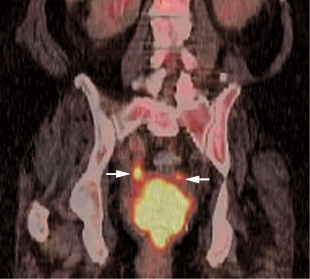
22 The primary value of positron emission tomography (PET) in cervical cancer is in diagnosis of extrapelvic disease in initial staging and in detection of recurrence. PET will detect the majority of primary tumors (Figs. 22.1 and 22.2), but is not as accurate as magnetic resonance imaging (MRI) for assessing locoregional involvement.3 The degree of uptake in the primary tumor at diagnosis negatively correlates with treatment response and prognosis.4 PET is useful in staging locally advanced untreated cervical carcinoma. There are conflicting data on the value of PET in early-stage resectable cervical cancer.5 Fig. 22.1 Metastatic cervical cancer. Coronal positron emission tomography/computed tomography scan demonstrates uptake in a primary cervical carcinoma (arrow) with multiple pelvic and retroperitoneal nodal metastases.
Gynecologic Tumors
Eugene C. Lin and Abass Alavi
 Cervical Cancer1,2
Cervical Cancer1,2
Primary Tumor
Clinical Indication: D
Staging
Clinical Indication: B
Accuracy and Comparison with Other Modalities
Body Region
Sensitivity %
Specificity %
Aortic nodes
84
95
Pelvic nodes
79
99
Pearls
- Urinary activity. Minimizing the effects of radioactive urine in the bladder and ureters is important in cervical cancer, as the specific areas of concern are the pelvic and para-aortic nodes (Fig. 22.2).
- Dual time point imaging. Dual time point imaging (an additional delayed 3-hour scan) increases accuracy in para-aortic lymph nodes, particularly inferior para-aortic nodes.17
Pitfalls
- In patients with early-stage disease, most of the false-negative results will be seen in the pelvis.
Table 22.2 Sensitivity and Specificity of Positron Emission Tomography (PET) versus Magnetic Resonance Imaging (MRI) in the Detection of Pelvic Nodal Metastases
Sensitivity %
Specificity %
PET
79
99
MRI
72
96
- In patients’ advanced stages of disease, more false-negative results will be noted in para-aortic nodes.
- Lymphangiography can cause false-positive nodal uptake.18
- A short axis diameter > 0.5 cm is the size threshold for accurate identification of metastatic lymph nodes from cervical cancer by PET/CT.16
- Lymphangiography can cause false-positive nodal uptake.18
Recurrence
Clinical Indication: C
Limited data suggest that PET is more sensitive than conventional imaging for recurrent cervical cancer. PET might be best employed in patients with better prognoses (e.g., determined by squamous cell carcinoma antigen levels and symptoms) and possibility of salvage therapies. In these patients, accurate determination of recurrence location can help decide between salvage therapy and chemoradiation.19,20
Accuracy and Comparison with Other Modalities
- PET. Sensitivity 96%, specificity 81%11
- Body region. The sensitivity for recurrence is poor in the lung, retrovesical, and para-aortic lymph nodes.21
- CT/MRI. PET is more sensitive than CT/MRI, but there is no difference in specificity.
- PET is more sensitive than CT/MRI for metastases (89% vs 39%), but there is no difference in local lesion detection.20
Pearls
- Symptoms. PET is useful in both symptomatic and asymptomatic women.22
- Squamous carcinoma antigen. PET is useful in detecting recurrence if serum squamous carcinoma antigen is elevated.23
Pitfalls
Focal rectal activity on PET is a possible cause of false-positive results for recurrent local disease.
Therapy Response and Prognosis
Clinical Indication: C
- Therapy response. There are limited data on the utility of PET for evaluation of therapy response in cervical carcinoma.
- Radiotherapy effect.24 Following irradiation, increased fluorodeoxyglucose (FDG) activity is common from inflammation; therefore, increased FDG activity is sensitive but nonspecific for active tumor.
- Neoadjuvant chemotherapy.25 Decrease in SUV correlates better with histological response than MRI in patients undergoing neoadjuvant therapy prior to radical hysterectomy.
- Radiotherapy effect.24 Following irradiation, increased fluorodeoxyglucose (FDG) activity is common from inflammation; therefore, increased FDG activity is sensitive but nonspecific for active tumor.
- Prognosis
- Pretherapy. A visual grading system, which incorporates the primary tumor size, its shape, the degree of nonuniformity of FDG uptake, and the level of pelvic or para-aortic nodal involvement by PET, can estimate prognosis.26
- Posttherapy. Persistent FDG uptake following therapy, particularly in para-aortic nodes, is a strong predictor of poor prognosis.27
- Pretherapy. A visual grading system, which incorporates the primary tumor size, its shape, the degree of nonuniformity of FDG uptake, and the level of pelvic or para-aortic nodal involvement by PET, can estimate prognosis.26
 Ovarian Cancer: Ovarian Masses1,2
Ovarian Cancer: Ovarian Masses1,2
Clinical Indication: C
PET has little role as a primary modality in the evaluation of primary ovarian masses.
- PET employed alone results in a substantial number of false-positive and -negative results.
- However, PET can complement the results of ultrasound and/or MRI findings and improve the overall accuracy of diagnostic imaging in patients with ovarian masses (as seen in Fig. 6.38).28
Accuracy and Comparison with Other Modalities
- PET. Sensitivity 58 to 86%, specificity 54 to 86%28
- Comparison: Table 22.328
Table 22.3 Sensitivity and Specificity of Positron Emission Tomography versus Other Imaging Modalities in the Evaluation of Primary Ovarian Masses
Sensitivity %
Specificity %
PET
58
76
US
92
60
MRI
83
84
Combined
92
85
Abbreviations: MRI, magnetic resonance imaging; PET, positron emission tomography; US, ultrasound.
Pearls
- Standardized uptake value. There is no established SUV threshold for distinguishing malignant from benign ovarian lesions: published values range from 3.25 to 7.9.29,30
- Visual threshold. One arbitrary visual threshold for malignancy includes any uptake equal to or greater than that of the liver.28
- Postmenopausal uptake. Ovarian uptake in the postmenopausal woman is much more worrisome than in a premenopausal woman, and malignancy should be strongly suspected.30
Pitfalls
- False-negatives. Low-grade tumors, early-stage ovarian carcinomas
- False-positives
- Inflammatory processes, endometriomas, benign cystic lesions (e.g., corpus luteum cyst, dermoid cyst, serous cyst), thecoma, physiologic uptake
- In premenopausal women, physiologic ovarian uptake is most common around ovulation and during the early luteal phase of the menstrual cycle.31 Physiologic ovarian uptake can be minimized by scheduling PET just after menstruation.
- Bowel or iliac node activity on PET can be difficult to differentiate from ovarian activity (as seen in Fig. 10.13, p. 111).
- Inflammatory processes, endometriomas, benign cystic lesions (e.g., corpus luteum cyst, dermoid cyst, serous cyst), thecoma, physiologic uptake
Recurrence
Clinical Indication: B
- PET is most useful when conventional imaging is inconclusive and cancer antigen (CA-) 125 is elevated.
- Second look laparotomy. Although PET is accurate in the diagnosis of ovarian cancer recurrence (particularly if used in conjunction with conventional imaging techniques), it is still limited because a second-look laparotomy is still necessary if recurrence is strongly suspected. The sensitivity of PET for small volume disease (< 1 cm) is low compared with second-look laparotomy.32 Despite this, PET can change management due to its high positive predictive value.33,34
- A positive PET scan can preclude the need for invasive surgical assessment.
- Tumor deposits large enough to be identified by PET may be considered for surgical resection because these lesions may not respond to chemotherapy.
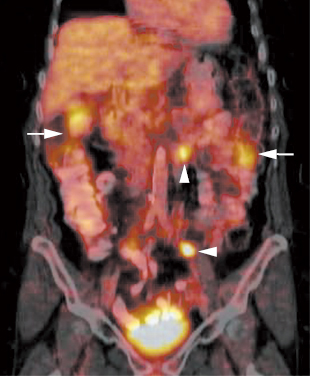
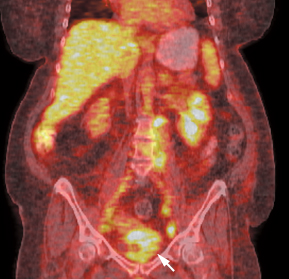
Fig. 22.3 Metastatic ovarian cancer. Coronal positron emission tomography/computed tomography (PET/CT) scan demonstrates both nodal (arrowheads) and peritoneal (arrows) metastases from ovarian cancer. PET has better sensitivity for nodal metastases than peritoneal metastases in ovarian cancer. (Courtesy of Carolyn Meltzer, MD, Atlanta, GA).

Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


- A positive PET scan can preclude the need for invasive surgical assessment.