Gynecology
QUESTIONS
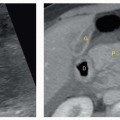
1a A 33-year-old female presents for evaluation of dysmenorrhea. Images of the left adnexa are shown. An ultrasound from 3 months ago showed a similar finding. Beta-hCG was negative. What is the most likely diagnosis?
|
A. Hemorrhagic cyst
B. Mature cystic teratoma
C. Endometrioma
D. Tuboovarian abscess
View Answer
1a Answer C. Images of the left ovary show a rounded mass with low-level homogeneous internal echoes, increased through transmission, and lack of vascular flow. These findings are characteristic of endometrioma. Endometriomas occur in females of menstrual age as a result of growth of endometrial tissue within the ovaries. The tissue undergoes repeated cyclical hemorrhage and forms cystic lesions containing degenerated blood products. The sonographic appearance of endometriomas can be variable, although approximately 50% of endometriomas appear as unilocular cysts containing low-level internal echoes. Other variations include multiloculated, mixed solid cystic, and, rarely, anechoic cystic morphologies. Although a cystic lesion containing homogeneous low-level echoes is the classic appearance of an endometrioma, this appearance can overlap with that of a hemorrhagic cyst. Therefore, a 6- to 12-week follow-up ultrasound is suggested when encountering a lesion with these characteristics for the first time in a patient of menstrual age to allow for the expected evolution of a hemorrhagic cyst.
A hemorrhagic cyst (choice A) is usually a complex cystic mass with a lace-like or reticular pattern of internal echoes due to interdigitating fibrin strands or a solid-appearing area with concave margins and no internal flow on Doppler ultrasound due to a retracting clot within the cyst. A mature cystic teratoma (dermoid) (choice B) usually contains hyperechoic components, lines and dots, and area of acoustic shadowing, with no internal flow at color Doppler sonography. Tuboovarian abscess (choice D) is commonly seen as a multilocular complex adnexal mass with internal echoes and septations.
1b Which of the following is the standard of reference in the diagnosis of endometriosis?
A. Hysterosalpingogram
B. CT
C. MRI
D. Laparoscopy
View Answer
1b Answer D. Although the diagnosis of endometriosis is suspected based on the history, signs, symptoms, physical exam findings, and imaging tests, laparoscopy is considered the gold standard for the diagnosis of endometriosis.
1c Malignant transformation is a rare complication (<1% of cases) of endometriosis. Which of the following is the most common malignant neoplasm arising from endometriosis?
A. Clear cell carcinoma
B. Clear cell sarcoma
C. Endometrioid carcinoma
D. Endometrial carcinoma
View Answer
1c Answer C. Endometrioid carcinoma is the most common malignant neoplasm arising from endometriosis followed by clear cell carcinoma.
1d Which of the following is the most commonly affected gastrointestinal tract area by endometriosis?
A. Cecum
B. Distal ileum
C. Appendix
D. Rectosigmoid colon
View Answer
1d Answer D. Gastrointestinal tract involvement is seen in 5% to 37% of patients with endometriosis. The rectosigmoid colon is the most commonly involved site followed by the small bowel, the cecum, and the appendix, in order of decreasing frequency.
References: Gore RM, Szucs RA, Wolf EL, et al. Miscellaneous abnormalities of the colon. In: Gore RM, Levine MS (eds). Textbook of gastrointestinal radiology, 3rd ed. Philadelphia, PA: Saunders Elsevier, 2008:1213.
Hertzberg BS, Middleton WD. Ultrasound: the requisites, 3rd ed. Philadelphia, PA: Elsevier, 2016:578-579.
Rumack CM, Wilson SR, Charboneau WJ. Diagnostic ultrasound, 4th ed. Philadelphia, PA: Elsevier Health Sciences, 2011:579-580.
Woodward PJ, Sohaey R, Mezzetti TP. Endometriosis: radiologic-pathologic correlation. RadioGraphics 2001;21(1):193-216.
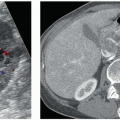
2a A 30-year-old female is undergoing infertility workup. 3D coronal US image of the mid to fundal uterus and transverse image through the lower uterine segment are shown. The imaging features are most consistent with which uterine anomaly?
|
A. Bicornuate
B. Didelphys
C. Septate
D. Arcuate
E. DES drug related
View Answer
2a Answer C. The images show two endometrial cavities with separation, which extends through the lower uterine segment and cervix. The main differential is between septate, bicornuate, and didelphys uterine anomalies. The 3D coronal image shows a single fundal contour, which extends above the interostial line. This key imaging feature excludes both bicornuate and didelphys anomalies, which are associated with a fundal cleft >1 cm. Arcuate uterus would be associated with a single uterine cavity. DES (in utero diethylstilbestrol exposure) uterine anomalies are associated with an atrophic, T-shaped uterine cavity.
2b What is the significance of distinguishing a septate uterus from other uterine anomalies?
A. Septate uterus is associated with congenital renal anomalies that should be diagnosed with additional imaging.
B. It is considered a normal anatomic variant that should have no effect on fertility.
C. Surgical correction can potentially improve reproductive outcomes.
D. Patients are at increased risk for vaginal clear cell carcinoma and should be screened.
View Answer
2b Answer C. In certain cases, surgical resection of the fibrous septation can improve obstetrical outcomes. Unicornuate, didelphys, and bicornuate uterus are associated with renal anomalies. Arcuate uterine configuration is considered a normal anatomic variant that has no effect on fertility and is not associated with renal anomalies. Patients with DES uterus are at increased risk for vaginal clear cell carcinoma.
References: Behr SC, Courtier JL, Qayyum A. Imaging of Müllerian duct anomalies. RadioGraphics 2012;32(6):E233-E250.
Chandler TM, Machan LS, Cooperberg PL, et al. Müllerian duct anomalies: from diagnosis to intervention. Br J Radiol 2009;82(984):1034-1042.
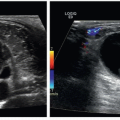
3 A 23-year-old female outpatient presents with obesity, anovulation, and hirsutism. The patient had a negative pregnancy test. What does the patient most likely have?
|
A. Ovarian torsion
B. Hyperstimulated ovaries
C. Polycystic ovary syndrome
D. Endometriosis
View Answer
3 Answer C. Both ovaries contain multiple small follicles that line up along the periphery of the ovary, the so-called string of pearls sign. Also, the ovarian stroma is prominent and echogenic. This appearance, along with the provided clinical history, is most consistent with polycystic ovary syndrome (PCOS). PCOS is an endocrine disorder characterized by hyperandrogenism and anovulation/oligoovulation due to high levels of luteinizing hormone (LH) and low levels of follicle-stimulating hormone (FSH). Clinically, women present with infertility, hirsutism, obesity, acne, and insulin resistance.
Ovarian torsion (choice A) is not the best choice because although there are multiple peripheral follicles as is often seen in torsion both ovaries look fairly symmetric. Patients with torsion present with pain and an enlarged ovary on the affected side. In torsion, the ovarian echotexture is often heterogeneous, different from this case where the echotexture is homogeneous.
Hyperstimulated ovaries (choice B) are usually markedly enlarged with multiple cysts, often with intracystic hemorrhage, ascites, and pleural effusions. Most often, this occurs in the setting of first-trimester pregnancy following ovulation induction for assisted fertility. The ovaries in this patient are only mildly enlarged, and the question stated that she is not pregnant.
Although endometriosis (choice D) can be a cause of infertility, it is not the best choice because no endometrioma is shown. Endometriomas usually have the appearance of complex ovarian cysts, often containing uniform low-level echoes. Other sonographic features include punctate echogenic mural foci, fluid-fluid levels, internal septations, multilocularity, and solid-appearing nodules due to clotted blood. The ovaries in this case have none of these sonographic features.
References: Hertzberg BS, Middleton WD. Ultrasound: the requisites, 3rd ed. Philadelphia, PA: Elsevier, 2016:580-589.
Lee TT, Rausch ME. Polycystic ovarian syndrome: role of imaging in diagnosis. RadioGraphics 2012;32(6):1643-1657.
4 A 26-year-old female presents to the emergency department after sudden onset of right lower quadrant pain, nausea, and vomiting. Laboratory values are as follows: WBC 8,500, beta-hCG negative. Images shown are from transvaginal ultrasound. Which of the following is the most likely diagnosis?
|
A. Oophoritis
B. Ovarian hyperstimulation
C. Polycystic ovarian syndrome
D. Ovarian torsion
View Answer
4 Answer D. The first image shows the left ovary, which is normal both in size and in morphology. The next image shows the right ovary, which is enlarged relative to the asymptomatic left side. In addition, the ovarian stroma is enlarged and heterogeneous, and the follicles are displaced peripherally. The imaging findings, along with the clinical presentation and laboratory values, are compatible with ovarian torsion (choice D). Clinically, patients with ovarian torsion present with acute onset of pain, often with nausea and vomiting. Intermittent pain may precede the acute episode by weeks. Ovarian torsion may present at any time in life, although relatively uncommon following menopause. The risk is increased during pregnancy. The most constant finding in ovarian torsion is unilateral enlargement of the torsed ovary. This is true even when the ovary shows Doppler flow, which is thought to be the result of dual blood supply to the ovary. The torsed ovary can, in fact, show arterial flow, venous flow, both, or neither. Therefore, in the appropriate clinical setting, an enlarged ovary should suggest torsion even in the presence of Doppler flow. Additional findings include heterogenous echotexture (from hemorrhage, edema, and necrosis), relative paucity of follicles, small peripheral follicles, echogenic rings around the follicles (follicular ring sign), twisted pedicle, whirlpool sign, and ovarian cyst.
Oophoritis (choice A) is not correct because of the clinical presentation. Although there can be relative asymmetric ovarian enlargement, oophoritis typically presents in the context of pelvic inflammatory disease, which has a different presentation of fever, cervical motion tenderness, and leukocytosis, which this patient does not have. Ovarian hyperstimulation (choice B) is incorrect because it typically involves both ovaries in a patient in the setting of first-trimester pregnancy following ovulation induction. This patient is not pregnant, and only one ovary is enlarged. Polycystic ovarian syndrome (choice C) is incorrect because of the acute presentation, which is not a feature of PCOS.
References: Hertzberg BS, Middleton WD. Ultrasound: the requisites, 3rd ed. Philadelphia, PA: Elsevier, 2016:580-582.
Rumack CM, Wilson SR, Charboneau WJ. Diagnostic ultrasound, 4th ed. Philadelphia, PA: Elsevier Health Sciences, 2011:584.
5 A 65-year-old female outpatient presents with postmenopausal bleeding and the following images on transvaginal ultrasound. Which of the following is the most appropriate next step for this patient’s management?
|
A. Follow-up ultrasound in 3 months to assess for resolution.
B. Send the patient for hysteroscopy and tissue sampling.
C. Send her to interventional radiology for embolization as this is a submucosal leiomyoma.
D. Send the patient for pelvic MRI for better characterization of the abnormality.
View Answer
5 Answer B. The first image shows an abnormally thickened endometrium with a solid mass containing cystic spaces. The second image shows Doppler flow within the mass. Based on the images shown and the clinical information provided, the best answer is B.
The patient is postmenopausal and presents with vaginal bleeding. According to a consensus statement by the Society of Radiologists in Ultrasound, an endometrial thickness of >5 mm in a woman with postmenopausal bleeding is abnormal. In a woman of this age group, the most likely causes are hyperplasia, polyps, submucosal fibroid, and carcinoma. The endometrium in this patient is clearly much thicker than 5 mm. In a postmenopausal patient, the endometrium is normally thin, homogeneous, and <5 mm. If the endometrium is thicker than 5 mm in a woman with postmenopausal bleeding, further evaluation with tissue sampling should be obtained. In a postmenopausal woman who is not bleeding, the upper limit of endometrial thickness is controversial, but a threshold of 8 mm (some suggest 11 mm) is advocated.
Choice A is not correct because the endometrium is clearly too thick to call normal in a woman of any age. Also, there is clearly a mass in the endometrial canal. Although submucosal fibroids (choice C) can cause bleeding, they are usually broad based, solid, hypoechoic masses with an outer layer of echogenic endometrium. This lesion is not completely solid and is isoechoic to the myometrium. Although the cystic components are more commonly present within polyps, they can also be identified within hyperplasia and carcinoma. Therefore, a tissue diagnosis is needed. Choice D is not the correct answer because imaging cannot reliably exclude carcinoma.
Reference: Hertzberg BS, Middleton WD. Ultrasound: the requisites, 3rd ed. Philadelphia, PA: Elsevier, 2016:541-546.
6 A 48-year-old woman presents with abnormally heavy menstrual bleeding, dyspareunia, and uterine enlargement on physical exam. Her gynecologist requests a pelvic ultrasound. The first image is transabdominal, and the second image is a transvaginal image. What is the most likely diagnosis?
|
A. Lipoleiomyoma
B. Adenomyosis
C. Intramural leiomyoma
D. Endometrial polyp
View Answer
6 Answer B. The first image shows an enlarged uterus with a bulbous configuration, with marked myometrial heterogeneity, especially along the anterior aspect. The second image (transvaginal) shows similar findings with multiple echogenic and hypoechoic linear striations, the so-called venetian blind appearance. Also note the indistinct interface between the endometrium and the myometrium. These findings are the result of adenomyosis. Adenomyosis is a common condition characterized by the presence of endometrial glands and stroma in the myometrium. These patients present with abnormally heavy vaginal bleeding, particularly at menses, dyspareunia, and an enlarged uterus. Very commonly, there is greater involvement in the posterior wall. Adenomyosis comes in two forms: diffuse, which is composed of widely scattered foci within the myometrium, and nodular, which consists of circumscribed nodules called adenomyomas. Ultrasound findings include an enlarged, globular uterus, disproportionate thickening of the posterior myometrium, myometrial cysts, heterogeneous echotexture, linear shadows (“venetian blind”) pattern, and indistinct myometrial-endometrial interface. MRI is highly accurate in the diagnosis of adenomyosis, which shows thickening of the junctional zone (>12 mm) on T2-weighted images, as well as poorly defined areas of decreased T2 signal in the myometrium.
Lipoleiomyoma (choice A) are rare, fat-containing, benign neoplasms that are well-defined, solid echogenic masses. Intramural leiomyoma (choice C) is incorrect because of the indistinct borders. Although they can have a variety of appearances and can also have the “venetian blind” appearance, they are well-circumscribed masses. Endometrial polyp (choice D) is incorrect because the images show that the abnormality is in the myometrium, not the endometrium. Also, polyps do not cause dyspareunia or globular uterine enlargement.
References: Hertzberg BS, Middleton WD. Ultrasound: the requisites, 3rd ed. Philadelphia, PA: Elsevier, 2016:550-553.
Rumack CM, Wilson SR, Charboneau WJ. Diagnostic ultrasound, 4th ed. Philadelphia, PA: Elsevier Health Sciences, 2011:559-560.
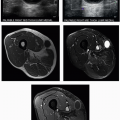
7 A 28-year-old woman underwent CT of the pelvis because of minor trauma. Bilateral ovarian masses were noted on the CT, and a pelvic ultrasound was recommended. Images shown are from transvaginal ultrasound. The most likely diagnosis is:
|
A. Endometriosis with bilateral endometriomas
B. Bilateral dermoid cysts
C. Tuboovarian abscesses
D. Bilateral hemorrhagic ovarian cysts
View Answer




7 Answer B. The first two images labeled “rt ovary” show a homogeneously echogenic mass within the right ovary. Attenuation of the ultrasound beam results in poor visualization of the deep portion of the mass, the “tip of the iceberg” sign. The second image shows shadowing deep to the mass. The next two images are labeled “lt ovary” and show a cystic lesion containing multiple echogenic, linear strands, the “dermoid mesh” sign. The second image of the left ovary also shows an echogenic mass with attenuation of the ultrasound beam deep to the mass. Therefore, the correct answer is bilateral dermoid cysts, choice
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree