Hand and Wrist
Monique Reijnierse
Nicole C. Fernandes
INTRODUCTION
The complex soft tissue structures of the hand and wrist are ideally suited for ultrasound examination. They are superficial and accessible. Dynamic examination can be performed in real-time and vascularity assessed by color or power Doppler. Standard linear array transducers are adequate for most purposes, but small footprint transducers operating at high frequency (>10MHz) may be valuable.
ANATOMY OF THE WRIST
Bones and Ligaments
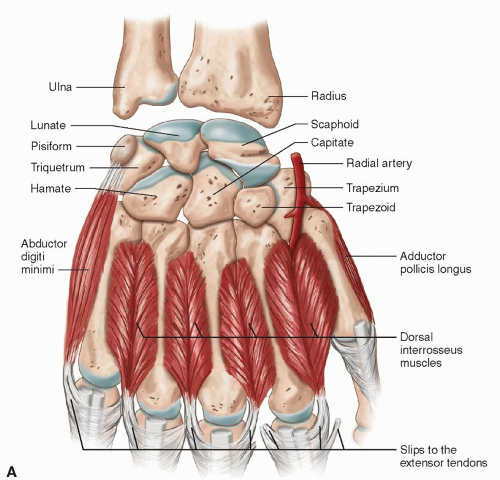
Two carpal rows with eight carpal bones form the wrist. From radial to ulnar, the proximal carpal row is formed by scaphoid, lunate, triquetrum, and pisiform, and the distal carpal row by trapezium, trapezoid, capitate, and hamate (Fig. 5.1). Stability is maintained by extrinsic (radiocarpal and ulnocarpal) and intrinsic (intercarpal) ligaments. Palmar and dorsal ligaments are differentiated and are named for the bones from which they originate and into which they insert, starting from proximal to distal and from radial to ulnar.1,2
The scapholunate (SLL) and lunotriquetral ligaments (LTL) are the most important intrinsic ligaments. They have thick palmar and dorsal components and thinner central portions.3
The triangular fibrocartilage is a biconcave disk between the ulnar styloid and the radius, with a variable thickness. Together with the meniscus homologue,
the ulnar collateral ligament (UCL), the radioulnar ligament, and the sheath of the extensor carpi ulnaris (ECU) tendon, the triangular fibrocartilage forms the triangular fibrocartilage complex (TFCC).3 It increases stability of the ulnar side of the wrist.
the ulnar collateral ligament (UCL), the radioulnar ligament, and the sheath of the extensor carpi ulnaris (ECU) tendon, the triangular fibrocartilage forms the triangular fibrocartilage complex (TFCC).3 It increases stability of the ulnar side of the wrist.
Tendons and Synovium
Extensor Tendons at the Wrist
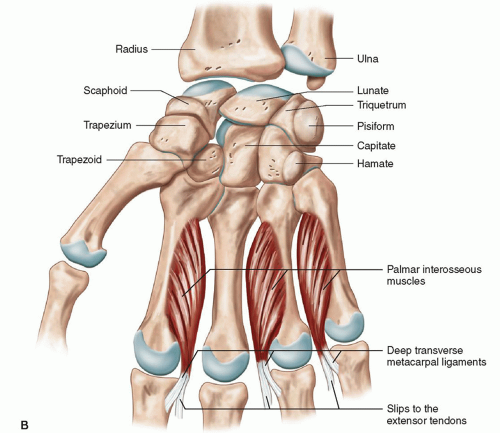
The extensor tendons run across the dorsum of the wrist held in position by the extensor retinaculum, a focal thickening of the deep fascia that is attached to the radius laterally and to the triquetrum and pisiform medially. Fibrous bands extend from the deep surface of the retinaculum and attach to the radius and ulna, resulting in six separate compartments numbered 1 to 6, starting from the radial side.
Compartment one is at the level of the styloid process of the radius and contains the tendons of abductor pollicis longus (APL) and extensor pollicis brevis (EPB).
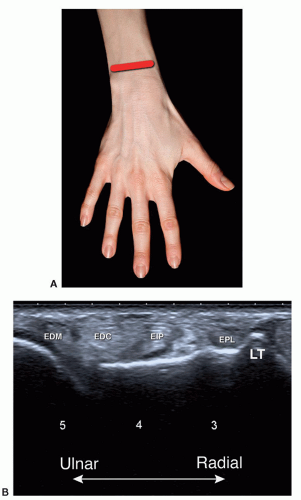
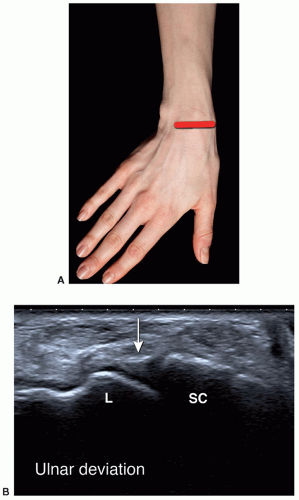
Compartment two lies on the radial side of Lister’s tubercle, a bony prominence on the dorsal aspect of the distal radius, and contains the extensor carpi radialis longus (ECRL) and extensor carpi radialis brevis (ECRB) tendons. Ulnar to Lister’s tubercle, compartment three contains the extensor pollicis longus (EPL) tendon. The fourth compartment is the last compartment on the ulnar side of the radius, and contains the four tendons of the extensor digitorum muscle and the tendon of extensor indicis, which is deeper. Compartment five lies over the ulna, at the level of the distal radioulnar joint, and contains the extensor digiti minimi (EDM) tendon. Compartment six contains the tendon of the ECU in the groove of the distal ulna (Fig. 5.2).
The tendons of each compartment are enveloped by double-layered synovial sheaths to prevent friction.4 These sheaths extend proximally and distally from the extensor retinaculum. The sheaths surrounding the tendons to the fingers are longer than those of ECU, ECRB, and ECRL. The tendons of ECRB and ECRL insert on the bases of the second and third metacarpals, and ECU inserts on the base of the fifth metacarpal. Abductor pollicis longus inserts on the base of the first metacarpal. The extensor tendons are vulnerable at the dorsum of the hand, since they are located superficially. The extensor digitorum tendons show intertendinous connections that limit separate movement. Since the tendon of the extensor indicis is extra, separate extension of the index finger is possible.
Proximal to the extensor retinaculum the tendons of compartment one cross superficial to the tendons of compartment two. Distal to Lister’s tubercle, EPL crosses over extensor compartment two.
Flexor Tendons at the Wrist
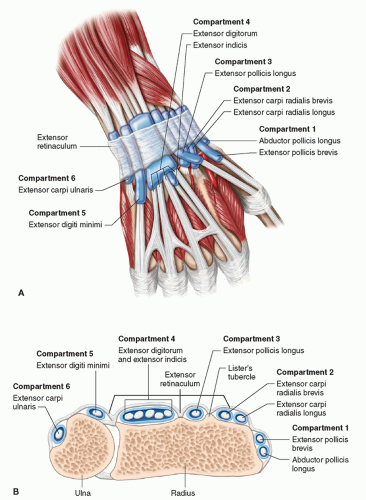
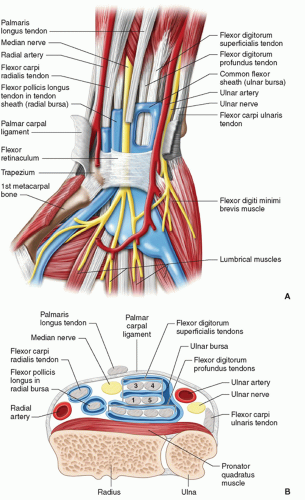
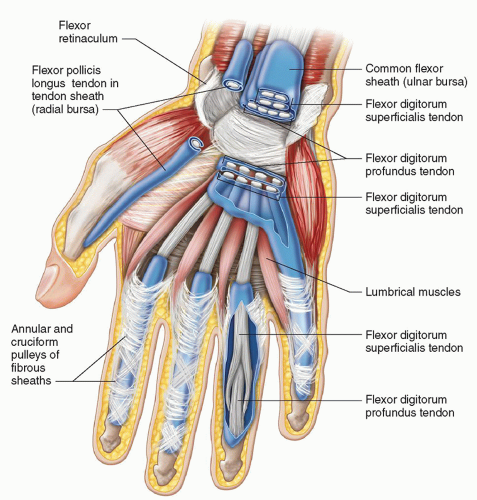
There are nine flexor tendons in the carpal tunnel. The flexor tendons of the fingers, the flexor digitorum superficialis (FDS) and flexor digitorum profundus (FDP), are arranged in the carpal tunnel, superficial and deep, respectively, and continue distally in pairs to each finger except the thumb (Fig. 5.3). They are invested by a common tendon sheath that starts proximal to the carpal tunnel and extends to within 5 mm of the insertion of the profundus tendon on the distal phalanx. A separate ulnar bursa envelops the flexor tendons of the little finger. There is a gap between ulnar bursa and the synovial sheaths of the index, long, and ring fingers in the distal palm of the hand. The other tendon in the carpal
tunnel is the flexor tendon of the thumb, flexor pollicis longus, which has a separate synovial covering, the radial bursa (Fig. 5.4).
tunnel is the flexor tendon of the thumb, flexor pollicis longus, which has a separate synovial covering, the radial bursa (Fig. 5.4).
There are two primary wrist flexors. They are superficial to the carpal tunnel. The flexor carpi radialis (FCR) tendon inserts on the base of the second metacarpal. It has a separate synovial sheath. Flexor carpi ulnaris (FCU) contains the pisiform, a sesamoid bone, and inserts on the hook of the hamate and the base of the fifth metacarpal. The FCU does not have a tendon sheath. The palmaris longus tendon is a thin, variable tendon that inserts on the transverse carpal ligament and the palmar aponeurosis and is absent in 20% of cases.4
Nerves at the Wrist
The median nerve (MN) enters the carpal tunnel with the FDP and FDS tendons of the fingers. The MN is located superficial to the flexor pollicis longus tendon and the FDS tendon of the index finger. Distal to the carpal tunnel, it divides into recurrent motor and common palmar digital nerves.5 It provides the motor supply for the muscles of the thenar eminence and the sensory supply to the palmar aspect of the thumb, index, and middle fingers and the radial half of the ring finger.3 Anatomic variants include a persistent median artery of the forearm and bifid MN.
The ulnar nerve and artery run through Guyon’s canal. The floor of this small tunnel is formed by the transverse carpal ligament, its ulnar wall by the pisiform, and its roof by the palmar carpal ligament, which is an extension of the flexor retinaculum. The tunnel is demarcated by the pisiform proximally and the hook of hamate distally. The ulnar nerve divides in the distal canal into a superficial sensory branch and a deep motor branch, located on either side of the flexor digiti minimi brevis muscle.5,6 The sensory branch supplies the palmar aspect of the ulnar portion of the ring finger and the little finger, and the motor branch supplies the muscles of the hypothenar eminence, ulnar lumbrical, and interosseous muscles and the adductor pollicis.4
The radial nerve at the wrist is a small superficial branch in the subcutis and pierces the deep fascia proximal to the extensor retinaculum. It crosses the first extensor compartment, subdivides into two branches, which usually split into four or five dorsal digital nerves, and provides sensation to the dorsum of the wrist, hand, thumb, and proximal fingers.6,4
ANATOMY OF THE FINGERS
The five metacarpal bones and their phalanges form the metacarpophalangeal (MCP) and proximal (PIP) and distal interphalangeal (DIP) joints, except for the thumb, which has a metacarpal joint and a single interphalangeal joint. In each joint, the bones are united by a loose articular capsule, radial and ulnar collateral ligaments, and a palmar ligament. Dorsally the joints are reinforced by the expansion of the digital extensor tendon.4
The collateral ligaments are strong, fan-shaped, cordlike bands that stabilize the joint.
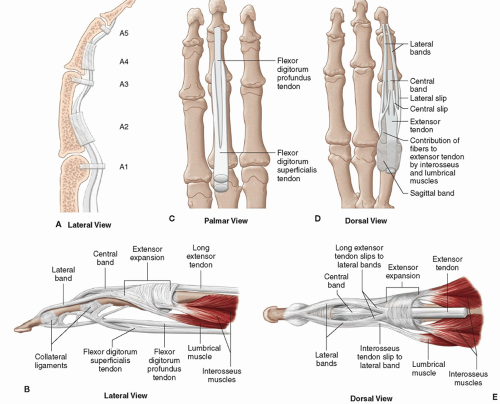
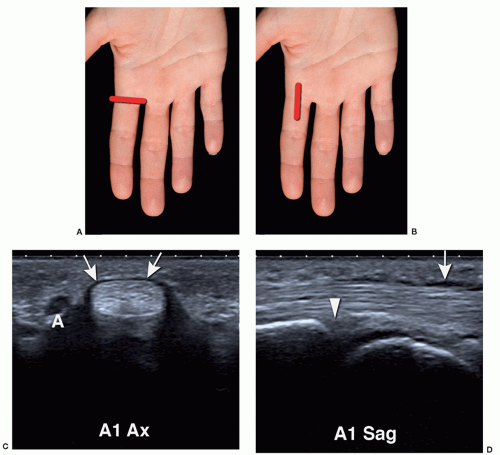
The palmar ligament, also called the palmar or volar plate, consists of thick fibrocartilage, extending from the neck of the proximal bone to the base of the distal bone. Proximally it is loosely attached, distally firmly. At the sides, it is continuous with the collateral ligaments, and at the level of the MCP joints it is also continuous with the deep transverse metacarpal ligament. On the volar side of the palmar plate, a groove holds the flexor digitorum tendons. Fibrous sheaths cover the synovial sheaths and extend from the head of the metacarpals distally. The fibrous sheaths have thick, transversely running fibers, pulleys, which insert on the palmar plate (Fig. 5.5). The pulley system refers to a number of ligaments, including annular pulleys (A1-A5) and cruciform pulleys (C1-3).
Their task is to keep the tendons close to the bone in flexion and to prevent “bowstringing.” The A2 and A4 pulleys are broader than the others and are functionally more important. (Fig. 5.5)
The tendon of FDP inserts on the base of the distal phalanx. The tendon of FDS splits at the level of the proximal phalanx and inserts on the shaft of the middle phalanx (Fig. 5.5B).
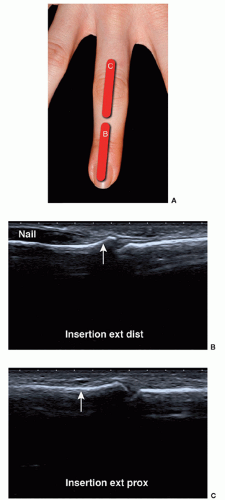
The four tendons of extensor digitorum longus flatten distally from the MCP joints and divide into three slips: the central slip inserts on the base of the middle phalanx, and the two lateral slips insert on the base of the distal phalanx (Fig. 5.5C). The extensor tendons are closely related to the joint capsule, and an extensor expansion for the MCP, PIP, and DIP joints is formed by the tendons of the lumbrical and interosseous muscles of the hand.4 At the level of the MCP joint this dorsal expansion is called a hood. A triangular aponeurosis is formed over the distal end of the middle phalanx, with the apex inserting on the distal phalanx. The thumb has two separate extensor tendons: the EPL inserting on the base of the distal phalanx and the EPB inserting on the base of the proximal phalanx. Thus the extensor tendons are attached to the bone by a complex ligamentous structure and do not have a synovial sheath.
ULTRASOUND TECHNIQUE
The patient is seated opposite the examiner, with the hand placed on the examination couch. The height of the couch is adjusted such that it is comfortable for both the patient and the examiner. Abundant ultrasound gel is required to ensure that the ultrasound probe is in good contact with the underlying skin, without the need to exert excessive pressure. The hand is placed on an absorbent pad.
In general, anatomy is identified using a standardized protocol3,5,7 and important landmarks. Be aware of normal variations.
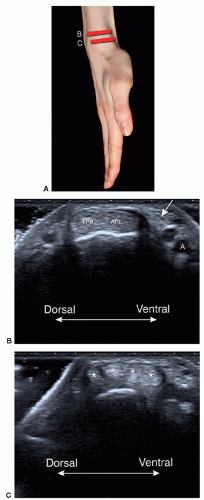
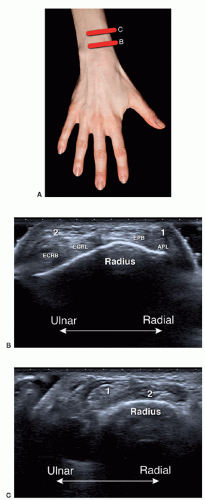
Dorsal Wrist
Start the examination of the wrist in a transverse plane. Identification of the different tendons is achieved by using the important landmark of Lister’s tubercle, a bony prominence on the distal radius that separates the second and third compartments. The six extensor compartments are identified. Compartment one contains the tendons of the APL (palmar) and the EPB (dorsal), which are best shown with the hand placed on its ulnar side, thumb upward (Fig. 5.6). A septum may divide this compartment into two. This is important in the case of therapeutic injections as the two sub-compartments may have to be injected separately.
The APL may have multiple tendinous slips, a normal finding. The radial artery and the sensory branch of the radial nerve lie palmar to the APL. The artery crosses deep to the tendons, and the nerve crosses superficial. To exclude accessory tendons at the first compartment, the APL should be followed distally over the scaphoid.
The APL may have multiple tendinous slips, a normal finding. The radial artery and the sensory branch of the radial nerve lie palmar to the APL. The artery crosses deep to the tendons, and the nerve crosses superficial. To exclude accessory tendons at the first compartment, the APL should be followed distally over the scaphoid.
The wrist is then turned prone. The second compartment (Fig. 5.7) contains ECRL and ECRB. Moving the transducer proximally from Lister’s tubercle, the point where the first compartment crosses superficial to the second compartment is identified, the site of intersection syndrome.
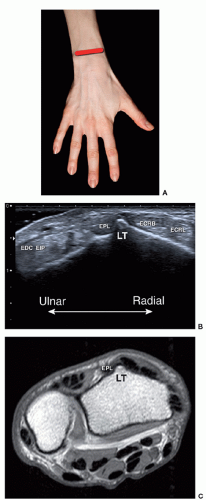
Extensor compartment three lies immediately medial or ulnar to Lister’s tubercle and contains the tendon of EPL. Distally, the tendon of EPL (Fig. 5.8) crosses superficial to the tendons of compartment two.
The fourth compartment contains the extensor digitorum communis (EDC) tendon and the tendon of the extensor indicis proprius (EIP), which is located deeper. The compartment has a thick, hypoechoic retinaculum that should not be mistaken for fluid. The fifth compartment is small and contains the tendon of EDM (Fig. 5.9).
The sixth compartment (Fig. 5.10) contains the tendon of ECU, and is best examined with the hand in extreme pronation, that is, with the thumb on the examination couch and the ulnar surface of the wrist upward.
Tip:
To remember the names of the tendons in the extensor compartments one to three, start from the radial side with longus (L) and alternate with Brevis (B): APL, EPB (1), ECRL, ECRB (2), and EPL (3).
The TFCC is located in the space between the distal ulna and the proximal carpal row, but is not well demonstrated by ultrasound. Suspected TFCC tears should be investigated by magnetic resonance imaging (MRI) or MR arthrography.
To identify the SLL (Fig. 5.11), the transducer is moved distally from Lister’s tubercle. Only the dorsal part of the SLL can be seen as a thin band running between the scaphoid and the lunate, but this is a useful screening tool in suspected SLL tears. The LTL may be seen ulnar to the SLL.
Tip:
Use Lister’s tubercle as a landmark to identify the second and third compartments. By moving distally from Lister’s tubercle, you will find the scapholunate ligament.
Longitudinal imaging is used to image the radiocarpal joint and screen for synovial hypertrophy or joint
effusion. The distal radio ulnar (DRU) joint is imaged transversely and lies just proximal to the radiocarpal joint.
effusion. The distal radio ulnar (DRU) joint is imaged transversely and lies just proximal to the radiocarpal joint.
Volar Wrist
Carpal Tunnel
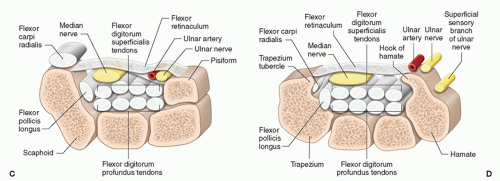
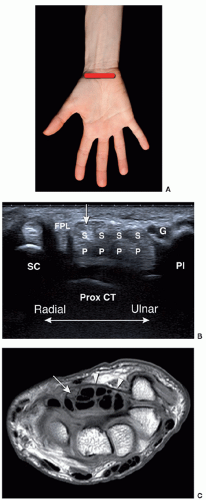
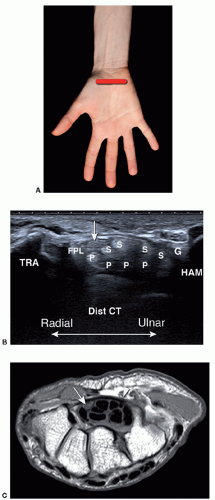
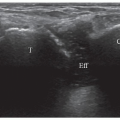
The volar wrist is examined with the wrist supinated and slightly extended. The transverse plane is most valuable in identifying the anatomic landmarks. The bony landmarks for the proximal carpal tunnel are the scaphoid tubercle (radial) and pisiform (ulnar). By placing the transducer on these marks, the flexor retinaculum, nine flexor tendons, and MN are demonstrated. (Fig. 5.12) Attention should be paid to possible anomalous muscles in the carpal tunnel. The landmarks for the distal carpal tunnel are the trapezium tubercle (radial) and hamate hook (ulnar) (Fig. 5.13). Adjustment of the orientation of the probe or slight flexion of the wrist can help to optimize imaging.
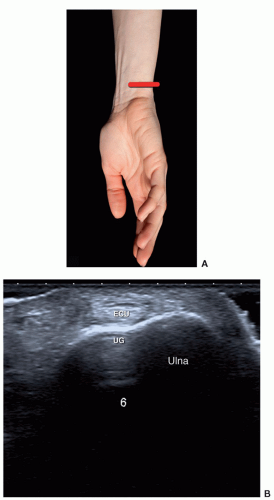 Figure 5.10. Compartment six. A: Extreme pronation of the hand is the ideal position for examining the sixth compartment. B: Extensor carpi ulnaris (ECU) is situated in the ulnar groove (UG). |
The MN is identified in the carpal tunnel in the transverse plane by rocking the transducer back and forward. As transducer angulation alters, the tendons change between hypoechoic and hyperechoic due to anisotropy, whereas the MN does not, or at least not to the same degree. On longitudinal scans, the flexor tendons show quite long excursions on finger flexion/extension, whereas the MN has a shorter excursion. Another way to identify the MN is to scan transversely in the mid-forearm and demonstrate the nerve between the muscle bellies of FDS and FDP, then trace the nerve distally to the carpal tunnel. The cross-sectional area (CSA) of the MN can be calculated proximal to and in the carpal tunnel (see section on carpal tunnel syndrome).5 As it runs distally through
the carpal tunnel, the nerve changes shape from oval to more flattened.3
the carpal tunnel, the nerve changes shape from oval to more flattened.3
Potentially important normal variants may occur here such as a persistent median artery and a bifid MN, which may coexist.
Tip:
Use anisotropy to distinguish tendons from the MN by rocking the transducer: tendons change between bright and dark; MN echogenicity does not change as much.
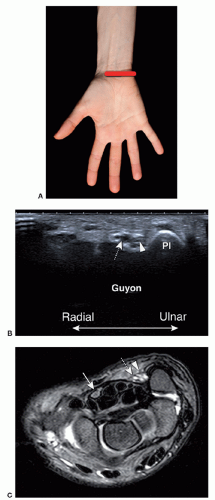
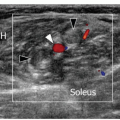
Guyon’s Canal
On the volar ulnar side of the wrist, the pisiform is the landmark for Guyon’s canal (Fig. 5.14). The ulnar nerve lies between the pisiform and the ulnar artery. Color Doppler demonstrates the ulnar artery and its companion paired veins, which are effaced by pressure and refill when pressure is removed. Moving the transducer distally identifies the division of the ulnar nerve into a superficial sensory branch and a deep motor branch. The hook of hamate is a landmark for the deep motor branch.
Fingers
Abundant gel is essential and allows good contact and visualization. Start the examination in a sagittal plane to get a first impression of the anatomy. Joint fluid is more easily detected dorsally, as the thick volar plate and capsule form a tighter structure, than the dorsal capsule. The synovial pouch, which extends distally and proximally from the joint, can be filled with fluid. Synovial thickening is less hypoechoic than fluid. Color/power Doppler differentiates between active and chronic synovitis. Appreciate the lateral pouches and collateral ligaments in the axial and coronal planes.
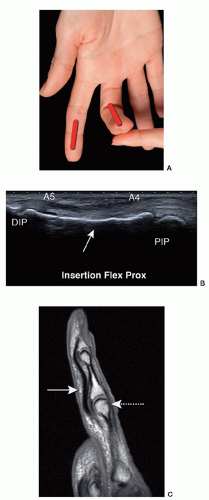
Examination of the flexor tendons starts axially in the palm of the hand, where the superficial and deep tendons are separately identified. Differentiation may be more difficult distally, but tilting the transducer back and forward at the level of the proximal phalanx and PIP joint shows anisotropy affecting the tendons inversely, that is, when FDP is hypoechoic, FDS is echogenic, and vice versa. The two slips of the superficialis tendon insert on the volar aspect and sides of the base of the middle phalanx, separated by the profundus tendon, which inserts distally on the base of the distal phalanx (Fig. 5.15). The distal FDP tendon and its insertion are best examined on longitudinal scans.
Dynamic imaging helps distinguish between superficialis and profundus tears. The transducer is placed sagittally at the level of the metacarpal joint, and passive movement of the PIP or DIP joints shows the tendons moving in the sheath.
The extensor tendons are smaller and more band-like than the flexor tendons and more difficult to examine.
A small cushion underneath the carpus allows movement and facilitates discrimination between a proximal or distal tendon tear (Fig. 5.16).
A small cushion underneath the carpus allows movement and facilitates discrimination between a proximal or distal tendon tear (Fig. 5.16).
The synovial sheath of a flexor tendon is normally not visible, although a thin hypoechoic rim <0.1 mm may surround the flexor digitorum tendons just proximal to the A1 and A2 pulleys3 and has to be differentiated from tenosynovitis.
The five annular pulleys are small hypoechoic linear structures at the level of the MCP (A1), PIP (A3), and DIP (A5) joints and the proximal shaft of the proximal (A2) and mid-shaft of the middle (A4) phalanges (Fig. 5.17). Dynamic imaging shows a pulley tear as an increased distance between the tendon and the bone (bowstringing). The C-pulleys are more difficult to visualize with ultrasound.
The palmar digital nerve branches of the median and ulnar nerves are detected by locating the palmar digital arteries with Doppler. The nerves run alongside the arteries.
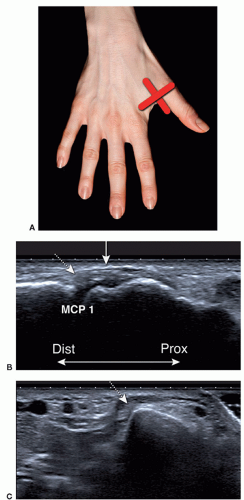
Ultrasound of the UCL of the thumb is performed with the hand prone. The transducer is placed lengthwise on the ulnar side of the MCP joint for long-axis scans, and rotated 90 degrees for short-axis images. Imaging is performed at rest. Additional imaging during flexion and cautious valgus stress can be performed. However, varus and valgus stressing should be employed with caution for fear of aggravating an injury. The normal UCL is hyperechoic and lamellar and extends from the metacarpal head to the base of the proximal phalanx. The deep fibers demonstrate anisotropy and may be hypoechoic. The adductor aponeurosis, a thin hyperechoic band superficial to the UCL, is demonstrated by flexing the interphalangeal joint while scanning in the long axis (Fig. 5.18).
Tips:
Use abundant gel, an “ice cream cone,” to maintain contact and avoid excessive pressure. Hypervascularity can be missed using too much pressure.
Use dynamic imaging by flexing and extending the finger to identify a tendon.
If there is fluid in a joint or around a tendon, always use color or power Doppler to identify hypervascularization.
Accessory Muscles
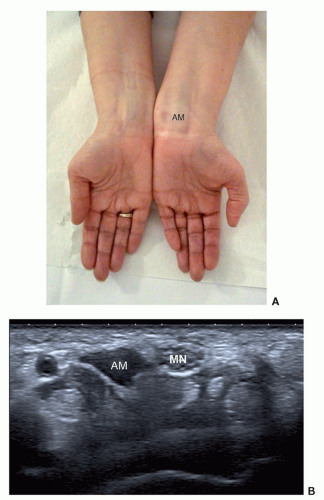
Accessory muscles are frequent incidental findings at the wrist. They have typical locations and are frequently bilateral. Most are asymptomatic, but they may present as soft tissue masses or cause nerve compression in the carpal tunnel or Guyon’s canal. Ultrasound shows a mass with similar morphology and echogenicity to other muscles, and dynamic imaging shows muscle contraction, confirming the diagnosis (Fig. 5.19). The most common
anomalous muscles include the accessory abductor digiti minimi (AADM), extensor digitorum brevis manus (EDBM), the digastric FDS of the index finger, a proximal origin of the lumbrical muscles and variants of palmaris longus.8
anomalous muscles include the accessory abductor digiti minimi (AADM), extensor digitorum brevis manus (EDBM), the digastric FDS of the index finger, a proximal origin of the lumbrical muscles and variants of palmaris longus.8
The AADM occurs in 24% to 47% of the normal population and is bilateral in 50% of cases.9,10 Sites of origin include the palmar carpal ligament, the palmaris longus tendon, and the antebrachial fascia of the forearm. The tendon of AADM inserts with the abductor digiti minimi on the ulnar aspect of the proximal phalanx of the little finger. The pisiform can be used as a landmark in identifying this accessory muscle.8 Most AADMs are small and asymptomatic, with a mean muscle thickness of 1.7 mm. The size of the accessory muscle (mean thickness 4 mm in symptomatic cases) is an important factor in determining if nerve compression at Guyon’s canal is significant.9
The EDBM muscle occurs in 3% of individuals and is bilateral in 54% of cases. It lies on the dorsum of
the wrist on the ulnar side of the extensor tendon of the index finger. It originates from the distal radius and posterior radiocarpal ligament and inserts on the index finger, at the level of the metacarpal head, less frequently the long finger.11,12 It is considered to be a variant of the EIP muscle, and the two are often joined and have the same nerve and arterial supplies and insertion. However, in 40% of individuals with an EDBM muscle, the EIP is absent or hypoplastic.13,8
the wrist on the ulnar side of the extensor tendon of the index finger. It originates from the distal radius and posterior radiocarpal ligament and inserts on the index finger, at the level of the metacarpal head, less frequently the long finger.11,12 It is considered to be a variant of the EIP muscle, and the two are often joined and have the same nerve and arterial supplies and insertion. However, in 40% of individuals with an EDBM muscle, the EIP is absent or hypoplastic.13,8
The anomalous belly of the FDS muscle in the palm of the hand is usually related to the index finger. The anomalous muscle can be seen in the carpal tunnel and can cause carpal tunnel syndrome (CTS) or it can be appreciated as a mass at the base of the index finger.14,15 The muscle can be seen moving distally in or into the carpal tunnel on finger extension and proximally when the fingers are flexed. Comparison with the opposite side may be helpful.
A proximal origin of the lumbrical muscles inside the carpal tunnel is seen in 22% of individuals and may cause CTS. Normally, the lumbricals arise from the FDP muscle and insert on the radial aspect of the extensor expansion at the level of the proximal phalanx.8,16 As with the anomalous FDS, dynamic imaging may be helpful.
Palmaris longus tendon anomalies include variants of its insertion deep to the retinaculum and a distal belly. Both can cause compression of the MN in the carpal tunnel. An accessory palmaris longus can compress the ulnar nerve during repeated contractions.17 A hypertrophied palmaris longus muscle has also been reported.18
TENDONS