≤5 Fr
6 Fr
≥7 Fr
Advantages
Smaller puncture
Smaller puncture
Increased support
Small vessel access
Small vessel access
Improved visualization
Radial access
Radial access
Increased torque
Deeper engagement possible for active support
Deeper engagement
Facilitate the use of 2 balloons (kissing)
Smaller quantity of contrast
Allows the use of any covered stent
Improved patient comfort
Disadvantages
↓ passive support
↓ support
Larger puncture site/recovery time
↓ visualization
↓ visualization
Less radial access possible
↓ torque
↓ torque
Pressure dampening
Device limiting (no thrombectomy, no simultaneous balloon inflation (kissing) technique possible, no Rotablator)
Device limiting
Increased contrast usage
Increased risk of ostial dissection
Passive vs. Active Support
In this chapter, we distinguish two types of support. Passive support is typically needed when deep active engagement of the coronary is not possible. Examples include the presence of a moderate left main lesion, aorto-ostial disease, or a severe proximal RCA lesion. In such situations, selection of a guide catheter curve and size that provides the best support despite few active manipulations will be desired. An additional situation would be for chronic total occlusion (CTO) PCI, when deep engagement is often not possible. Typically, larger bore catheters are stronger than smaller catheters and provide more passive support. For such reason, it is often possible, through 8-Fr guide catheters, to perform complex PCI in a calcified LAD lesion even with JL 4 curves. However, 6-Fr JL 4 guides will only provide poor support for such a purpose. Smaller guides are more easily manipulated for the active support maneuvers. They typically involve deeper engagement of the catheter, with push or rotation, to allow for delivery of the equipment. 5- or 6-Fr JR 4 guides can be actively rotated clockwise to engage the mid-RCA segment to allow for better support in case a distal lesion cannot be crossed with balloons or stents. However, some curves, even when used in 6 Fr, never allow for active engagement of the coronary and are typically used for passive support. This is the case of AL or AR catheters. Therefore, proper selection curve of the catheter, for passive or active support, will be crucial, especially when using 5- or 6-Fr guide catheters from the transradial approach.
Construction
Guide catheter construction differs between manufacturers and usually are very different from their diagnostic counterparts. A stiffer shaft, thinner walls, larger internal lumen diameter, a shorter and more angulated tip (110° vs. 90°), and a reinforced construction (3 vs. 2 layers) are some of the characteristics that differentiate guide catheters from diagnostic catheters. In fact, to allow passage of interventional devices, guiding catheters must have very thin walls (<0.12 mm or 0.005 in.) to achieve a lumen diameter at least twice that of a typical diagnostic catheter (2 mm or 0.076 in. vs. 1 mm or 0.038 in.) while maintaining good rotational response and avoiding kinking issues (Table 7.2).
Table 7.2
Internal diameters of standard, large, and giant lumen guiding catheters
French | Standard (in.) | Large (in.) | Giant (in.) |
|---|---|---|---|
6 | ≤0.061 | 0.062–0.065 | ≥0.066 |
7 | ≤0.071 | 0.072–0.075 | ≥0.076 |
8 | ≤0.079 | 0.080–0.085 | ≥0.086 |
9 | ≤0.089 | 0.090–0.096 | ≥0.096 |
10 | ≤0.099 | 0.100–0.107 | ≥0.108 |
Guiding catheters are generally composed of three layers. The outer layer is a soft nylon elastomer jacket composed of either polyurethane or polyethylene for overall stiffness. The smooth outer coating must also resist thrombus formation. The middle layer is a stainless-steel braid (wire matrix) for increased strength and torque generation. The lubricious PTFE inner coating is conceived for smooth passage of guidewires and balloon catheters. Additionally, to reduce the risk of vessel trauma or dissection during coronary cannulation of the non-tapered tip, most guiding catheters now also incorporate a very soft material in the most distal 2 mm of the catheter (Figs. 7.1 and 7.2).
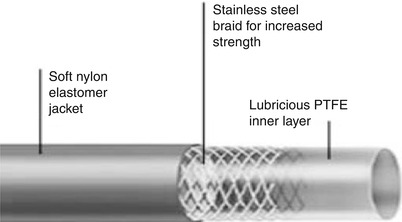
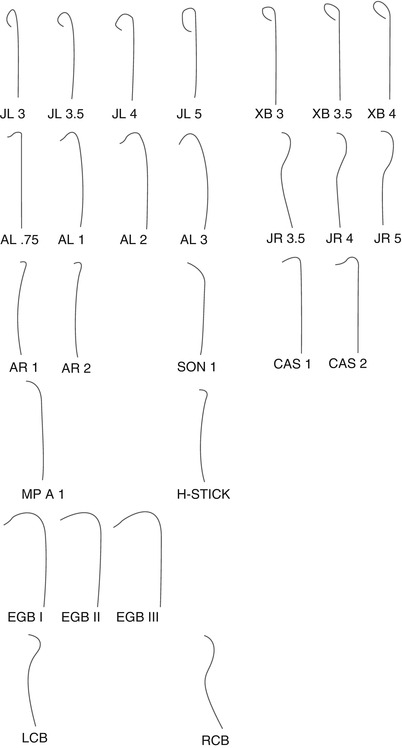
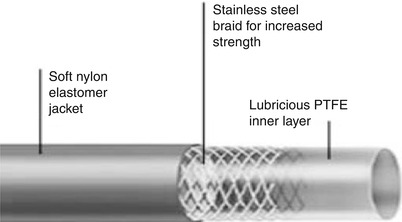
Fig. 7.1
Guide catheter construction
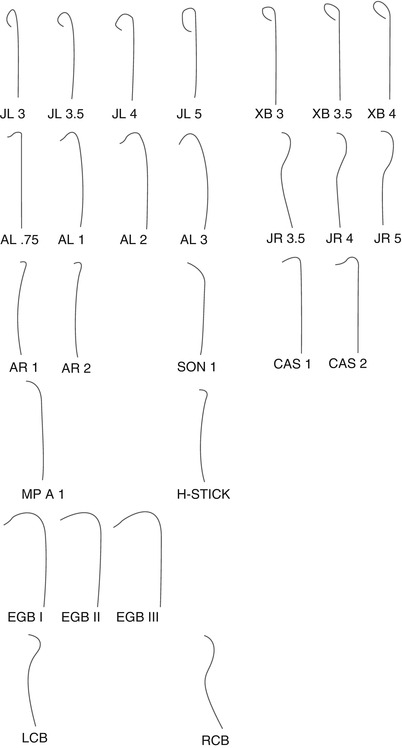
Fig. 7.2
Shapes of some of the most popular guiding catheters
Side Holes
Guiding catheter with side holes might be useful to secure pressure monitoring despite intubation of a diseased vessel (e.g., CTO PCI interventions) or when it is crucial to monitor the pressure throughout a risky procedure (like in left main interventions or while performing interventions on a unique surviving index artery). Side holes are mainly valuable to avoid catheter damping, to allow supplementary blood flow out of the tip to perfuse the coronary artery, and to help avoid dissection of the coronary ostium when the catheter is not perfectly coaxial or if it is engaged into a plaque, by allowing contrast to flow in the side hole and reduce risk of hydraulic antegrade dissection. On the other hand, the presence of side holes may give a false sense of security because the aortic pressure is monitored and not the coronary pressure. Therefore, the catheter can still occlude the coronary flow and induce ischemia but reduce recognition because the pressure curve on the monitor could remain normal. Other drawbacks of using side-hole catheters include increased contrast utilization, and suboptimal opacification of the index artery.
Also, measurement of coronary flow reserve (CRF) is dependent on the presence of side holes on the guiding catheter and on the vasodilator dose. In a small animal study published by Abizaid et al. [4], when CFR measurement was done with an 8-Fr guiding catheter without side holes, a maximum vasodilatory response was obtained using intracoronary adenosine dose of 12 μg. To the contrary, with side hole and 8- or 9-Fr guiding catheters, an approximate doubling of the adenosine dose was required to provoke a maximal vasodilatory response. Consequently, larger doses of adenosine should be given to assess coronary flow parameters when guiding catheter with side holes is used.
Transfemoral Interventions
From the femoral approach, in the presence of a normal aorta and a normal length of the left main, engaging the left coronary ostium is usually feasible with an Extra Backup (XB or EBU depending on the vendor), 4 in males and 3.5 in females, or Judkins left (JL) 4. Judkins diagnostic catheter is useful because its fixed primary curve permits to intubate only a little segment of the ostium of either the left main coronary artery or right coronary artery. Therefore, there is less risk of trauma to these vessels. On the contrary, when performing PCI, this fixed primary curve might cause a limitation because the Judkins catheter may not be oriented coaxially with the index artery. Moreover, the secondary curve of JL guiding catheters usually makes a 90° angle at the point of contact on the ascending aorta and has limited back wall support. Therefore, it may be difficult to deliver interventional devices through all the curves, and angles. Unless 7 or 8 Fr is used to increase passive support, the inability to effectively and coaxially engage a 5- or 6-Fr JL catheter make it unsuitable for complex LCX or LAD intervention, one exception being ostial left main intervention, where support is often less necessary and deep engagement is not preferred.
In the presence of a large aorta, it is preferable to upsize to an EBU 4.5 or JL 5 or to an Amplatz left (AL) 2–3 if a better support is needed. The AL guiding catheter is also valuable for the posterior and anterior left main takeoff and for interventions on a circumflex artery with a sharp angulation or abrupt downward origin from the left main. Amplatz catheters can be very valuable in providing Extra Backup passive support when proximal vessel tortuosity, chronic total occlusion, or a distal target lesion is present. Although ensuring a deep engagement with the coaxial alignment and a strong backup support for complex lesions, the AL catheter is a more aggressive and potentially traumatic catheter and must be manipulated cautiously to avoid vessel dissection, especially using 8-Fr size, where passive support will become maximized. In fact, just a simple withdrawal can advance the tip of the AL catheter even further into the coronary artery. Therefore, to disengage an AL catheter properly, one should advance the catheter slightly and then rotate it out of the ostium. If the ostium of the left main is high or the aortic root is small, a JL catheter may be selected, acknowledging the loss of passive support. Therefore, larger catheter could be favored to counteract this. If the left main is short, a short-tip guide may provide a better coaxial alignment, which can be verified in a left anterior oblique view.
The right coronary artery is usually more difficult to cannulate than the left coronary artery. The Judkins right (JR) 4 is usually a good guiding catheter for percutaneous interventions in the right coronary artery (RCA), in the presence of a normal aorta with a regular 90° origin of the RCA. With JR catheters, there is no point of contact with the aorta. Thus, this catheter customarily provides less passive support for right coronary interventions. When a stronger passive support is required, the AL 0.75 or 1 is a good alternative. With a large aorta, the Amplatz right (AR) 2–3 or the Hockey stick (HS) may be chosen by the operator. For a RCA superior takeoff, which means that the RCA points upward from the sinus, AL, AR, or HS catheters are decent choices. JR, JR short tip, Multipurpose, and the bypass right catheter are best for the inferior takeoff.
Shepherd’s Crook configuration (severe superior angulation and tortuosity) of right coronary artery represents a challenge for the interventional cardiologist. Effectively, studies have demonstrated that angioplasty of a RCA with a sharp upturn with a near-180° switchback turn is associated with a lower primary success rate, essentially because there is less support provided by the guiding catheter [5]. While JR catheter is particularly inadequate for this type of RCA anatomy, AL 1 or AL 0.75, SCR, Hockey stick, internal mammary, El Gamal, Voda right, or Multipurpose are best suited for this anatomy.
It may be demanding to easily cannulate the left internal mammary (LIMA) when using a femoral approach. This situation may occur because of proximal tortuosity of subclavian artery or acute angle between the subclavian artery and the LIMA. Moreover, because LIMA may be tortuous and extremely redundant, it can be very difficult to reach the culprit lesion with interventional devices. Interventions in arterial mammary grafts are usually performed with 90 cm internal mammary catheter, which offers contralateral wall support from the subclavian artery and is expressly designed to sit coaxially in the ostium of the internal mammary artery and allow for an extra 10 cm to the balloons and stents to reach the lesion. Since there is a high risk of dissection and spasm, forceful engagement of internal mammary artery should be avoided. Pretreatment with nitroglycerin or verapamil and frequent boluses of nitroglycerin may be used to minimize spasm. Finally, after balloon dilation, it is essential to assure that withdrawal of balloon catheter does not intubate the guiding catheter more deeply into the internal mammary artery, inducing a traumatic dissection.
Saphenous vein bypass grafts are often challenging to engage, particularly grafts to the obtuse marginal, which are usually located above and lateral to RCA grafts and may have superior angulation. Left coronary bypass (LCB) catheter, with a 90° primary bend and a 70° secondary bend, is specially designed for left coronary bypass grafts but often provides limited passive support. AL 1–2 offers a good backup force in such cases. The Multipurpose curve, the HS, or the right coronary bypass (RCB) catheter, which has a 120° tip and secondary bend, are nice options for grafts to RCA, which typically arise from the anterior wall of the aorta several centimeters above the aortic root and have horizontal to downward takeoff and direction. Multipurpose catheters may deeply engage a right graft; therefore, large 8-Fr catheters must be manipulated carefully. For grafts with abnormal takeoffs from aorta, especially inferior orientations, the Multipurpose guiding catheter might be useful.
Long Soft Tips Guide Catheters
Some catheters come in two versions: regular tip or longer soft tip. In our experience, the longer soft tip is associated with some compromise in terms of support. It allows to more easily engage the coronary, as its tip will bend before penetrating the ostium. Therefore, an operator can use such catheters placed in non-diseased proximal segments of the LAD or the LCX in the case of a short left main, to increase passive and active support, especially when using smaller equipment. However, if the selected catheter curve is too short, its soft tip will sit at the ostium of the left main or the RCA and will reduce passive support (Table 7.3).
Table 7.3
Choice of guiding catheters – transfemoral procedures
Target ostium | Guiding catheter (in order of preference) |
|---|---|
Left coronary artery | |
Normal aorta | EBU or XB 4, XB 3.5, JL 4, AL 2 (especially for LCX), |
Dilated aorta | XB ≥4, JL 5, AL ≥2, |
Narrow aorta | XB or EBU 3.0 or 3.5 (especially long soft tip), AL 1, JL 3.5 |
Superior/high takeoff | AL 2, AL 3, AL 4, JL 3.5, XB, EBU |
Inferior/low takeoff | XB 4, XB 3.5, Multipurpose, JL 4 MOD, AL 1.5 |
Posterior | AL 2 |
Anomalous circumflex | Multipurpose, AL 1 |
Right coronary artery | |
Normal aorta | JR 4, AR 2, AL 0.75 or 1, IMA, HS, |
Dilated aorta | JR ≥5, AL ≥2, AR ≥2 |
Narrow aorta | JR 3, AR 1, AL 0.75 |
Superior takeoff | AL 0.75 or 1, IMA, AR 2, HS |
Anterior origin | AL 1, Multipurpose, HS |
Posterior origin | AL 1, AR 2 |
Shepherd’s Crook | AL 0.75 or 1, HS, |
Saphenous vein graft | |
LCA graft | JR, LCB, AL 1, HS, Multipurpose, |
RCA graft | Multipurpose, RCB, |
Internal mammary artery | IMA, JR 4 |
Transradial or Brachial Interventions
Transradial interventions [6] are more technically demanding. However, they are becoming more widely used by interventional cardiologists who wish to reduce bleeding complications and increase patient comfort while decreasing staff workload compared to transfemoral interventions [7]. Ability of the patient to resume ambulation immediately after the intervention is greatly appreciated. However, the radial artery is one of the most spasm-prone in the human body. Mechanical stimuli can precipitate radial spasm. Consequently, reducing catheter manipulations will diminish the risk of radial spasm and thereby will cause less pain and will increase procedural success. Other drawbacks associated with transradial procedures are the inability to cannulate the radial artery, found in approximately 3–4 % of patients [8]; inability to cannulate the coronaries, which ranges in from 1 to 7 % [9]; and potential lack of guide support for coronary interventions [10]. Saito et al. [11] have measured by ultrasound a mean radial diameter of 3.10 ± 0.60 mm and 2.80 ± 0.60 mm in Japanese male and females, respectively. Consequently, 5-Fr introducer can be utilized in approximately 93 % of patients, 6-Fr in 85 % of men and 72 % of women, 7-Fr in 71 % of male and 40 % of female, and 8-Fr in 45 % and 24 %, respectively, if the objective is not to overstretch the vessel. However, currently, most transradial operators use 6-Fr catheters even in small radials.
Some of the characteristic features the guiding catheter should have when a transradial coronary intervention is performed include an optimal stiffness for optimal support, sufficient flexibility of the primary curve, contact with the aortic root, and a coaxial alignment with the target coronary artery. Guiding catheter manipulation differs between radial and femoral approaches. Some maneuvers facilitate guide positioning. The operator may ask the patient to take a deep breath to facilitate catheter movement and positioning of the wire into the ascending aorta. It is also valuable to use an exchange-length wire to avoid the need to recross the great vessels. Alternatively, some operators will leave the short 0.035’ J guidewire against the aortic valve during the exchange, with the use of a syringe with flush. The next catheter is then advanced without proximal guidewire control, until the back end of the wire exits the guide catheter with further advancement. Finally, when cannulating the left main, most cannulation of the left main involves pushing and counterclockwise rotation of the catheter, especially with XB or AL catheters.
When the procedure is performed from a radial or brachial access, the EBU or XB, JL, or Voda catheters are good options for the left coronary artery. However, when approaching from the right radial artery, it is helpful to use a curve 0.5 cm shorter than that employed in the femoral route with a comparable aortic root (i.e., EBU 3.5 or JL 3.5). For RCA interventions from the right radial artery, the JR catheter offers good engagement. On the contrary, procedures from the left radial artery can be achieved with conventional “transfemoral” curves. The AR catheter may also be used for RCA procedures, although the passive support of such catheter is limited. Therefore, we prefer the use of JR or Barbeau catheter for active support, especially when there is minimal proximal disease. However, when maximal passive support is warranted, AL curves are preferred. The AL 0.75 offers the advantage of good backup support while limiting deep seating of the catheter, which may become problematic with proximal RCA disease. AL catheters may also be advantageous for LCX interventions (Tables 7.4 and 7.5




Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree