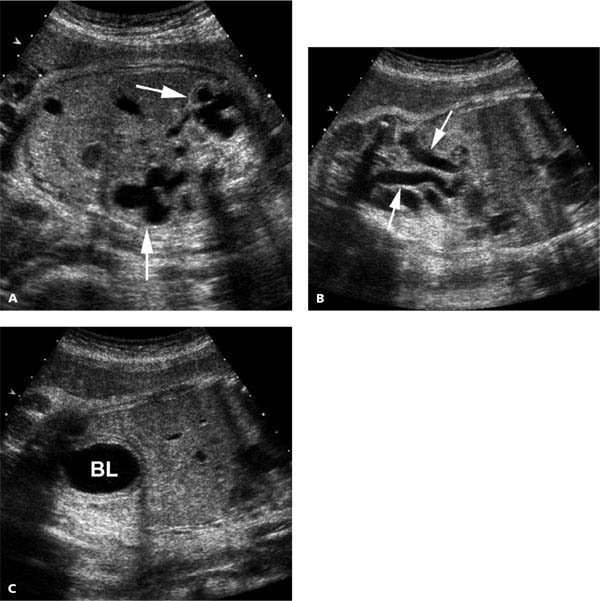
Figure 12.5.1
Posterior urethral valves. Views of the fetal abdomen at 32 weeks gestation reveal severe oligohydramnios and (A) bilateral hydronephrotic kidneys (arrows), (B) bilateral hydroureters (arrows), and (C) distended thick-walled bladder (BL).
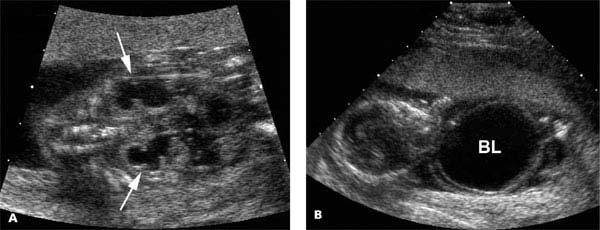
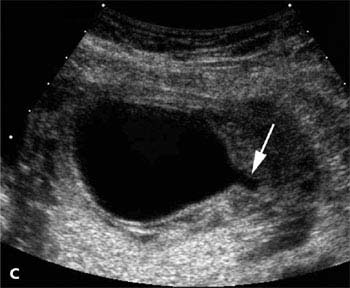
Figure 12.5.2
Posterior urethral valves with marked bladder distention. Views of the fetal abdomen at 17 weeks gestation reveal oligohydramnios and (A) bilateral hydronephrotic kidneys (arrows), (B) markedly distended bladder (BL), and (C) dilated posterior urethra (arrow) extending from the bladder.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree