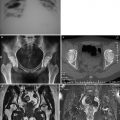
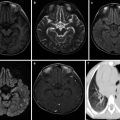
Fig. 7.1
Lesion of cerebral infarction, with degenerative and necrotic neuron as well as poorly defined or absent neuronal nissl body, H&E ×100
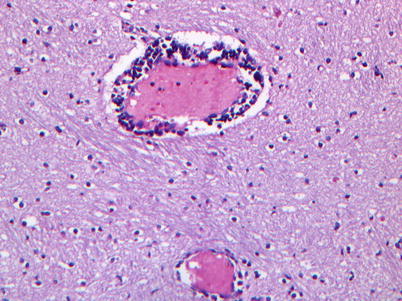
Fig. 7.2
Perivascular lymphocytic sleeve in the brain tissue, H&E ×200
2.
Lungs
Different from lung lesions of other infectious diseases such as human-infected highly pathogenic avian influenza, EV71 is most likely to damage the ventral, dorsal, and intermediate sections of the medulla oblongata. Nerve centers related to respiration and vasomotion are located at these parts. Therefore, in addition to direct invasion of virus to lung tissue, neurogenic pulmonary edema is the main reason for acute pulmonary edema. The occurrence of acute pulmonary edema is related to the impaired respiratory center at the brain stem caused by brain lesions and increased intracranial pressure caused by encephaledema. The respiratory disease in patients with EV71-induced HFMD is mainly severe viral pneumonia. Its main pathological changes include dilated and congestive vascular capillaries in the alveolar septum, a large quantity of infiltrated mononuclear cells, a large quantity of fluid from edematous lungs in the alveolar space, monocyte effusion, and formation of pulmonary hyaline membrane. These pathological changes cause pulmonary edema, local lung consolidation, and hemorrhagic infarction, constituting the main reason for respiratory distress in pediatric patients (Figs. 7.3 and 7.4).
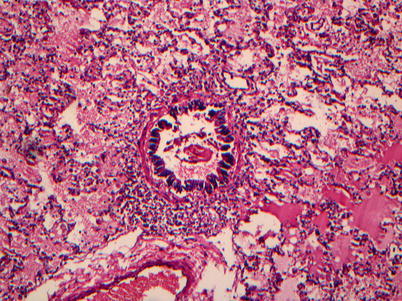
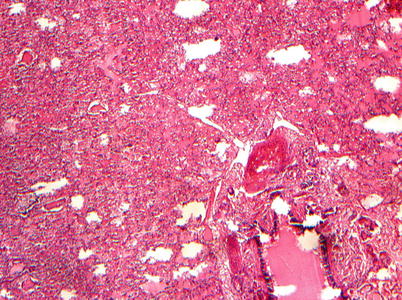
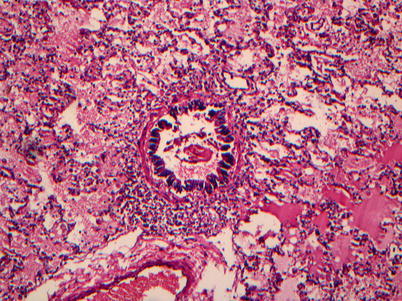
Fig. 7.3
Edema fluid in alveolar cavity and infiltration of peribronchiolar inflammatory cells, H&E ×200
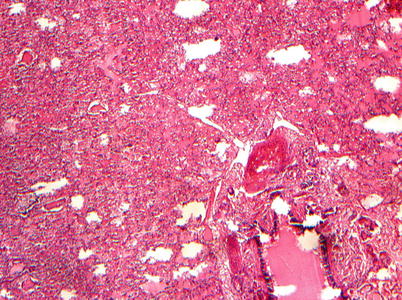
Fig. 7.4
Hemorrhage of alveolar cavity and pulmonary septum, H&E ×100
3.
Heart
EV71-induced brain stem encephalitis may cause dysfunctional autonomic nervous system. The sympathetic nerves innervating the heart, by releasing adrenaline, activate β-adrenergic receptors and then stimulate adenosine cyclase to produce cAMP. The production of cAMP leads to stronger myocardial contraction, tachycardia, and high blood pressure. Based on autopsy of death cases, it has been confirmed that the heart is slightly involved, with mild hypertrophy. The epicardium was demonstrated with patchy lymphocytic infiltration, and the myocardium was always shown with no inflammation. Occasionally, focal myocardial cells were demonstrated with degeneration and necrosis, with interstitial edema as well as infiltration of lymphocytes and plasmocytes.
In addition, other organs also show different degrees of pathological changes. For instances, hepatic sinusoid dilation, congestion, and hepatocyte edema were shown in tissues of hepatic lobule. The kidneys may be demonstrated with renal interstitial congestion, epithelial cell edema, and adrenal medulla congestion. The small intestinal mucosa is congestive and thinner, with accompanying multifocal epithelial cell necrosis, shedding of cell membrane and hyperplasia of submucosal lymphoid tissue, expanded germinal center, splenic sinus congestion, and reactive hyperplasia.
7.5 Clinical Typing and Laboratory Test
7.5.1 Incubation Period
The incubation period of EV71 infection generally lasts for 2–7 days and occasionally lasts for up to 12 days. The patients in incubation period are asymptomatic, with EV71 detectable in throat swabs or stool specimen. Most patients do not experience onset of symptoms immediately after infection, namely, latent infection or asymptomatic infection. Pediatric patients, especially infants and young children, have a high incidence rate after being infected, with various symptoms. In both symptomatic and asymptomatic patients, respiratory excretion of virus persists for 1–3 weeks, and fecal excretion of the virus persists for 7–11 weeks.
7.5.2 Clinical Typing
Based on severity and prognosis, EV71 infection can be clinically classified into four types: common type, severe type, critical type, and atypical type.
7.5.2.1 Common Type
The onset is acute onset, with mild fever and a body temperature of about 38 °C. Simultaneously or within 1–2 days after the onset, scattered ulcerative herpes occur at the mucosa of oral cavity; maculopapules and herpes occur at the skin of hands, feet, and buttocks. Red inflammatory halo surrounds the skin rashes. And the prognosis is good.
7.5.2.2 Severe Type
The severe type refers to patients with mild encephalitis, encephalomyelitis, aseptic meningitis, or acute flaccid paralysis. The patients experience neurological symptoms of low spiritual stage, drowsiness, headache, vomiting, tendency to be frightened, shaking limbs, or paralysis. By physical examination, the patients show meningeal irritation sign and weakened or absent tendon reflex. Most of the patients have no sequelae, with good prognosis.
7.5.2.3 Critical Type
Critically ill patients, especially those aged under 3 years, may experience neurogenic pulmonary edema, pulmonary hemorrhage, circulatory failure (shock) brain stem encephalitis, cerebral edema and herniation, respiratory failure, severe pneumonia, sepsis, and multiple organ failure. Most of the patients sustain relevant sequelae and the mortality rate is high.
7.5.2.4 Atypical Type
In rare patients, the patients experience no typical rashes or oral herpes and/or ulceration but only fever and some other atypical symptoms. The atypical type of patients may only experience meningitis and encephalitis but no skin rashes.
7.5.3 Laboratory Test
7.5.3.1 Peripheral WBC Count
For common type of patients, the WBC count is generally within normal range. For severe type of patients, the WBC count may significantly increase.
7.5.3.2 Blood Biochemistry
In some cases, slight increases of ALT, AST, and CK-MB may be demonstrated. In severe type of patients, blood glucose level may be increased.
7.5.3.3 Cerebrospinal Fluid Examination
For the patients with the nervous system involved, cerebrospinal fluid examination demonstrates clear fluid, increased pressure, increased WBC count (with more multinucleated cells than monocytes in the critical type of cases), normal or slightly increased protein, and normal levels of sugar and chloride.
7.5.3.4 Etiological Examination
Virus isolation is the basis to define the diagnosis:
1.
Throat swab
At the beginning of enterovirus infection, within about 1–2 weeks, the virus may be isolated from pharyngeal secretions.
2.
Fecal examination
At the early stage after enterovirus infection, the virus can be excreted in feces for 3–8 weeks or longer. Therefore, the virus can be isolated in the feces.
3.
Other examination for virus isolation
The virus can also be isolated from cerebrospinal fluid, blood, or other potentially infected tissues.
Viral nucleic acid detection can be performed by using RT-PCR. Positive finding of EV71 nucleic acid constitutes the basis to define the diagnosis.
7.5.3.5 Serological Test
Comparing to viral antibody titers in the acute and convalescent stages, an at least four times increase or IgM antibody positive is the basis to define the diagnosis.
7.6 Clinical Diagnosis
EV71 infection commonly occurs in preschoolers; especially young children aged under 3 years have been demonstrated with the highest incidence rate. The source of infection includes symptomatic patients and individuals with latent infection. The virus spreads mainly via digestive tract, respiratory tract, and close contact to secretions. The patients commonly experience maculopapules and herpes on hands, feet, oral cavity, and other body parts. Occasionally, the patients may experience encephalitis, encephalomyelitis, meningitis, pulmonary edema, and circulatory failure. Based on epidemiological data and clinical manifestations, the clinical diagnosis can be made.
7.6.1 Basis for Diagnosis
7.6.1.1 Epidemiological Data
The disease occurs during epidemic seasons and the patients are commonly aged under 3 years.
7.6.1.2 Clinical Manifestations
The patients mainly experience symptoms of fever, maculopapules, and herpes on hands, feet, oral cavity, and buttocks. Some patients may also experience symptoms of upper respiratory tract infection.
7.6.1.3 Physical Signs
Some patients only experience rashes/herpes on hands, feet, and buttocks and herpetic angina.
7.6.1.4 Nervous System Involvement as well as Respiratory and Circulatory Failure
The severe type of patients may experience neurological symptoms due to involvement of the nervous system, as well as respiratory and circulatory failure. In some rare cases, especially those aged under 3 years, the patients may experience encephalitis, encephalomyelitis, meningitis, pulmonary edema, circulatory failure, and other symptoms.
7.6.1.5 Laboratory Test
1.
Peripheral WBC count
In common type of patients, the WBC count is within normal range. In severe type of patients, the WBC count may obviously increase.
2.
Blood biochemistry
In some cases, slight increases of ALT, AST, and CK-MB can be detected. In severe cases, the blood glucose level may be increased.
3.
Cerebrospinal fluid examination
In the patients with the nervous system involved, cerebrospinal fluid is shown to be clear, with increased pressure, increased WBC count (with more multinucleated cells than monocytes in critical cases), normal or slightly increased protein, as well as normal levels of sugar and chloride.
7.6.1.6 Etiological Examination
1.
Virus isolation
The virus isolation is the basis for definitive diagnosis. Throat swab, stool specimen, cerebrospinal fluid, blood, or other potentially infected tissues can be sampled for virus isolation.
2.
Viral nucleic acid detection
EV71 nucleic acid positive by RT-PCR is also the basis for definitive diagnosis.
7.6.1.7 Serological Test
Comparing the serum viral antibody titers in the acute stage and the convalescent stage, an at least four times increase of antibody titer or IgM antibody positive also constitutes basis for the diagnosis.
7.6.1.8 Diagnostic Imaging
1.
Chest CT
Chest CT may demonstrate changes of bronchitis, pneumonia, pulmonary edema, and pulmonary hemorrhage.
2.
MRI
By MRI, the lesions are mainly located in the brain stem and the gray matter of the spinal cord.
7.6.2 Basis for Definitive Diagnosis
The diagnosis should be based on comprehensive analysis of epidemiological data, clinical manifestations, and laboratory findings. And the diagnosis can be defined based on evidence from serological test and etiological examination.
1.
After the onset, EV71 nucleic acid is detected positive or EV71 virus is isolated from stool specimen or mouth-rinsed fluid.
2.
EV71 nucleic acid is detected positive or EV71 virus is isolated from cerebrospinal fluid or herpetic fluid.
3.
EV71 IgM antibody is serologically detected in the early stage.
4.
Serum neutralizing antibody in the convalescent stage shows an at least four times increase as high as that in the acute stage.
Clinically typical cases, with any one of the above four conditions, can be defined with HFMD.
7.7 Radiological Demonstrations
7.7.1 Radiology of the Neurological Complications
Compared to CT scan, MRI is definitively superior in examining the central nervous system due to its favorable soft tissue contrast and multiparameter imaging. Therefore, MRI is the radiological modality of choice to detect and assess the neurological complications of HFMD.
7.7.1.1 Aseptic Meningitis
Aseptic meningitis, also known as viral meningitis, is a common complication occurring at the central nervous system induced by EV71. Its diagnosis is mainly based on clinical symptoms, biochemistry of cerebrospinal fluid, and virus isolation. Plain MR imaging always shows no abnormalities, and contrast MR imaging demonstrates no meningeal enhancement, indicating its difference from bacterial meningitis. In the case with HFMD complicated by viral encephalitis, necrosis and edema can be displayed at the bilateral temporal lobes and frontal lobes, with long T1 and long T2 signal from the diseased lobes. The ependyma of lateral ventricle is demonstrated thickened, with slightly hyperintense T2WI signal. And some indirect signs, including meningeal enhancement and subdural effusion, can also be shown.
7.7.1.2 Brain Stem Encephalitis
The complications of brain stem encephalitis are commonly induced by EV71 infection, with diversified radiological demonstrations.
Location of Lesion
The main lesion is located at the dorsal interface between pons and medulla oblongata, which are longitudinal lesions. The lesion may extend upward and downward to involve medulla oblongata, midbrain, thalamus, cerebellar dentate nucleus, and even into the cervical spinal cord. MRI shows abnormal patchy signals.
Signal Change
The main lesion (at the dorsal interface between pons and medulla oblongata) is demonstrated with long T1 and long T2 signals. We analyzed the cases of brain stem encephalitis by large sampling and found that the signal changes are diversified, which is related to the duration of the illness course.
Get Clinical Tree app for offline access

1.
Signal of the main lesion at the acute stage can be classified into three types based on plain and contrast imaging: (1) negative by plain MR imaging but slight enhancement by contrast imaging (Fig. 7.5); (2) positive by plain MR imaging but no enhancement by contrast imaging (Fig. 7.6) (3) as well as isointense or slightly hypointense T1WI signal, slightly hyperintense T2WI signal, hyperintense FLAIR, and DWI signals by plain imaging but no enhancement by contrast imaging; and (4) positive by plain MR imaging and slight to moderate enhancement by contrast imaging (Fig. 7.7) as well as isointense or slightly hypointense T1WI signal, slightly hyperintense T2WI signal, hyperintense FLAIR, and DWI signals by plain imaging.