Peritoneal Space, Retroperitoneum, Abdominal Wall, and Chest
QUESTIONS
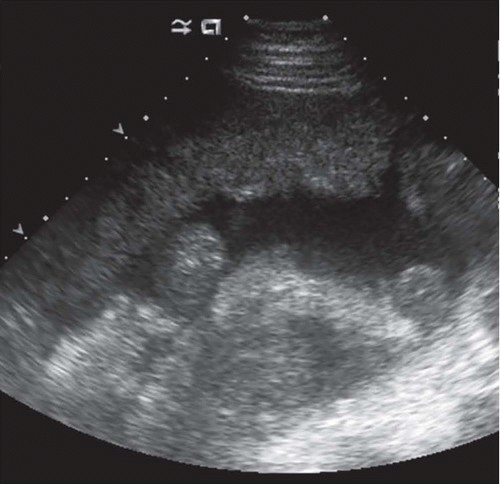
1a A 50-year-old male patient presents with abdominal distention. Transverse US image of the mid abdomen is shown. What is the most likely cause of the abdominal ascites?
|
A. Metastatic colon cancer
B. Cirrhosis
C. Splenosis
D. Mesothelioma
View Answer
1a Answer A. The image shows irregular peritoneal soft tissue thickening anteriorly and small volume abdominal ascites. In a male patient, metastatic disease from GI primary is the most common cause of peritoneal carcinomatosis. Although malignant mesothelioma could have a similar appearance, this condition is less common. Cirrhosis with associated portal hypertension is a common cause of ascites. Simple ascites from portal hypertension is not accompanied by peritoneal soft tissue mass as shown in this case.
1b Which of the following is considered a risk factor for peritoneal mesothelioma?
A. Asbestos exposure
B. Smoking history
C. Tuberculosis
D. Female gender
View Answer
1b Answer A. As in pleural mesothelioma, asbestos exposure has been shown to be a risk factor for peritoneal mesothelioma. Smoking is not a reported risk factor for mesothelioma. Tuberculous peritonitis is an infectious disorder, which may result in similar imaging findings including ascites, but is not considered a risk factor for mesothelioma. Mesothelioma is more common in men than women.
References: Diop AD, Fontarensky M, Montoriol PF, et al. CT imaging of peritoneal carcinomatosis and its mimics. Diagn Interv Imaging 2014;95:861-872.
Levy AD, Shaw JC, Sobin LH. From the archives of the AFIP: secondary tumors and tumorlike lesions of the peritoneal cavity: imaging features with pathologic correlation. RadioGraphics 2009;29:347-373.
Park JY, Kim KW, Kwon HJ, et al. Peritoneal mesotheliomas: clinicopathologic features, CT findings, and differential diagnosis. AJR Am J Roentgenol 2008;191:814-825.
2 A 39-year-old woman presents with pain and swelling over her c-section scar. The pain worsens during menstruation. The most likely diagnosis is:
|
A. Desmoid tumor
B. Suture granuloma
C. Hematoma
D. Scar endometrioma
View Answer
2 Answer D. The first image shows a hypoechoic, heterogeneous soft tissue mass with irregular margins in the abdominal wall at the site of c-section scar. The second image shows a feeding vascular pedicle entering the mass. The history and imaging features are characteristic of scar endometrioma.
Scar endometriomas most commonly develop following c-section or hysterectomy but have also been reported in laparoscopic trocar tracts, amniocentesis needle tracts, episiotomy sites, and in the vulva following excision of Bartholin gland cyst. Many patients with scar endometriosis do not have signs or symptoms of peritoneal endometriosis, leading many to believe that endometrial cells are transported to ectopic sites, particularly during surgical procedures that open the uterus. Women with symptomatic scar endometriosis present with a small, tender abdominal or pelvic wall mass at a previous surgical incision site—usually previous c-section, hysterectomy, or other gynecologic/obstetric procedure. Typically symptoms occur at the time of menses and include abdominal or pelvic wall pain and swelling. However, some patients are asymptomatic. Painful swelling may worsen during coughing and exertion and may be confused with postoperative hernia. Recurrent cyclical pain, a result of response to monthly ovulatory hormonal influences, is essentially diagnostic of scar endometriosis.
Desmoid tumors (choice A) are rare fibromatous lesions that do not metastasize but can be locally invasive and recur locally following surgery. They frequently occur at incision sites. They may be sporadic or associated with Gardner syndrome. Although there is overlap in imaging features with scar endometriosis, the clinical history of worsening pain during menstruation is typical of scar endometriosis, not desmoid tumor. Stitch granuloma (choice B) may have a similar imaging appearance and occur at the site of scar, but the history of worsening symptoms at menses is typical of scar endometriosis, not stitch granuloma. Hematoma (choice C) would be avascular and would not have a feeding vascular pedicle. The history is also not consistent with hematoma.
References: Gidwaney R, Badler R, et al. Endometriosis of abdominal and pelvic wall scars: multimodality imaging findings, pathologic correlation, and radiologic mimics. RadioGraphics 2012;32(7):2031-2043.
Hertzberg BS, Middleton WD. Ultrasound: the requisites, 3rd ed. Philadelphia, PA: Elsevier, 2016:213.
3 A 86-year-old male with a history of usual interstitial pneumonia (UIP) pattern pulmonary fibrosis was incidentally found to have a new right lung nodule on a radiograph and CT scan of chest. Shown here is an image from ultrasound of the right chest demonstrating the nodule. What is the next best step in management of the nodule?
|
A. The appearance is classic for pleural effusion. No biopsy is required.
B. The sonographic appearance is nonspecific, and ultrasound-guided biopsy should be performed to assess for possible malignancy.
C. The patient should be transferred to a CT suite as lung masses cannot be biopsied under ultrasound guidance.
D. The sharply defined deep margins suggest consolidation. Treat with antibiotics.
View Answer
3 Answer B. The sonographic appearance is not classic for effusions, consolidation, or atelectasis. The sharply defined deep margins are suspicious for a lung tumor. Pleural-based masses, especially the larger ones, if visible at ultrasound, can be safely and quickly biopsied under ultrasound guidance. Ultrasound-guided percutaneous biopsy in this patient revealed small cell carcinoma of the lung.
Choice A. The lesion is not anechoic to convincingly suggest an effusion. Also, the lobulated margins of the lesion argue against a collection.
Choice C. When visible, pleural-based lung masses can be biopsied under ultrasound guidance. In fact, ultrasound-guided biopsy not only is safe but also has additional advantages over CT scan. These include lack of ionizing radiation, ability to continuously visualize biopsy needle in real time during respiration, and the option to choose from multiple angles of needle trajectory.
Choice D. The well-defined deep margins of the lesion favor a tumor. Consolidation tends to have poorly defined deep margins and contains sonographic fluid- or air bronchograms within.
References: Hertzberg BS, Middleton WD. Ultrasound: the requisites, 3rd ed. Philadelphia, PA: Elsevier, 2016:254-261.
Rumack CM, Wilson SR, et al. Diagnostic ultrasound, 4th ed. Philadelphia, PA: Elsevier Mosby, 2011:603-619.
4 A 80-year-old woman with detected abdominal mass. Shown here are axial CT image of lower abdomen and transverse ultrasound image of right lower quadrant. What is the next best step in management of this patient?
|
A. The hyperechoic area around the hypoechoic lobulated mass suggests acute bleed. Mesenteric catheter angiogram should be performed on an emergent basis.
B. There is no safe approach to perform percutaneous biopsy of the mass. Laparoscopic biopsy is the only way to sample the mass.
C. The apparent “mass” seen on CT scan is unopacified small bowel and has characteristic ultrasound appearance of normal small bowel. No further evaluation is necessary.
D. Ultrasound-guided fine needle aspiration of the mass can be safely performed with needle traversing the surrounding bowel loops.
View Answer
4 Answer D. The hypoechoic mass is surrounded by small bowel loops along the anterior and lateral aspects, but this does not preclude percutaneous biopsy as trans-enteric fine needle aspiration is safe.
Choice A. The hyperechoic area around the mass represents mesenteric/omental fat and not blood. Hematoma is anechoic in the acute stages and later often evolves into a complex collection with variable hypo to anechoic components, septations, and layering debris.
Choice B. Laparoscopic biopsy is not the only option for sampling the mass. A less invasive and quick option is ultrasound or CT scan-guided trans-enteric biopsy.
Choice C. Typical ultrasound gut signature consists of outer thin hypoechoic rim representing the muscularis mucosa and muscularis propria, and an inner echogenic mucosa-lumen interface. In the image, the lesion is lobulated and heterogeneously hypoechoic throughout without the classic sonographic gut signature, suggesting a mass rather than normal bowel.
References: Carberry GA, Lubner MG, Wells SA, et al. Percutaneous biopsy in the abdomen and pelvis: a step-by-step approach. Abdom Radiol 2016;41(4):720-742.
Rumack CM, Wilson SR, et al. Diagnostic ultrasound, 4th ed. Philadelphia, PA: Elsevier Mosby, 2011:270-271.
5 A 24-year-old male presents with complaint of a 1-cm nontender palpable nodule in the right groin. Images from targeted sonography of the lesion of concern are shown. What is the most likely diagnosis?
|
A. Spermatocele
B. Incomplete descended testis
C. Indirect inguinal hernia
D. Encysted hydrocele of the cord
View Answer
5 Answer D. Ultrasound images show an anechoic oval structure along the right inguinal canal superior to and separate from the right testis and epididymis. No vascular flow is present within the cystic lesion. This represents an encysted hydrocele of the cord. Encysted hydrocele of the cord (hydrocele of the spermatic cord) is a rare anomaly that results from an aberration in the closure of the processus vaginalis. It is a loculated fluid collection along the spermatic cord, separate from the testis and the epididymis and located above them.
There are three types of spermatic cord hydroceles: communicating, funicular, and encysted.
A communicating hydrocele is associated with complete patency of the processus vaginalis. At US, it appears as a fluid collection that extends from the pelvis through the deep inguinal ring to the scrotum. A funicular hydrocele is a result of abnormal obliteration of the deep inguinal ring, with constriction just above the testis. At US, it resembles a peritoneal diverticulum, appearing as a fluid collection that communicates with the peritoneum at the deep inguinal ring and that does not surround the testicle. Funicular hydroceles become larger with increased intraperitoneal pressure during straining and smaller during relaxation. An encysted hydrocele is enclosed between two constrictions at the deep inguinal ring, just above the testis. It does not communicate with the peritoneum. An encysted hydrocele may be located anywhere along the spermatic cord. It may be any size or shape, but it does not change with increased peritoneal pressure. At US, an ovoid or a round mass is seen in the groin along the spermatic cord; internal echogenicity varies depending on the contents.
Spermatoceles (choice A) are cystic lesions that occur in the head of the epididymis and are filled with spermatozoa-containing fluid. Low-level echoes and septations can be seen in the lumen of spermatoceles. A normal descended testis is shown inferior to the encysted hydrocele. Therefore, choice B is incorrect. The images here do not show any herniation of mesenteric fat or bowel loops into the inguinal canal or scrotum. Therefore, choice C—indirect inguinal hernia is incorrect.
References: Garriga V, Serrano A, Marin A, et al. US of the tunica vaginalis testis: anatomic relationships and pathologic conditions. RadioGraphics 2009;29(7):2017-2032.
Hertzberg BS, Middleton WD. Ultrasound: the requisites, 3rd ed. Philadelphia, PA: Elsevier, 2016:147.
6 A 25-year-old female recently established care with a new primary care physician and presented for her first annual routine visit. She is sent from her primary care physician’s office for evaluation of an imaging finding seen on an outside hospital CT scan from 5 years prior. She is asymptomatic. What is the most likely diagnosis?
|
A. Pseudomyxoma peritonei
B. Abdominal abscess
C. Lymphangioma
D. Urinoma
View Answer
6 Answer C. A CT image from 5 years prior shows a low attenuation lesion occupying the periportal space, encasing multiple vessels, and conforming to the surrounding structures. Ultrasound evaluation of this lesion shows multiple thin-walled small cystic spaces. In an asymptomatic patient who has had this lesion for several years, the most likely diagnosis from the choices provided would be an abdominal lymphangioma.
Lymphangiomas are benign lesions of vascular origin that show lymphatic differentiation. They occur predominantly in the cervical and axillary regions. They are quite rare in the peritoneal cavity. In the abdomen, lymphangiomas occur most commonly in the mesentery, followed by the omentum, mesocolon, and retroperitoneum.
Histologically, lymphangiomas are thin-walled cystic masses. They may contain large macroscopic cysts or microscopic cysts. The dilated lymphatic spaces are lined with attenuated endothelial cells resembling the cells that line normal lymphatics.
The ultrasonographic appearance of lymphangioma is described as a cystic lesion with multiple thin septa (honeycomb or cobweb pattern). CT may show enhancement of the cyst wall and septae. The fluid component is typically homogeneous with low attenuation values. On MRI, the cyst contents are low in signal intensity on T1-weighted images and high in signal intensity on T2-weighted images. Magnetic resonance imaging is the most useful preoperative radiological tool for diagnosis and in surgical planning.
Choice A. Pseudomyxoma peritonei (PMP)—would not be expected to be stable over several years. The low attenuation lesion in this case has smooth borders on CT scan. There is no evidence of scalloping of the liver surface, which is commonly seen with PMP.
Choice B. Abdominal abscess—is a collection of purulent material in the abdomen. It would be accompanied by constitutional symptoms such as pain and fever.
Choice D. Urinoma—would not be expected to be seen in an otherwise healthy, asymptomatic patient. Moreover, the low attenuation lesion in this case is not in the perinephric space, which is where a urinoma would be expected to be seen.
References: Levy AD, Cantisani V, Miettinen M. Abdominal lymphangiomas: imaging features with pathologic correlation. AJR Am J Roentgenol 2004;182(6):1485-1491.
Rumack CM, Wilson SR, Charboneau WJ. Diagnostic ultrasound, 2-Volume set, 4th ed. Philadelphia, PA: Elsevier Health Sciences, 2011:529.
7 With regard to relative ultrasound power, what is the difference in ultrasound power corresponding to an increase of 3 dB?
A. Doubling
B. Half
C. 10-fold
D. 100-fold
View Answer
7 Answer A. The decibel scale is used to compare different levels of ultrasound power. The decibel value equals 10 times the log10 of the ratio of the intensities being compared. In this example, 10(log10 × 2) = 3 dB. It follows that-3 dB corresponds to halving of acoustic power. A 10-fold increase in sound intensity corresponds to 10(log10 × 10) = 10 dB. A 100-fold increase in sound intensity corresponds to 10(log10 × 100) = 20 dB.
Reference: Rumack CM, Wilson SR, Charboneau WJ. Diagnostic ultrasound, 2-Volume set, 4th ed. Philadelphia, PA: Elsevier Health Sciences, 2011:7.
8 Which of the following are components of spatial resolution in ultrasound?
A. Axial, elevational, and coronal resolution
B. Axial, coronal, and sagittal resolution
C. Axial, sagittal, and elevational resolution
D. Axial, lateral, and elevational resolution
View Answer
8 Answer D. Axial, lateral, and elevational resolution are the three components of spatial resolution in ultrasound. Axial resolution is the ability to separate two closely spaced objects in the direction of the ultrasound beam. Lateral resolution is the ability to separate two closely spaced objects perpendicular to the direction of the ultrasound beam. Elevational/slice thickness resolution is perpendicular to the image plane.
Reference: Bushberg JT, Seibert JA, Leidholdt EM. The essential physics of medical imaging, 3rd ed. Philadelphia, PA: Wolters Kluwer Health/Lippincott Williams & Wilkins, 2011:561.
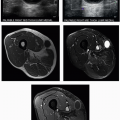
9 A 28-year-old male presents with painful bulge in right lower abdomen 3 weeks following right lower quadrant renal transplant. What is the most likely etiology of his symptoms based on the ultrasound images?
|
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree