Scrotum
QUESTIONS
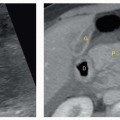
1 A 25-year-old healthy male presents with painless left testicular mass. Which of the following when present is the most helpful distinguishing feature of the lesion shown in the images here?
|
A. Well encapsulated with sharply delineated borders
B. Lack of vascular flow on color Doppler
C. Normal background testicular parenchyma
D. Alternating hypo- and hyperechogenic concentric rings
View Answer
1 Answer D. Images of the left testis show a well-circumscribed solid mass with multiple concentric hypo- and hyperechogenic rings giving it an “onion ring” appearance. There is lack of vascular flow on color Doppler, and the surrounding testicular parenchyma is normal. The findings are pathognomonic of epidermoid cyst of the testis, which is a rare but benign lesion.
Alternating hypo- and hyperechogenic concentric rings are considered to be characteristic of an epidermoid cyst and correspond to its natural evolution. The lining of the cyst produces keratin in successive layers by desquamating epithelium from the cyst wall, resulting in the onion ring appearance.
References: Hertzberg BS, Middleton WD. Ultrasound: the requisites, 3rd ed. Philadelphia, PA: Elsevier, 2016:153.
Loya AG, Said JW, Grant EG. Epidermoid cyst of the testis: radiologic-pathologic correlation. RadioGraphics 2004;24(Suppl 1):S243-S246.
Rumack CM, Wilson SR, Charboneau WJ. Diagnostic ultrasound, 4th ed. Philadelphia, PA: Elsevier Health Sciences, 2011:853-854.
2 A patient is referred for a scrotal ultrasound for acute scrotal pain. He is concerned about the potential risks of ultrasound including infertility. What is the best course of action?
A. Perform the ultrasound after telling him that sound waves cannot possibly cause harm.
B. Tell him that you understand his concerns, and return him to the emergency department.
C. Agree not to use Doppler ultrasound to image his testes.
D. Tell him that the benefits of this study far outweigh the risks, if any, that exist.
View Answer
2 Answer D. The potential for higher ultrasound intensities to cause biologic injury has been established in the laboratory. A theoretical risk exists that diagnostic ultrasound can also produce unwanted biologic effects on humans, especially on intrauterine gestations as a result of thermal and nonthermal bioeffects. However, diagnostic ultrasound has an excellent safety record, and there have been no reported incidents of adverse bioeffects on humans at diagnostic ultrasound levels in the absence of contrast agents. In situations in which an ultrasound is clinically indicated, the benefit of the ultrasound will outweigh the risks.
Reference: American Institute of Ultrasound in Medicine. Medical ultrasound safety, 3rd ed. Laurel, MD: American Institute of Ultrasound in Medicine, 2014:23-28.
3 How many gray levels are usually displayed in ultrasound images?
A. 24 (i.e., 16)
B. 26 (i.e., 64)
C. 28 (i.e., 256)
D. 210 (i.e., 1,024)
View Answer
3 Answer C. Ultrasound images are typically composed of 640 × 480 or 512 × 512 pixels. Each pixel has a depth of 8 bits (1 byte) of digital data, providing up to 28, that is, 256 levels of gray scale.
Reference: Bushberg JT, Seibert JA, Leidholdt EM. The essential physics of medical imaging, 3rd ed. Philadelphia, PA: Wolters Kluwer Health/Lippincott Williams & Wilkins, 2011:542.
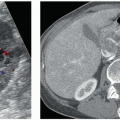
4a A 70-year-old man presents to the emergency department with diffuse scrotal pain and swelling. There is no history of trauma. Of the following choices, which underlying illness does he most likely have?
|
A. Lymphoma
B. Congestive heart failure
C. Pseudomembranous colitis
D. Diabetes mellitus
View Answer
4a Answer D. Images of the right testicle show multiple echogenic foci with “dirty” shadowing in the scrotum posterior to the right testicle consistent with gas. In the setting of scrotal swelling, pain and no history of trauma, the findings are consistent with Fournier gangrene. The most common predisposing factors for Fournier gangrene are diabetes mellitus and alcoholism. Therefore, choice D is the correct answer.
Coexisting diabetes mellitus has been found in up to 40% to 60% of patients with Fournier gangrene. Other predisposing factors include indwelling Foley catheters, surgical procedures, malignancy, steroids, chemotherapy, radiation therapy, prolonged hospitalization, and HIV. It occurs most frequently in men aged 50 to 70 years. Multiple organisms are usually involved, including Klebsiella, Streptococcus, Proteus, and Staphylococcus.
Congestive heart failure (choice B) and pseudomembranous colitis (choice C) are not risk factors. Although malignancy can be associated with Fournier gangrene, lymphoma (choice A) is incorrect because diabetes mellitus is a far more common cause.
4b Which of the following is the appropriate management for this patient?
A. Consultation with medical oncologist
B. Echocardiogram
C. Optical colonoscopy
D. Emergent surgical debridement
View Answer
4b Answer D. The treatment of Fournier gangrene includes IV antibiotics, hemodynamic stabilization, and immediate surgical debridement. Multiple debridements may be needed to remove all nonviable tissue. Patients with incomplete debridement/drainage or who are treated with antibiotics alone have a poor prognosis. The cause of death includes severe sepsis, multiple organ failure, coagulopathy, acute renal failure, and diabetic ketoacidosis.
References: Levenson R, Singh A, Novelline R. Fournier gangrene: role of imaging. RadioGraphics 2008;28(2):519-528.
Rumack CM, Wilson SR, Charboneau WJ. Diagnostic ultrasound, 4th ed. Philadelphia, PA: Elsevier Health Sciences, 2011:869.
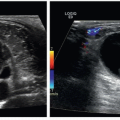
5 A 28-year-old man presents to the emergency department, and a testicular ultrasound is requested. The history provided by the ED is “right scrotal swelling.” Of the following choices, which is the most likely correct history?
A. Acute-onset scrotal pain and swelling
B. Palpable, painless testicular mass
C. Blunt scrotal trauma
D. Fever and pyuria
View Answer
5 Answer C. Images 1 and 2 show a contour abnormality of the testicle at the lower end of the image. Image 3 shows flow within the testicle, except for a peripheral hypoechoic area with no flow, and geographic, non-mass-like margins. There is disruption of the tunica albuginea, which is free floating in image 1. The findings are consistent with testicular rupture.
The tunica albuginea is a thin, echogenic curvilinear structure completely surrounding the testes. Disruption of the tunica along with extrusion of the seminiferous tubules is a specific sign of testicular rupture. The contour abnormality at the lower end of the images represents the extruded seminiferous tubules. In addition, there is a hydrocele containing low-level echoes consistent with a hematocele. Therefore, blunt scrotal trauma (choice C) is the correct answer. An intact tunica albuginea is crucial, because, if intact, surgery is usually not indicated. If disrupted, testicular viability can be maintained more than 80% of the time if surgery is performed within 72 hours. Afterward, viability drops to below 50%. A disruption of the tunica albuginea is a definitive sign of rupture, but is often not detected. A contour abnormality indicates extrusion of the seminiferous tubules and is a reliable secondary sign.
Patients with intrascrotal hematoma or hematocele will typically undergo surgical exploration because of the difficulty in excluding rupture in their presence. Testicular fracture indicates tearing of the testicular parenchyma with or without disruption of the tunica albuginea. It appears as an avascular or hypovascular intratesticular defect. Intratesticular hematoma is also common in testicular trauma. When large, they can lead to testicular necrosis, and surgical exploration is necessary.
Acute onset of testicular pain and swelling (choice A) can be seen in epididymitis-orchitis and torsion. However, the contour abnormality and disrupted tunica would not be seen in either of these entities. One would expect to see a mass with Doppler flow, and no disruption of the tunica if the patient had a neoplastic process (choice B). Fever and pyuria (choice D) would be indicative of an infectious process. Of the choices, the images support trauma, not infection.
References: Hertzberg BS, Middleton WD. Ultrasound: the requisites, 3rd ed. Philadelphia, PA: Elsevier, 2016:164-167.
Rumack CM, Wilson SR, Charboneau WJ. Diagnostic ultrasound, 4th ed. Philadelphia, PA: Elsevier Health Sciences, 2011:869-871.
6 A 48-year-old male with scrotal pain receives a scrotal ultrasound. Based on these images, what is the most appropriate next step in management?
|
A. Surgery
B. Reassurance
C. Further imaging
D. Follow-up ultrasound in 6 months
View Answer
6 Answer C. Multiple dilated veins within the right scrotum are compatible with a scrotal varicocele. Varicoceles are usually the result of incompetent or congenitally absent valves within the testicular vein. They are the most common correctable cause of male infertility. Diagnostic criteria include dilated veins of the pampiniform plexus greater in diameter than 2 to 3 mm in standing or supine positions and venous reflux on Doppler imaging during or without a Valsalva maneuver. The majority of varicoceles (85%) are unilateral and left sided. Bilateral varicoceles constitute the majority of the remainder of cases. Unilateral right-sided varicoceles rarely occur. When they do, compression of the right spermatic vein by a retroperitoneal mass or situs inversus should be considered.
Reference: Hertzberg BS, Middleton WD. Ultrasound: the requisites, 3rd ed. Philadelphia, PA: Elsevier, 2016:148-150.
7 A 53-year-old afebrile male with history of vasectomy presenting with left scrotal pain receives a scrotal ultrasound. What is the most likely diagnosis?
|
A. Sperm granuloma
B. Varicocele
C. Germ cell tumor
D. Hematocele
View Answer
7 Answer A. Sperm granulomas are presumed to be because of a necrotizing granulomatous response to extravasated spermatozoa. They can be painful or asymptomatic and are most frequently found in patients who have undergone vasectomy. Sperm granulomas are typically hypoechoic or heterogeneous and often lack increased Doppler flow. Calcifications can be seen in chronic sperm granulomas.
Varicoceles (choice B) are anechoic and tubular and contain Doppler flow. Germ cell tumors (choice C) arise from the testis and not the epididymis. The lesion shown is solid and in the region of epididymis. There is no peritesticular collection to suggest hematocele (choice D).
References: Black JA, Patel A. Sonography of the abnormal extratesticular space. AJR Am J Roentgenol 1996;167(2):507-511.
Rumack CM, Wilson SR, Charboneau WJ. Diagnostic ultrasound, 4th ed. Philadelphia, PA: Elsevier Health Sciences, 2011:872.
8a A 36-year-old man presents to the ED with acute left scrotal pain and swelling. Based on the history and imaging findings, what is the appropriate next step in the management of this patient?
|
A. The patient can be discharged with antibiotics and instructions to follow up with urology.
B. CT scan of the abdomen and pelvis for staging.
C. Discharge the patient with pain medication and instructions to follow up with urology.
D. Prompt surgical intervention.
View Answer
8a Answer D. The first image is of the right testicle, which has a normal appearance and normal color Doppler signal. The second image is of the left testicle, showing no detectable Doppler signal. The third image shows asymmetry of flow on a side-by-side view, and the fourth image labeled “left spermatic cord” shows a whirlpool appearance of the cord, the so-called torsion knot. This is a case of testicular torsion. In adults presenting with acute scrotal pain in the absence of trauma, the distinction must be made between torsion and an inflammatory condition such as acute epididymitis. Testicular torsion usually occurs as a result of a faulty attachment of the testis to the scrotal wall, most commonly resulting in the bell-clapper deformity. In this condition, the tunica vaginalis completely surrounds the testis, causing the testis to be freely suspended by the spermatic cord in the scrotal sac. Prompt surgical intervention (choice D) is necessary if the testis is to be salvaged.
The salvage rate is 80% to 100% if surgery is performed within 6 hours after the onset of pain but drops to only 20% if surgery is delayed for more than 12 hours. In most cases of torsion, as in this case, there will be no detectable flow. Some cases will show flow that is asymmetric, which is why side-by-side images are mandatory. If the torsion is prolonged, there may be hyperemia in the tissues surrounding the infarcted testis. Gray-scale findings in torsion are variable, and echogenicity may be normal, increased, or decreased, and the parenchyma may be homogeneous or heterogeneous. If the testis is hypoechoic or heterogeneous, it is likely nonviable.
Choice A is incorrect because this is not a case of epididymitis. With epididymitis or epididymitis-orchitis, one would expect to see increased flow on the side of pain, not decreased/absent flow as in this case. If this was a case of tumor infiltration of the left testis, one would expect to see increased flow in the affected parenchyma. Tumor most often presents as a painless mass, which is not how this patient presented. Therefore, a staging CT scan (choice B) is not appropriate. Choice C is incorrect because of the need for prompt surgical intervention, ideally within 6 hours, for salvage.
8b What is the salvage rate if surgery is performed after 12 hours?
A. 80% to 100%
B. Approximately 50%
C. Approximately 20%
D. 60% to 75%
View Answer
8b Answer C. Approximately 20% is the correct answer, as discussed above.
Reference: Hertzberg BS, Middleton WD. Ultrasound: the requisites, 3rd ed. Philadelphia, PA: Elsevier, 2016:159-162.
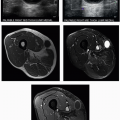
9 A 50-year-old white male who has been receiving steroid supplementation for his entire life has noticed for several years that his testes have been painless but lumpy and increasingly so in the past month. Which of the following is the most appropriate management of these findings?
|
A. Antibiotics
B. Testicular biopsy
C. Bilateral orchiectomy
D. Increased steroid dosage
View Answer




9 Answer D. The history of lifelong steroid supplementation suggests a diagnosis of congenital adrenal hyperplasia. Congenital adrenal hyperplasia (CAH) is an autosomal recessive disorder resulting in an enzyme deficiency (usually 21-hydroxylase deficiency) involved in the production of cortisol and aldosterone. Low levels of glucocorticoids and mineralocorticoids lead to elevated levels of adrenocorticotropin (ACTH), which in turn lead to adrenal hyperplasia. Adrenal rests are ectopic foci of adrenal tissue that can be found in up to 50% of normal neonates within the retroperitoneum, broad ligaments, ovaries, inguinal region, and testes. Normally, adrenal rests almost always regress. However, elevated ACTH levels in the setting of CAH can maintain and grow the ectopic rests. Testicular adrenal rests are usually bilateral and vary in size from 4 to 38 mm. They are usually sharply demarcated hypoechoic lesions on ultrasound. Large lesions are palpable. As lesions enlarge, they may compress the surrounding testicular parenchyma, leading to infertility or chronic pain.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree