Jean Noel Buy1 and Michel Ghossain2
(1)
Service Radiologie, Hopital Hotel-Dieu, Paris, France
(2)
Department of Radiology, Hotel Dieu de France, Beirut, Lebanon
10.1 Introduction
10.3.1 Pathology
10.3.3 Other Forms
10.4 Other Teratomas
10.4.1 Immature Teratoma
10.4.2 Mature Solid Teratoma
10.5.2 Different Types
10.6.1 Gonadoblastoma (Fig. )
10.6.2 Definition
10.6.4 Gross Examination
Abstract
In adults, 30 % of ovarian tumors are of germ cell origin [1]; the great majority of germ cell tumors (95 %) are benign and consist of mature cystic teratomas (MCT), usually designated dermoid cysts [2]. In children and adolescents, more than 60 % of ovarian neoplasms are of germ cell origin, and one-third of them are malignant [2–6].
10.1 Introduction
In adults, 30% of ovarian tumors are of germ cell origin [1]; the great majority of germ cell tumors (95%) are benign and consist of mature cystic teratomas (MCT), usually designated dermoid cysts [2]. In children and adolescents, more than 60% of ovarian neoplasms are of germ cell origin, and one-third of them are malignant [2–6].
In the majority of cases, diagnosis of MCT is relatively easy and the therapeutic approach roughly univoque. However, characterization of other types of germ cell tumors and especially primary malignant tumors can be much more difficult leading in some cases to a more complex management.
While most types of germ cell tumor occur in pure form, each of them may also be mixed with one or more other types. The prognosis of a mixed germ cell tumor generally reflects that of its most malignant element, but a small focus of high malignancy does not influence the prognosis as adversely as a large component [7].
10.2 Classification and Frequency
According to the WHO, there are two types of germinal cell tumors (Fig. 10.1, Table 10.1):
Fig. 10.1
Schematic representation of the origin of germ cell tumors. Dysgerminoma are constituted of cells that resemble primordial germinal cell. Other tumors are constituted of cells that resemble the different components of an embryo at 3 weeks. Polyembryoma is characterized by embryoid bodies
Table 10.1
Classification of germinal cell tumors
(A) Teratomas |
1. Mature cystic teratoma (B) usually pluritissular; almost always dermoid cyst |
2. Other teratomas |
∑ Other pluritissular teratomas |
– Immature cystic teratoma (M) |
– Mature solid teratoma or dysembryoma (B) |
∑ Monodermal and highly specialized teratoma: |
– Struma ovarii (usually B) |
– Carcinoids (low malignant potential) |
– Neuroectodermal tumors (B or M) |
(B) Primitive germ cell tumors (M) |
– Dysgerminoma |
– Yolk sac tumor |
– Choriocarcinoma |
– Embryonal carcinoma |
– Polyembryoma |
– Mixed malignant germ cell tumors |
Teratomas which contain tissues developed from one, two, or three germ cell layers. Mature teratomas contain adult-type tissues; immature teratomas contain embryonic-type tissues.
These different teratomas can be cystic, mainly cystic, mainly solid, or solid.
If the neoplastic tissue is uniformly mature, the tumor is designated mature teratoma.
The presence of any immature tissue warrants the diagnosis of immature teratoma.
An exception is a typical dermoid cyst at macroscopy that contains at microscopy tiny foci of immature tissue [7, p 267].
Primitive germ cell tumors from one germ cell type.
Figure 10.2 reports frequency of benign and malignant tumors according to the age, and Table 10.2 displays the frequency of the different types of tumors among the benign and malignant.
Fig. 10.2
Proportion of benign versus malignant germs cell tumors according to age
Benign | Malignant |
|---|---|
– Mature cystic teratoma >99% | – Dysgerminoma 50% |
– Mature solid teratoma <1% | – Yolk sac tumor 20% |
– Struma ovarii (usually benign) <1% | – Immature teratoma almost 20% |
– Mixed malignant germ cell tumor 8–10% | |
– Others < 2% | |
– Choriocarcinoma (most commonly part of a mixed germ cell tumor) | |
– Embryonal carcinoma | |
– Polyembryoma | |
– Carcinoid (low malignant potential) | |
– Neuroectodermal tumors (benign or malignant) |
10.3 Mature Cystic Teratoma (MCT)
MCT is the most common type of ovarian tumor [7]. Over 80% of MCT occur during the reproductive years [8], but they are also found in children and postmenopausal women. Ten percent are diagnosed during pregnancy [8].
Clinical Findings
1.
2.
When symptoms are present, abdominal pain occurs in 47% of cases, pelvic mass or swelling in 15% of cases, and unexplained abnormal uterine bleeding in 15% [9].
3.
Dermoid cyst can be discovered during a complication, i.e., mainly torsion, exceptionally rupture or infection (see Sect. 10.3.3.3).
10.3.1 Pathology
Almost all mature cystic teratomas are dermoid cysts. Dermoid cysts are defined by the presence of tissues in the wall which are ectodermal in origin and are formed by skin and its adnexa (sweat and sebaceous glands which excrete in the cyst sweat and sebum). In continuity with the inner wall of the cyst, there is in 80–90% of cases [11] a tissular portion named the Rokitansky protuberance which derivates from two to three germ cell layers (Fig. 10.3). For this reason, dermoid cyst is usually a pluritissular teratoma. Exceptionally dermoid cyst is monotissular [7].
Fig. 10.3
Surgical specimen of an 8-cm ovarian dermoid cyst. Typical aspect with three different components: (1) The cystic content made of fat intermingled with hair has been removed. (2) A regular thickened wall is seen; at microscopy, it contained an epidermoid epithelium and numerous skin adnexa. (3) A 4-cm Rokitansky protuberance lies against the inner wall of the cyst. It has a semilunar shape. It contains a bony and cartilaginous portion mixed with connective tissue. Hairs are extending from the protuberance into the cyst. Its inner border is regular
Exceptionally the wall of a MCT is formed by another tissue than skin, and in this case, only the term of MCT applies.
10.3.1.1 General Features
4.
6.
7.
While most of the dermoids are surrounded by normal ovarian parenchyma, in some cases they can have mainly an extra-ovarian development or even an elongated pedicle [12].
10.3.1.2 Macroscopy and Microscopy
The three main components of a MCT (Fig. 10.3) will be detailed separately:
1.
The wall is regular and measures in average from 2 to 3 mm in diameter. It is composed of connective tissue lined mainly by skin [2]. This skin is lined mainly by keratinized squamous epithelium.
2.
The Rokitansky protuberance is specific of a dermoid cyst.
Almost always [7], arising from its wall and projecting into its cavity, there is a protuberance composed of a mass of tissue, which contains derivatives from 2 to 3 germ cell layers:
(b)
(c)
Content:
Macroscopically: (Fig. 10.3)
(i)
The wall of the protuberance projecting into the lumen is formed by skin and is in continuity with the inner wall of the cyst.
(ii)
Tufts of hair are radiating from the protuberance into the lumen of the cyst.
(iii)
Most often, the inner part is tissular. It contains macroscopically recognizable structures: adipose tissue (2/3 of cases) often underlining the skin, soft tissue related to other types of connective tissue, and dense elements like cartilage with or without areas of calcification (38.6%), bone (18.6%), or more rarely teeth (8%) [8]. In some cases, the protuberance is partly cystic [2]. Exceptionally, an abortive attempt to form a fetus, characterized by one or more of these complex structures is referred to as a homunculus [7].
Microscopically it usually contains derivatives from (1) the ectodermic layer (99.3%) [8]: skin and cerebromeningeal structures which can secrete cerebrospinal fluid in the cavity; (2) the mesodermic layer (73.3%) [8]: bone, cartilage, muscle, fibrous, and adipose tissue; and (3) the endodermic layer (31.9%) [8], with its derivatives from the respiratory and GI endodermal epithelium, thyroid, and salivary gland tissue. Mucinous glands can be adjacent to the protuberance and form a little mucinous cyst.
(d)
Shape and situation: Most often it lies against the inner wall of the cyst; although it has roughly the shape of a vegetation, it has different macroscopic and microscopic features which are very helpful radiologically to distinguish it from a vegetation (Table 10.3). It can also be fingerlike or look like a nodule. More rarely, it lies in a septum. Exceptionally it forms a bridge between two parts of the wall (Fig. 10.4).
Table 10.3
Differentiation between a Rokitansky protuberance and a vegetation
Rokitansky protuberance | Vegetation | Vegetation | |
|---|---|---|---|
Benign | Borderline or malignant | ||
Size | 0.5–5 cm | Usually <1 cm | < or > 1 cm |
Border | Rather regular | Regular | Irregular |
Content | Adipose tissue and/or other tissues | Tissular proliferation | Tissular proliferation |
Tooth, bone, cartilage, or calcifications | Macrocalcifications | ||
Vessels | Few | Few | More numerous |
Thin | Larger (neovascularization) |
Fig. 10.4
Examples of two dermoid plugs. A classical dermoid plug (Rokitansky protuberance) lying against the inner border of the cyst is displayed in (a). An exceptional bridge shaped plug is displayed in (b)
(e)
Inner border: most often regular and more rarely slightly irregular
(f)
Malignant transformation: Malignant transformation occurs in 1–2% of MCT, most often in the dermoid plug but also can arise in the wall (see Sect. 10.3.3.4).
3.
The Content of the Cyst
According to the nature of the content, there are three different forms (Fig. 10.5):
Fig. 10.5
Schematic representation of the content of the cyst
Fat mixed with hair is the most common presentation. The skin which forms part of the wall secretes sebum and watery fluid more or less intermingled with hair. At body temperature, the contents are liquid but become solid at temperature below 25°C [13].
A purely cystic content can be related to a watery fluid coming from the sweat glands. Choroid plexus formation can be prominent enough to form a cystic structure filled with cerebrospinal fluid [12]. The liquid can be gelatinous, especially when the wall contains some amount of thyroid glands.
10.3.2 Isolated Noncomplicated Benign Mature Cystic Teratoma
Nowadays, most MCT are discovered on ultrasound. Occasionally the lesion is discovered during a plain abdominal radiograph or during an intravenous pyelography (Fig. 10.7). The most common finding is a calcification (a) that in the typical cases has a tooth shape; exceptionally the wall of the cyst is visibly delineated by intracystic and peritoneal fat (b).
Fig. 10.7
MCT discovered on abdominal films. The most common finding is a calcification (arrow in a). Rarely the cyst wall is visible because it is silhouetted by external peritoneal fat and intracystic fat (arrows in b)
10.3.2.1 US
Pitfalls in the Diagnosis
1.
Because of its property to strongly attenuate the US beam, a dermoid cyst may be confused with bowel and with a subserous leiomyoma. One must also remember that the exceptional lipoleiomyoma of the uterus may have a hyperechoic pattern that mimics a dermoid cyst.
2.
Some MCT cannot be detected on US [14] because of a high position that can be related to an elongated ovarian pedicle, or because they can be hidden by bowels, or associated pelvic pathologies such as multiple myomas or dense adhesions (Fig. 10.8) [15, 16].
Fig. 10.8
Small MCT not detected in ultrasound because of a huge myoma. US displays a large uterine leiomyoma. CT discloses a small right dermoid cyst containing fat and calcification
Conventional US and Doppler Findings
US and Doppler findings are summarized in Table 10.4.
Table 10.4
US and Doppler findings of mature cystic teratoma
Conventional US |
A. Content of the cyst |
Common |
1. Hyperechogenic ill-defined structure (dermoid mess) with a broad and ill-defined acoustic shadowing |
2. Hyperechogenic well-defined round structure (hair ball) with or without acoustic shadowing |
3. Hyperechogenic lines in a dark field |
4. Entirely hyperechogenic mass |
5. Fat-fluid level |
Uncommon |
1. Cystic mass |
2. Echogenic mass with a nonspecific echogenicity |
3. Multiloculated |
4. Unusual floating balls |
B. Rokitansky Protuberance (rarely identified) |
1. Against the inner wall |
2. Predominantly hyperechogenic |
3. May contain bright echogenic focus with sharp acoustic shadowing |
C. Wall of the Cyst (rarely delineated) |
1. Regular and thin |
Color Doppler |
1. Absence of flow in the cyst |
2. Absence of flow in the protuberance |
Cystic Content
The mass is usually round in shape, exceptionally oblong [17].
Characteristic Cystic Patterns
The aspect of the cystic content depends on the nature of the liquid and the amount of hair. The most characteristic and peculiar finding of MCT is the presence in the cyst of a hyperechogenic (echogenicity superior to myometrium) element which can have different patterns.
Six main patterns can be described. Each of them can be the only pattern of representation, but more often, some of them are associated, giving the mass a very typical aspect for a dermoid cyst [18]:
1.
A hyperechogenic ill-defined structure formed by multiple hyperechogenic and heterogenic pinpoint spots with or without a broad ill-defined acoustic shadowing [19] called by Malde et al. [20] the dermoid mesh. It is related at pathology to fat and hair gathered as tufts (Fig. 10.5, type 1; Fig. 10.9). The shadowing is more marked with a higher-frequency transducer.
Fig. 10.9
Dermoid cyst in a 41-year-old woman with central ill-defined hyperechogenic structure. (a) Ultrasound displays an echogenic mass containing a hyperechogenic structure made of dots or lines with some sound attenuation. (b) Pathologic specimen shows that the cystic content is composed of yellow fat with a center that contains brown fat and hair
2.
A hyperechogenic well-defined round structure without or with acoustic shadowing named on US as a hair ball. It is usually related at pathology to conglomeration of fat and hair as a ball shape (Fig. 10.5, type 2; Fig. 10.10), more rarely to conglomeration of pure fat (Fig. 10.11).
Fig. 10.10
A 50-year-old woman with a dermoid cyst that contains a hair ball and a cystic content looking like an endometrioma. (a) TAS shows a mass with a low echogenic cystic content and a hyperechoic structure with a broad acoustic shadowing in the dependent portion of the cyst. (b) On TVS with a higher-frequency transducer, the acoustic shadowing is more important
Fig. 10.11
Fat ball with US attenuation in a 44-year-old woman with a left ovarian dermoid cyst. (a) TAS shows an echogenic cystic mass that contains a round hyperechogenic mass wrongly considered as a hair ball, corresponding in fact to accumulation of fat. (b) In vitro US study shows a marked shadowing of this hyperechoic structure. (c) Pathologic specimen. Section through the cystic content shows yellow fat and brown fat without hair looking like a hair ball
In the same tumor, with a low-frequency transducer, the hair ball can be displayed without acoustic shadowing, while a higher-frequency transducer can demonstrate an acoustic shadowing.
3.
Hyperechogenic sparkling lines and dots in a hypoechoic field (Figs. 10.12, 10.13, and 10.14). They are related to hair in water [19] or fat (Fig. 10.5, type 3). The presence of these hyperechogenic lines in a ground-glass pattern helps in differentiating MCT from endometrioma.


Fig. 10.12
TVU of a left 5.6 × 4.5-cm MCT containing hyperechogenic sparkling lines in a hypoechoic field
Fig. 10.13
Dermoid cyst with a low echogenic pattern containing echogenic lines and a hyperechogenic focus against the wall (corresponding to the protuberance)
Fig. 10.14
Dermoid cyst with low echogenic cystic content and echogenic lines. (a) Sagittal TVS: The superior part of the cyst (left side of the figure) is nonechogenic, while the lower part (right side of the figure) is mainly low echogenic. (b) Transverse TVS through the lower part of the cyst demonstrates that it is diffusely low echogenic containing some hyperechoic lines
4.
A predominantly or entirely hyperechogenic mass as in 5/23 cases of Sheth et al. series [21] (Fig. 10.15). On CT, this form corresponds to a mass containing a small amount of fat intermingled with a larger component of hair [21]. This pattern is particularly common in small dermoid cysts (<3 cm) [22] (Fig. 10.7, type 4).
Fig. 10.15
Small dermoid cyst displayed as a hyperechogenic mass with acoustic shadowing. (a, b) Endovaginal US and b color Doppler: A 13-mm hyperechogenic mass with acoustic shadowing is very suggestive of a dermoid. Absence of vessel on color Doppler rules out a corpus luteum, but a corpus albicans could not be excluded. (c, d) CT scan is very useful in these cases and confirms the diagnosis (small cysts containing fat with a density of −90 HU)
Sometimes this form can be confused with a hemorrhagic cyst (Fig. 10.16). CT or MR allows to make the differential diagnosis.
Fig. 10.16
TVU displays a 3-cm hyperechogenic mass. CT confirms the presence of a small cyst containing fat and hair
5.
A fluid level
Usually the upper part is hypoechogenic, the lower part more echogenic (Fig. 10.17). Signification of this level has no clear explanation. It may be due to sedimentation, in fat that is fluid at body temperature, of cellular debris resulting from desquamation of the lining epithelium of the inner wall or simply a level between two different types of liquid like in an oil bottle.


Fig. 10.17
Dermoid cyst with fat-fat level. In vitro US study: (1) Hair ball: hyperechogenic focus with broad and ill-defined acoustic shadowing. (2) Fat-fat level
When isolated, this finding is not specific and can represent a hemorrhagic cyst. When an echogenic mass is floating at the interface, the aspect is characteristic (Fig. 10.17). Uncommonly, the upper part of the level looks more echogenic than the lower part (Fig. 10.18); this pattern described by Sandler et al. [17] and Owre et al. [23] is considered pathognomonic for a dermoid cyst [23].
Fig. 10.18
Sagittal TVU shows a MCT of 15 cm with a level formed by an upper echogenic fluid and a lower hypoechoic fluid. Hairs are seen in the hypoechoic fluid as hyperechogenic sparkle lines or foci. A hair ball is seen at the interface
6.
Unusual floating balls
A very uncommon presentation and at the same time very suggestive of the diagnosis of dermoid cyst is the presence in the cyst of multiple mobile spherical hyperechoic structures [24].
Nonsuggestive Cystic Patterns
(a)
Mainly or Exclusively Anechoic:
Purely anechoic (Fig. 10.19). Watery fluid (Fig. 10.5, type 6) can be demonstrated as an anechoic structure like in 2/23 cases of Sheth et al. series [21] and in 7/39 in Cohen’s series with enhanced sound transmission [17]. This anechoic fluid can be related to sweat glands contained in the wall or to cerebromeningeal structures in the protuberance. Differential diagnosis with a functional cyst or an epithelial tumor can be difficult.
Fig. 10.19
Anechoic 8-cm MCT of left ovary in a 3-year- and 4-month-old girl. The content of the cyst was anechoic on ultrasound and clear during surgery. At pathology, the wall was slightly irregular (1–3 mm) with some hairs
Mainly anechoic containing some echogenic lines (Fig. 10.20). Usually, the high echogenicity of these hair fibers in an anechoic pattern differentiates them from lower echogenic lines seen in the fishnet pattern of functional hemorrhagic cysts, but in some cases, the differential diagnosis may be difficult (Fig. 10.21).
Fig. 10.20
Almost anechoic 3.1-cm right ovarian dermoid cyst in a 52-year-old woman. The content of the cyst is anechoic except for some sparkle lines representing hairs in fat
Fig. 10.21
Twenty-centimeter MCT with hyperechogenic lines in an anechoic field. TAS in an anechoic cystic portion displays multiple hyperechogenic lines that resemble the fishnet appearance of functional hemorrhagic cyst. However, the lines are not usually so echogenic in a functional hemorrhagic cyst
Mainly anechoic with an echogenic portion. This echogenic portion is difficult to characterize as a Rokitansky protuberance or a vegetation or a tissular portion (Figs. 10.22 and 10.23).
Fig. 10.22
Right 9.5-cm MCT in a 19-year-old woman. (a) and (b) Ultrasound shows a right mass composed of a large anechoic loculation (in a) and a smaller hyperechoic component (in b). (c) CT scan without injection discloses a right dermoid cyst with fat, hair, and calcification
Fig. 10.23
MCT with a watery cystic content. (a) Sagittal TVS shows a left ovarian mass with a purely watery cystic content and an echogenic portion in the inferior part of the cyst. Diagnosis of MCT is not suggested. (b) CT scan without contrast. The cystic content has a mean density of 14 HU. Identification of the protuberance with calcifications and adipose tissue allows making a specific diagnosis of MCT
(b)
Hypoechoic Endometrioma-like Pattern. A hypoechogenic portion (less than myometrium) [21] with [19] or without acoustic shadowing. When there is no acoustic shadowing, this pattern can be confused with an endometrioma (Figs. 10.24 and 10.25). This low echogenicity on TVS can be depicted as anechoic on TAS. Sheth et al. [21] has demonstrated that this pattern on US corresponded more often on CT to low attenuation of pure fat (Fig. 10.5, type 5).

Fig. 10.24
Dermoid cyst with the cystic content resembling endometrioma

Fig. 10.25
EVS: left ovarian MCT resembling an endometrioma. At pathology, content of the cyst was watery fluid
(c)
Homogeneous echogenic (equal to myometrium) containing some hyperechogenic lines (Fig. 10.26). The main differential diagnosis is functional hemorrhagic cyst.
Fig. 10.26
Atypical form of MCT on US. EVS (a): homogeneous echogenic form containing some echogenic lines. Color Doppler (b) proves the mass is cystic. Differential diagnosis with a functional hemorrhagic cyst or an endometrioma is not possible
(d)
Heterogeneous echogenic mass (Fig. 10.27). The main differential is functional hemorrhagic cyst.
Fig. 10.27
Atypical MCT on US, CT, and MR. EVS: right ovarian MCT. Echogenic mass containing echogenic lines. Differential diagnosis with a hemorrhagic cyst is difficult. At pathology, content of the MCT was mastic
(e)
Exceptionally multiple hyperechogenic points on a diffusely echogenic background in cases of necrosis (Fig. 10.28).
Fig. 10.28
MCT complicated with necrosis. A 29-year-old woman operated through laparoscopy 1 year before for a left MCT during pregnancy. The right ovary could not be clearly visualized. Endovaginal ultrasound (a and b) with color Doppler (c). Right ovarian echogenic mass containing multiple hyperechogenic points without acoustic shadowing (a), pushing the normal ovarian parenchyma toward the periphery (b). Color Doppler confirms its cystic nature. The precise characterization of this echogenic cystic mass could not be established. On macroscopy, consistency of the cystic content was brown and pasty. On microscopy, the cyst was filled with keratinized material mixed with eosinophilic proteic substance containing a polypoid mass entirely occupied by necrosis
Multilocular Patterns and Multiplicity (Table 10.5)
Table 10.5
Differential diagnosis of multilocular cystic masses
Common |
–Mucinous tumor (benign, borderline, malignant) |
–Serous cystadenoma |
–Mature cystic teratoma |
–Endometriomas |
–Peritoneal pseudocyst |
–Pelvic inflammatory disease |
–Macrofollicular dystrophy |
–Ovarian hyperstimulation syndrome |
Uncommon |
–Granulosa cell tumor and Sertoli-Leydig tumor |
–Immature cystic teratoma |
–Struma ovarii |
–Hyperreactio luteinalis |
(a)
MCT are not infrequently multilocular. When one or several loculi have a pattern suggestive of a dermoid cyst, the diagnosis can be made easily (Figs. 10.29 and 10.30).
Fig. 10.29
Huge multilocular MCT of the right ovary (30 × 40 cm). A hyperechogenic round component with acoustic shadowing suggests the diagnosis of a dermoid cyst
Fig. 10.30
Atypical multiloculated dermoid cyst on US. TAS: multiloculated cystic mass containing liquids of different echogenicities. Echogenic lines and acoustic shadowing suggest the possibility of a dermoid cyst. However, this pattern is not considered as characteristic
(b)
In other cases, the mass can be very difficult to characterize and differentiate from other multilocular cystic masses (Fig. 10.31).
Fig. 10.31
Multilocular MCT, atypical on US, typical on CT. (a) TAS shows a multilocular cystic mass containing hyperechogenic foci with acoustic shadowing. Diagnosis of MCT is not suggested. (b) CT scan without contrast shows calcifications in the septa. Identification of fat in most of the loculi suggests the diagnosis of MCT
(c)
A MCT may be associated with another type of tumor in the same ovary (collision tumor), especially a mucinous tumor, which can be impossible to distinguish from a pure multilocular MCT (see Sect. 10.3.3.2).
(d)
Multiple in the same ovary: Diagnosis of MCT can be difficult because of the multiple areas of attenuation. Delineation of a MCT from another can be quite difficult (see Sect. 10.3.3.1).
Rokitansky’s Nodule or Dermoid Plug
It is a tissular portion in continuity with the inner wall of the cyst, more rarely lying in a septum exceptionally forming a bridge (Fig. 10.4). Dense elements (calcifications, tooth) contained in this dermoid plug can be barely seen in the hyperechogenicity of the cyst.
Several ultrasound patterns can be present:
1.
The dermoid plug is most often overlooked on US [16] because its echogenicity is very close to the echogenicity of the cyst Fig. 10.32.
Fig. 10.32
Dermoid cyst with difficulty to detect the protuberance. (c) In vitro CT study. Different contiguous 5-mm thick sections have been performed through the entire pathologic specimen demonstrating the protuberance in section (c). The protuberance appears very distinctly against the inner wall because its overall density is very different from that of the fatty and hair cystic content and because the tooth situated in the protuberance is clearly displayed. (a, b) US in vitro study (a, b) through section (c) using two needles placed in the same plane. A small focus, slightly more echogenic than the rest of the cystic content, associated with a focal acoustic shadowing is demonstrated. This focus that was demonstrated to be related to the protuberance has been hardly detectable on US and might be confused with a simple association of fat and hair. (d) Pathologic specimen: protuberance containing a tooth and fat intermingled with hair in the cyst
2.
Typical form
When it is individualizable, Rokitansky protuberance has been described as a predominantly hyperechoic portion [25] lying against the inner wall with or without a sharp acoustic shadowing. When the protuberance is larger than 2–3 cm, some of its components can be depicted. When a section is performed in the middle of the protuberance, in vitro US study has demonstrated that this hyperechogenicity is mainly located to the wall (Fig. 10.33). Inside, the connective tissue, mainly adipose tissue, appears low echogenic. Dense foci related to tooth, calcification, bone, or cartilage appear hyperechogenic with sharp acoustic shadowing (Fig. 10.34).
Fig. 10.33
US in vitro study of the surgical specimen (a and b) demonstrates a hyperechogenic focus with obtuse angles with the inner wall that corresponds to the dermoid plug (in a), containing a calcification with acoustic shadowing (in b). Section of the surgical specimen (c) performed in the same plane as US displays the protuberance with a regular contour, containing a focus of calcification
Fig. 10.34
Dermoid cyst containing a Rokitansky protuberance contiguous to a hair ball. (a) EVS: broad echogenic focus with sharp acoustic shadowing. (b) CT scan with coronal reconstruction. Fatty cystic content (d = −125 HU) and hair ball. The Rokitansky protuberance containing teeth is situated immediately below the hair ball
When a section is performed on the border of the protuberance, through the skin, Rokitansky protuberance looks hyperechoic like in Quinn’s description [25].
When it is small, it looks mainly hyperechogenic.
3.
Unusual forms:
Shape: Rokitansky protuberance can be seen in a septum, or can form a bridge. It can also have a fingerlike shape (Fig. 10.35).
Fig. 10.35
Dermoid cyst in a 41-year-old woman. (a) EVS: Rokitansky protuberance appears slightly more echogenic than the cystic content, with a fingerlike shape. (b) Pathologic specimen: Rokitansky protuberance has two main components: (1) A thickened skin in its wall with adipose tissue, (2) A small serous cyst
Aspect :
1.
Echogenic ball (Fig. 10.36).
Fig. 10.36
Dermoid cyst. Benign Rokitansky protuberance, typical on CT not detected on US. (a) TAS with color Doppler. Regular echogenic portion against the inner wall of the cyst, which cannot be recognized as a dermoid plug. No vascularization in this portion is displayed. An echogenic portion is visualized in the dependent part of the cyst. (b) CT: The protuberance is very clearly depicted with its different components: wall, adipose tissue, connective tissue, and teeth. Its size is 4 cm. Its round shape forming acute angles with the inner wall, its regular border expresses its benign character. A fat level is displayed
2.
Predominantly cystic (Fig. 10.37).
Fig. 10.37
MCT. Rokitansky protuberance with a cystic content. (a) In vitro US study: echogenic cystic content with acoustic shadowing typical for a MCT. The cystic portion against the inner wall with acoustic enhancement represents in fact the Rokitansky protuberance. (b) In vitro CT study: The cystic nature of the protuberance is not as well displayed. However, adipose tissue and calcification are better demonstrated
3.
Isoechoic with the cystic content with predominantly sharp acoustic shadowing (Fig. 10.38).
Fig. 10.38
Dermoid cyst. In vitro US study. Rokitansky protuberance: A more echogenic focus with sharp and narrow acoustic shadowing is displayed. Its echogenicity, very close to the echogenicity of the cystic content, makes its recognition difficult
4.
Hyperechogenic focus without acoustic shadowing (Fig. 10.39), one possible exploration is that the calcified elements may be too small, partially masked with the adjacent hair, or if they are in the cyst wall, they may merge with adjacent bowels [21].
Fig. 10.39
Dermoid cyst. Unusual form of Rokitansky protuberance on US. (a) TAS: hyperechogenic focus without acoustic shadowing. Echogenicity of the cystic content is not suggestive for a MCT. (b) CT after contrast: a small tissular portion lying against the inner wall contains a tiny calcification related to the protuberance. Fatty content. On color Doppler, no vascularization is usually displayed in the dermoid plug
When a hyperechogenic focus is demonstrated, it does not look always typical for a dermoid plug and can be confused with other elements of a mature cystic teratoma or with a clot or a vegetation [26] (Fig. 10.40). In these cases, CT is very helpful in identifying the protuberance (Figs. 10.40 and 10.41).
Fig. 10.40
Dermoid cyst with a Rokitansky protuberance looking like a vegetation on US. (a) Longitudinal TVS: A hyperechogenic focus with a narrow acoustic shadowing is considered as a vegetation in this anechoic cystic portion. (b) Color Doppler: No vessel is displayed in the echogenic portion. A diagnosis of epithelial tumor was suggested
Fig. 10.41
Dermoid cyst with a Rokitansky protuberance looking like a vegetation on US. (a) TAS: unilocular anechoic cyst containing an echogenic round formation lying against the inner wall looking like an endocystic vegetation. Localized thickening of the wall. (b) CT scan displays at this level a typical protuberance containing a tooth and adipose tissue. (c) Content of the cyst is watery fluid with an overall density of 15 HU on CT
In other cases, the dermoid itself, situated in another tumor such as an epithelial tumor, can be confused with a vegetation (Fig. 10.42).
Fig. 10.42
Collision tumor. Mucinous cystadenoma and MCT. (a) Left ovarian cyst containing an echogenic portion protruding in the cyst with some attenuation. (b) CT scan confirms the diagnosis of left MCT in a multilocular cyst. Septa are thin and regular suggesting a benign mucinous cystadenoma
Wall of the Cyst
The wall was identified in 13/25 (52%) cyst in Nicolet et al. series [27].
When identified, usually one part is depicted. It is most often hypoechoic (48%); hypoechogenicity seems to be related to a wall mainly formed of fibrous tissue. It is more rarely hyperechoic; hyperechogenicity seems to be related to a thick layer of adipose tissue [27].
Association of These Different Findings
These different patterns can be associated in the same tumor and in these cases are vey suggestive of the diagnosis (Figs. 10.43 and 10.44).
Fig. 10.43
Dermoid cyst with part of the cystic content resembling endometrioma. (a, b) Longitudinal TVS: content of the cyst (pure fat) can resemble an endometrioma (a) with a clot (b). (c, d) TVS demonstrates a hyperechogenic focus with a broad ill-defined acoustic shadowing (c) (fat and hair) and a hyperechogenic focus with sharp acoustic shadowing related to the protuberance (d). Association of these findings allows the diagnosis
Fig. 10.44
MCT of the left ovary measuring 5.6 × 4.5 cm with several patterns on ultrasound: (a) a hypoechoic background with sparkle echogenic lines; (b) a hyperechoic structure with acoustic shadowing; (c) a broad acoustic shadowing. An association of these findings allows making with confidence the diagnosis of MCT
Evaluation of Normal Ovarian Parenchyma
Dermoids completely surrounded by normal ovarian parenchyma have been reported [28].Usually until a certain size roughly less than 6 cm, dermoid pushes gently the normal parenchyma toward the periphery.
Color Doppler
1.
On color Doppler, the absence of vessel in the tumor allows to prove its cystic nature and to rule out solid benign and malignant masses [29, 30]. However, in some cases of benign tissular ovarian masses as ovarian fibroma and Brenner tumor, vascularization is not displayed on color Doppler (Table 10.6).
Table 10.6
Differential diagnosis of MCT with other echogenic masses using conventional US and color Doppler
Absence of vascularization on color Doppler: |
Echogenic cystic masses |
Functional hemorrhagic cyst |
Endometrioma |
Mucinous tumor [19] |
Tubo-ovarian abscess [18] |
Slight or absence of vascularization on color Doppler: |
Echogenic tissular masses (slightly vascularized) |
Ovarian fibroma |
Brenner tumor: |
High attenuation without calcification |
Vascularization: slight and central |
Significant vascularization on color Doppler: |
Subserous leiomyoma |
High attenuation without calcification |
Hypervascularization: peripheral ± central |
Ovarian carcinoma |
Ruled out by color Doppler |
3.
In the wall, vessels can be depicted in 24% of cases [31] but should not be confused with a vascularization in the protuberance (Fig. 10.45).
Fig. 10.45
(a, b): Dermoid cyst. Vascularization of the wall. (a) TVS: a small hyperechogenic focus with sharp acoustic shadowing is rarely visible because of its echogenicity close to the echogenicity of the cystic content. (b) TVS with color Doppler. Vessels are demonstrated in the wall of the cyst, in front of the base of the Rokitansky protuberance; on pulsed Doppler, RI is 0.61, PI 1, and peak systolic velocity 12 cm/s
Other Forms
Dermoids of Small Size (<3 cm)
1.
2.
Although, they have structural patterns very similar to those observed for large tumors, a predominantly hyperechoic appearance with or without acoustic shadowing is commonly observed [22].
In these cases, differential diagnosis with a corpus luteum cyst [15], an endometrioma, or a simple calcification can be very difficult. CT in this case is very helpful in making a definitive diagnosis (Figs. 10.46, 10.47, 10.48, 10.49, and 10.50).

Fig. 10.46
Small dermoid cyst. (a) TAS: 7-mm hyperechogenic round left ovarian lesion without acoustic shadowing. Differential diagnosis with a corpus luteum cyst can be discussed. (b) CT scan without contrast: the fatty content with a density of −69 HU allows to make a definite diagnosis of MCT
Fig. 10.47
Dermoid cyst. Unusual form of Rokitansky protuberance on US. (a) TAS: hyperechogenic focus without acoustic shadowing. Echogenicity of the cystic content is not suggestive for a MCT. (b) CT after contrast: a small tissular portion lying against the inner wall contains a tiny calcification related to the protuberance. Fatty content

Fig. 10.48
Dermoid cyst of small size. (a) EVS: left ovarian mass measuring 2.5 cm with a hyperechogenic focus with broad acoustic shadowing. (b) CT scan without contrast: a round calcification and the fatty content (−117 UH) definitely confirm the diagnosis
Fig. 10.49
(a) TAS: 2-cm hyperechogenic left ovarian mass, slightly heterogeneous with broad acoustic shadowing. (b) TVS: delineation with normal ovarian parenchyma is well depicted. (c) CT scan without contrast: a little tooth in the protuberance and fat intermingled with hair in the cyst definitely confirm the diagnosis of MCT
Fig. 10.50
Small MCT of 17 mm of the right ovary discovered after spontaneous abortion. EVS with color Doppler (a): The right ovary contains a well delneated mass, containing hyperechoic and anechoic portions; absence of color flow in the mass allows to precise its cystic nature. Although the diagnosis of dermoid cyst could be suggested in the differential diagnosis, a definite diagnosis could not not be established. On CT without contrast (b), presence of fat in the cyst allowed to definitely make the diagnosis of dermoid cyst hyperechoic
3.
Capsi et al. [34] demonstrated that dermoids <6 cm in diameter had a very slow growth pattern. Over a roughly 3 years’ period, the masses showed a growth rate of 1.8 mm/year in premenopausal women and a regression rate of 1.6 mm/year in postmenopausal women.
Pediatric Age
MCT accounts for about two-thirds of ovarian tumors in children [5].
In prepubertal girls, US findings are not as typical as after puberty [36]. Although MCT can show one of the findings considered as typical of ovarian teratoma, mural nodules and acoustic shadowing are seen in only 38 and 13% of lesions before puberty [36]. Approximately 10–15% are purely anechoic masses [37] (Fig. 10.51); at pathologic examination, these lesions unusually contain mural nodules less than 4 mm in diameter that are too small to be detected with TAS [37].
Fig. 10.51
MCT of left ovary in a 3-year- and 4-month-old girl measuring 8 × 7 × 5 cm. TAS transverse section (a): unilocular cyst with a regular thin wall entirely anechoic; on sagittal section (b) some declive echoes are displayed. While the diagnosis of a benign cyst could be established, at this age diagnosis of a dermoid cyst can only be suggested in the differential diagnosis. At macrocopy, the liquid was clear the wall was slightly irregular (1–3 mm) with some hairs
Pregnancy
In the past the most frequent means of diagnosis [9] were incidental at the time of delivery (Fig. 10.52). Cysts are not expected to increase significantly in size during pregnancy [35], and the incidence of torsion, hemorrhage, or rupture is not increased [8, 35].
Fig. 10.52
MCT in a pregnant woman. A 26-year-old pregnant woman at 10 weeks and 2 days of amenorrhea. (a) Intrauterine pregnancy. (b) Ten-cm hyperechogenic left adnexal mass with sound attenuation suggesting a MCT. Because of the large size of the cyst, a laparoscopy with cystectomy was performed. Follow-up was uneventful with delivery of a normal girl
Familial Ovarian Dermoids
Occurrence of ovarian dermoids in multiple women in the same family with a higher incidence of bilateral lesions has been reported [38]. The use of TVS in relatives of women with symptomatic dermoids may be warranted.
10.3.2.2 CT
As far as most of these tumors contain fat and hyperdense structures, CT has been proven to be the best imaging modality to detect and to characterize MCT as in 42 of 43 cases (98%) of our series [11]. Its pattern on CT is so characteristic that it is one of the diagnoses of characterization of ovarian tumors which can be made almost with certainty (Table 10.7). Their shape can be round or ovoid.
Table 10.7
CT findings of mature cystic teratomas
Noncontrast |
A. Content of the cyst |
Common: |
d <−20 HU (@90%): almost specific, related to fat intermingled or not with hair |
Uncommon: |
d >−20 HU: related to fat and large amount of hair or watery content |
Fat level |
B. Rokitansky protuberance |
Common: |
Unique |
Against the inner wall |
<5 cm |
Aspect of nodule or vegetation containing: |
Adipose tissue |
Calcification, bone, cartilage, tooth |
Regular border |
Uncommon: |
Multiple |
In a septum, forming a bridge |
Irregular border |
C. Wall |
Regular and thin |
After contrast |
Not very helpful |
Slight contrast uptake on delayed CT in the wall, the septa and the protuberance |
Cystic Content
Characteristic Form: Density <−20 HU
When the density is <−20 HU in at least one area of the cyst as in 93% [11] to 84% [39] of cases, the diagnosis of MCT is almost certain. Usually the mean density of the cyst is frankly negative from −40 to −148 HU (mean −109 HU) [11]. It corresponds at pathology to a fatty content more or less intermingled with hair, rarely to pure fat.
When fat is intermingled with hair, hair appears on CT as separated lines of soft tissue density in the fatty content (Fig. 10.3, type 3; Fig. 10.53), or as gathered lines forming tufts of hair (Fig. 10.3 type 1; Fig. 10.54), or as a round mass called a hair ball (Fig. 10.3, type 2; Fig. 10.55). Fat can also appear sometimes as multiple small rounded areas of low density (Fig. 10.56) [40], which can move by positional change [41].
Fig. 10.53
Dermoid cyst containing scattered hairs. (a) CT scan displays a 3-cm cyst with a fatty content intermingled with dense lines corresponding to hairs. (b) View of the surgical specimen demonstrates hairs arising from the cyst wall and hairs intermingled with the fatty content that has been removed and that is solid at room temperature
Fig. 10.54
Dermoid cyst with tuft of hairs. (a) CT scan displayed a cyst with fatty content and an irregular dense structure corresponding to hairs. (b) View of the surgical specimen shows hairs arising from the cyst wall and a tuft of hairs that has been removed from the cystic content
Fig. 10.55
Dermoid cysts with hair balls. Three hair-ball patterns are displayed at CT in three different dermoid cysts. (a) The cystic content is hypodense (−125 HU) and the hair ball contains a hypodense center. (b) In vitro CT study demonstrates a fluid level with an upper low-density fatty portion and a dependent high-density portion. A hair ball is floating at the interface with hair fibers intermingled with fat well depicted inside its center
Fig. 10.56
Cystic content containing small round fatty areas
Differential diagnosis: In very uncommon tumors such as solid mature teratoma [7], immature teratoma [7], and lipoleiomyoma [42, 43], fat can be present in some parts of the tumor.
When the content is purely fatty, it appears on CT with a density slightly inferior or equal to subcutaneous fat (−120 HU), which is almost specific for a MCT (Fig. 10.57). Only the very exceptional lipoma of the ovary [7] containing larger nodules of adipose tissue could be a differential although no such case has still been reported with an imaging modality.
Fig. 10.57
Dermoid cyst with pure fatty content. CT scan without contrast displays a 3-cm right ovarian cyst (arrow) with homogeneous low-density content without hair
Exceptionally, pure fatty content may be associated with a pseudo hair-ball pattern related in fact to different types of fat (Fig. 10.58).
Fig. 10.58
Fatty ball simulating a hair ball in a dermoid cyst. (a) CT scan without contrast shows a left ovarian cyst with a low-density fatty content and a round structure looking like a hair ball. (b) In vitro CT study shows a calcification within a Rokitansky protuberance and the round dense structure. At macroscopic examination, the cystic content shows yellow fat and brown fat without hair (see view of the surgical specimen in Fig. 10.11)
When a fluid level [44, 45] is present, the anterior nondependent portion has a far density, while the posterior dependent portion has a density > 0 UH. Sometimes a hair ball can float at the interface (Fig. 10.59), and exceptionally two levels may be seen in the same cyst (Fig. 10.60). The high density of the dependent part has no definite explanation as it has already been mentioned on US. This finding of fat-fluid level was present in only five of 40 patients (12.5%) of Buy et al. series [11].

Fig. 10.59
Dermoid cyst with a hair ball floating at the interface of a fluid level. CT scan displayed a 15-cm dermoid with a fluid level and a hair ball floating at the interface. Fat is well depicted in the anterior nondependent portion of the cyst, around the hair ball, and in the adipose tissue situated in the Rokitansky protuberance (arrow)

Fig. 10.60
Two-fluid level in a dermoid cyst. CT scan displayed a right ovarian cyst with two levels. The anterior part has a mean density of −124 UH. The posterior part has a mean density of 19 UH. The middle part has an intermediate density. At macroscopy, the cyst contained fat intermingled with hair. No Rokitansky protuberance was present
Nonsuggestive Pattern (Density > −20 HU)
Rarely, the density of the cystic content is ≥ −20 HU, and the diagnosis of MCT on CT is not possible based on the cystic content alone because fat is not present or could not be characterized in it. These cases can be grouped in three categories:
(a)
A very large amount of hair is mixed with fat resulting in a cystic density ≥ −20 HU. In a low percentage of cases mentioned by Friedman et al. [46] and in 3/24 MCT containing fat at pathology in Guinet et al. series [39], fat mixed with hair could not be recognized on CT because the mean density was comprised between −13 and 8 HU (Fig. 10.61).
Fig. 10.61
Atypical form of MCT with no low-density content on CT. CT scan with time-density curve demonstrates that the left ovarian mass is cystic with a density close to 10 HU. Preoperative diagnosis of MCT was not suggested. At pathology, a MCT was found containing fat mixed with hair
(b)
A cystic content, without fat and with a density close to water, made of a watery fluid (Fig. 10.62), resulting from sweat glands, cerebrospinal fluid excreted from meningeal structures contained in the protuberance [12], or gelatinous fluid. In 1/25 (4%) in Guinet et al. series [39] and in 3/41 (7%) in Buy et al. series [11], attenuation around 0 HU and from 17 to 35 HU respectively corresponded to watery and gelatinous fluid.
Fig. 10.62
MCT with a watery cystic content. CT scan without contrast. The cystic content has a mean density of 14 HU. Identification of the protuberance with calcifications and adipose tissue allows making a specific diagnosis of MCT
(c)
Exceptionally, the density is very high until 70 HU. We observed this pattern in some cases of gelatinous fluid (Fig. 10.63) or in dermoid cysts complicated with necrosis (Fig. 10.64). Necrosis can be isolated or secondary to torsion like in a case reported by Cederlund et al. [44].
Fig. 10.63
MCT or struma ovarii with very high-density cystic content. CT scan without contrast shows homogeneous unilocular cyst with a regular wall and a density of 72 HU. Diagnosis of MCT was not suggested prospectively. At macroscopy, the cyst contained a gelatinous fluid. At microscopy, the wall contained dense connective tissue intermingled with a loosely connective tissue with thyroid vesicles. In some slides, glial tissue was demonstrated. A final diagnosis of pluritissular MCT was established
Fig. 10.64
MCT complicated with necrosis in a 29 years old woman. CT scan without contrast demonstrates a right ovarian mass with homogeneous mean density of 64 HU. On macroscopy, consistency of the cystic content was brown and pasty. On microscopy the cyst was filled with keratinized material mixed with eosinophilic proteic substance containing a polypoid mass entirely occupied by necrosis, containing some cells filled with hemosiderin
Rokitansky Protuberance
Detection
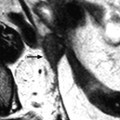
While the Rokitansky protuberance is most often overlooked on US, CT is the best modality to detect it (Fig. 10.65). Indeed, on CT, there is an excellent contrast between the content of the cyst and the Rokitansky protuberance that frequently contains tooth, calcification, or adipose tissue. In Buy et al. [11] series of 43 dermoid cyst, one or two protuberances in the same dermoid (total 43) were present at pathology in 36/43 (84%) cysts. CT detected 40/41 (98%) of benign dermoid plugs present at pathology and 2/2 dermoid plugs with malignant transformation.
Fig. 10.65
Dermoid cyst with Rokitansky protuberance overlooked on US and detected on CT. (a) Transverse TVU of a dermoid cyst shows an echoic content with sparkle lines and a hyperechoic focus with shadowing, situated on the internal wall of the cyst, representing probably tufts of hairs. (b) On CT, a Rokitansky protuberance containing adipose tissue and a calcification is well demonstrated on the lateral wall of the cyst
Characterization
Even when a mural nodule is detected on US, the Rokitansky protuberance can be confused with a vegetation, a clot, or a hair ball, while on CT its aspect is very characteristic (Fig. 10.66). It is even better demonstrated on CT than on MR (Fig. 10.67)


Fig. 10.66
Dermoid cyst with a Rokitansky protuberance looking like a vegetation on US. (a) TVU with Doppler displays an anechoic cyst containing an echogenic mural nodule looking like a vegetation. An epithelial tumor was suggested. (b, c) On CT without contrast: A calcification is clearly depicted against the inner wall, but the tissular portion of the Rokitansky protuberance is not visualized. However, the fatty cystic content (d = −154 HU) is typical for a dermoid cyst


Fig. 10.67
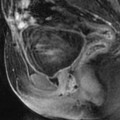
Dermoid cyst with Rokitansky protuberance, typical on CT, that could not be characterized with certainty on US and MR. (a) TAS with color Doppler displays a regular echogenic portion against the inner wall of the cyst which cannot be recognized as a dermoid plug. No vascularization in this portion is displayed. Echogenic material is visualized in the dependent part of the cyst. (b) On CT, the protuberance is very clearly depicted with its different components: wall, adipose tissue, connective tissue, and teeth. Its size is 4 cm. A fat level is displayed in the cyst. (c, d) On Axial MR T1-W image without (c) and with (d) fat suppression, the Rokitansky protuberance is not so well depicted as on CT: Hyperdense structures on CT with absence of signal on MR are much better characterized on CT as a calcification or a teeth. Adipose tissue in the protuberance cannot be detected with certainty. On the other hand, fatty cystic content with a fat level is well demonstrated
Features (Table 10.8)
Table 10.8
CT features of Rokitansky nodules in cystic teratomas of the ovary
Benign | Malignant | ||
|---|---|---|---|
Number | –Single | 26 | 2 |
–Multiple | 7 | – | |
Shape | –Oval or around | 37 | – |
–Bridge shaped | 3 | – | |
–Irregular | – | 2 | |
Content | –Adipose tissue | 24 | – |
–Calcification | 11 | – | |
–Tooth | 7 | 1 | |
–Hair | 18 | – | |
Inner border | –Regular | 39 | – |
–Irregular | 1 | 2 | |
Contrast uptake | – | 1 |
Shape
The protuberance lies almost always against the inner wall of the cyst and has the shape of a vegetation and a nodule and can be fingerlike, or very elongated (Figs. 10.68, 10.69, 10.70, 10.71, and 10.72). More rarely it is in a septum (Fig. 10.73). Exceptionally it forms a bridge between two parts of the wall (Fig. 10.74). When it has the shape of a vegetation, different radiological features allow to distinguish them one from the other.




Fig. 10.68
Dermoid cyst with a Rokitansky protuberance having the shape of a calcification
Fig. 10.69
Dermoid cyst with a Rokitansky protuberance having the shape of a vegetation. (a) CT scan displays a cyst containing fat and a hair ball. A Rokitansky protuberance is seen against the lateral wall, containing a calcification. (b) View of the surgical specimen

Fig. 10.70
Dermoid cyst with a Rokitansky protuberance having the shape of a nodule. With a thickened wall, calcifications, and adipose tissue
Fig. 10.71
Dermoid cyst with a fingerlike Rokitansky protuberance

Fig. 10.72
Dermoid cyst with a Rokitansky protuberance appearing as an elongated calcification. (a) On IVP, the elongated calcification is outside the ureter. (b–d) CT scan after contrast (b) and with coronal reformation (c, d).The calcification in the protuberance looks like a canine tooth
Fig. 10.73
Dermoid cyst with a Rokitansky protuberance in a septum. (a) In vivo CT scan: Rokitansky protuberance appears as a band of tissue containing a calcification. Soft tissue in contact is difficult to characterize. (b) In vitro study of the pathologic specimen
Fig. 10.74
Dermoid cyst containing a Rokitansky protuberance with a bridge shape. (a) CT scans without contrast. The Rokitansky protuberance is clearly depicted against the wall and extends as a bridge to another part of the cyst wall. A calcification is also displayed. (b) Pathologic specimen demonstrates nicely the protuberance
Structure
The wall of the protuberance clearly appears as a regular soft tissue density against the fatty content and forms with the inner wall of the cyst variable perpendicular acute or obtuse angles, which is not in agreement with previous descriptions [11, 25] (Figs. 10.75 and 10.76). Tufts of hair radiating from the wall of the protuberance into the cystic content can be demonstrated (Fig. 10.76).
Fig. 10.75
In vitro CT study of the Rokitansky protuberance of a dermoid cyst. The surgical specimen is immerged in water. The wall is clearly visible and forms on one side an acute angle with the wall of the cyst and a perpendicular angle on the other side. A large amount of adipose tissue is present in the Rokitansky protuberance with a density very close to the fatty cystic content
Fig. 10.76
In vivo (a) and in vitro (b) CT studies of a dermoid cyst with a Rokitansky protuberance. CT scan demonstrates at the best the Rokitansky’s protuberance. It appears as a 3- cm tissular portion with a regular border forming with the inner wall of the cyst variable angles. The architecture is very clearly depicted: wall, adipose tissue, tooth, and tuft of hairs
The content is most often tissular. Beneath the wall, adipose tissue is usually visualized either as a rim or occupying a more important component (Figs. 10.75, 10.76, and 10.77). Nonadipose connective tissue appears as a soft tissue density. Hyperdense structures related to bone, tooth, cartilage, or calcification are commonly present allowing in most of the cases a specific diagnosis. These hyperdense structures can occupy the entire protuberance (Fig. 10.78).Not uncommonly a small mucinous cyst is visualized adjacent to the protuberance sometimes in the cyst wall. Protuberances with an almost entirely cystic content are rare (Figs. 10.79 and 10.80).
Fig. 10.77
CT of dermoid cyst with Rokitansky protuberance and fat level. The Rokitansky protuberance has a well-defined wall and contains calcifications and a thin rim of adipose tissue. Fat displayed as fat level is well visualized in the adjacent cystic content
Fig. 10.78
Dermoid cyst anterior to the broad ligament with a Rokitansky protuberance almost entirely calcified. On CT, the Rokitansky protuberance appears almost entirely occupied by teeth. A tuft of hairs is nicely depicted, arising from its wall that is imperceptible
Fig. 10.79
In vitro US (a) and CT (b) studies of a MCT containing a Rokitansky protuberance with a mainly cystic content. The cystic nature of the protuberance is better displayed on US (a). Adipose tissue and calcification are better displayed on CT (b)
Fig. 10.80
Dermoid cyst with Rokitansky protuberance having a cystic content. (a) In vitro CT study: A typical dermoid cyst is displayed with fat and calcifications. The protuberance appears clearly with a focal hyperdense structure (related to cartilage at pathology), skin, and a cystic content close to 0 HU. (b) Pathologic specimen. Protuberance with a cystic content, cartilage, and its wall formed by skin is seen adjacent to a fatty cystic content with a loculation having a mucinous content
Inner Border
Inner border: regular or irregular
Vascularization
In most of the cases, this tissular portion is slightly vascularized. During the DCT, at the arterial phase, no vessel is visualized in the protuberance (Fig. 10.81), or small vessels are displayed. At the venous phase a moderate contrast uptake is visualized in the wall and in the protuberance. Diffusion of contrast medium is mainly seen on the delayed CT. In uncommon cases,when the protuberance contains a large portion of thyroid tissue, a high contrast uptake can be visualized at the arterial phase. In the exceptional cases of malignant transformation, at the arterial phase, tumoral vessels can be displayed in the protuberance; a significant contrast uptake can be seen at the venous phase (Table 10.8).
Fig. 10.81
Dynamic CT study of a Rokitansky protuberance. Dynamic CT scans before contrast (a) at the arterial phase (b) and at the parenchymal phase (c) with time-density curve (d). A typical dermoid cyst with fatty content and a Rokitansky protuberance is displayed
The Wall of the Cyst
CT much better than US depicts the entire wall. On noncontrast CT, it is clearly visualized; it is regular and thin measuring 2–3 mm. Rarely, calcifications are visualized in a part or all around the wall (Fig. 10.82).
Fig. 10.82
Bilateral atypical MCT on CT with calcifications. (a, b) CT scan without (a) and after (b) contrast. Bilateral ovarian mass with calcifications in the wall of the right one. Density of the cystic content in the right one is close to pelvic muscle, while density in the left one is close to urine. A slight contrast uptake is visualized in the wall of both masses. (c) In vitro CT study: right ovary: Calcifications are depicted not only in the wall but also in the cystic content; mean density of the cysts is 20 HU. Left ovary: A density close to 0 HU is displayed. Preoperative diagnosis was not suggested. At pathology, content of the right MCT was mastic, and content of the left one was watery fluid
On dynamic CT (Fig. 10.81), regular vessels are visualized at the arterial phase and slight contrast uptake is displayed at the parenchymal phase. This diffusion is also observed on delayed CT.
Analysis of the regularity of the entire wall and of the protuberance is fundamental. Indeed, carcinomas and carcinoids arise in the wall or in the protuberance. They can be detected on CT as a localized thickening of the wall (case 1 of Felberg et al.) [45] with eventually extracapsular extension (case 4 of Friedman) [46], which cannot be appreciated on US. Diffuse thickening of the wall with hemorrhage is very suggestive of torsion [47].
Association of These Findings
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree