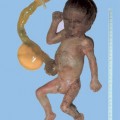
16 Growth Disturbance Definition: Birth weight above 4000 g or estimated fetal weight above the 95th centile for the given gestational age. It is important to differentiate between a constitutionally large fetus (“large for gestational age”) and a fetus with characteristic diabetic macrosomia (normal head circumference, increase in abdominal circumference, increased subcutaneous fat tissue). Incidence: 1–2% of births; if the percentile curves were correct, 5% of births would be detected. Clinical history: Genetically determined; parental heights. Pathological glucose tolerance test. Gestational diabetes. Macrosomia occurs frequently in consecutive pregnancies. Associated syndromes: Macrosomia is seen in Beckwith–Wiedemann syndrome, Weaver syndrome, and Sotos syndrome. Ultrasound findings: Fetal parameters, mainly the abdominal circumference, lie above the 95th centile. Estimating fetal weight, especially in macrosomia, is relatively inaccurate (maximum sensitivity 70%, positive predictive value 60 %). The abdominal circumference is possibly the best parameter for detecting macrosomia. The quotient of femur length and abdominal circumference (normally > 20%) is not a reliable parameter either (sensitivity 60%). Mild hydramnios is frequently present. Typically, the neck region and cheeks (cheek-to-cheek distance as measured using Abramowicz’s method) appear swollen, but this is due to fat tissue rather than edema. Clinical management: Glucose tolerance test, serial ultrasounds, possibly early delivery at 38 weeks of gestation. If the estimated fetal weight is above 4500 g, the benefit of primary cesarean section to avoid shoulder dystocia is disputed, as weight estimation in macrosomia is frequently not very accurate. Procedure after birth: A pediatrician should be present at delivery. Fetal distress and hypoglycemia are often observed. Prognosis: Normal, unless there are complications and injuries arising from delivery (for example, shoulder dystocia). References Benson CB, Coughlin BF, Doubilet PM. Amniotic fluid volume in large-for-gestational-age fetuses of non-diabetic mothers. J Ultrasound Med 1991; 10: 149–51. Best G, Pressman EK. Ultrasonographic prediction of birth weight in diabetic pregnancies. Obstet Gynecol 2002; 99: 740–4. Delpapa EH, Mueller HE. Pregnancy outcome following ultrasound diagnosis of macrosomia. Obstet Gynecol 1991; 78: 340–3. Elliott JP, Garite TI, Freeman RK, McQuown DS, Patel IM. Ultrasonic prediction of fetal macrosomia in diabetic patients. Obstet Gynecol 1982; 60: 159–62. Landon MB, Mintz MC, Gabbe SG. Sonographic evaluation of fetal abdominal growth: predictor of the large-for-gestational-age infant in pregnancies complicated by diabetes mellitus. Am J Obstet Gynecol 1989; 160: 115–21. Levine AB, Lockwood CJ, Brown B, Lapinski R, Berkowitz RL. Sonographic diagnosis of the large for gestational age fetus at term: does it make a difference? Obstet Gynecol 1992; 79: 55–8. Lurie S, Zalel Y, Hagay ZJ. The evaluation of accelerated fetal growth. Curr Opin Obstet Gynecol 1995; 7: 477–81. Miller JMJ, Brown HL, Khawli OF, Korndorffer FA, Gabert HA. Fetal weight estimatesin diabetic gravid women. JCU J Clin Ultrasound 1988; 16: 569–72. Miller JMJ, Kissling GE, Brown HL, Nagel PM, Korndorffer FA, Gabert HA. In utero growth of the large-for-menstrual-age fetus. JCU J Clin Ultrasound 1989; 17: 15–7.
Macrosomia
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree