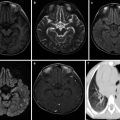
Fig. 2.1
Alveolar cavities were full of homogenous acidophilic effusions which condensed to form hyaline membranes (indicated by arrow) and attach to alveolar walls HE ×200
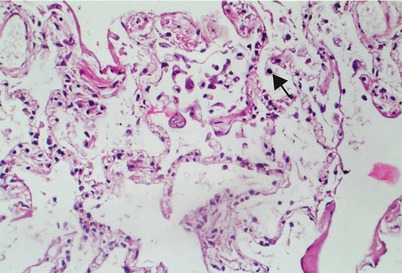
Fig. 2.2
Alveolar wall epithelial cells were disclosed with degeneration and necrosis, alveolar cavity with exfoliated type II alveolar epithelial cells (indicated by the arrow), and alveolar space with infiltration of a few lymphocytes and monocytes. HE ×200
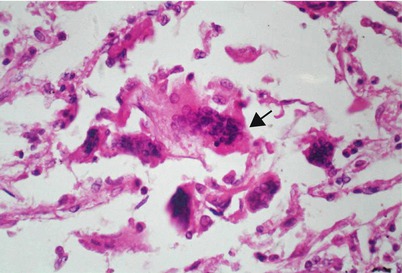
Fig. 2.3
Alveolar cavities were seen with multinucleated giant cells (indicated by the arrow). HE ×400
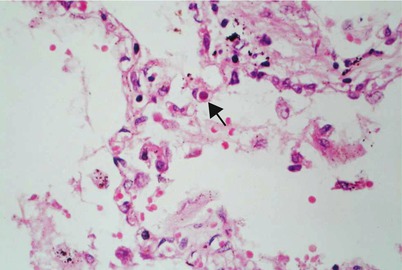
Fig. 2.4
Alveolar epithelial cells were detected with structures similar to viral inclusion bodies (indicated by the arrow), with spherical shape and acidophilic staining as well as transparent halo at the periphery. HE ×400
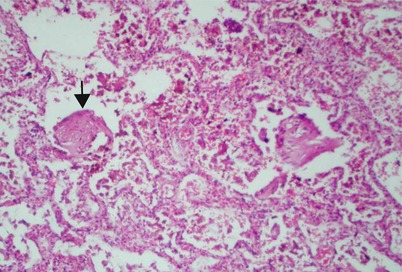
Fig. 2.5
Imaging visualized organization of fibrinous exudates from alveoli and proliferation of fibroblast to form similar glomerular structures (indicated by the arrow) HE ×200
2.4.2.2 Immune Organs
Chest and Abdominal Lymph Nodes
Pulmonary hilar lymph nodes demonstrate light swelling and present different degrees of congestion, hemorrhagic necrosis, and decrease of innate lymphocytes under the microscope. Blood sinus in the lymph nodes presents with grave congestion and dilatation, lymphoid nodule atrophy or disappearance, prominently the cortex, and lymphatic tissue focal necrosis, accompanied by apoptosis of some lymphocytes (Fig. 2.6).
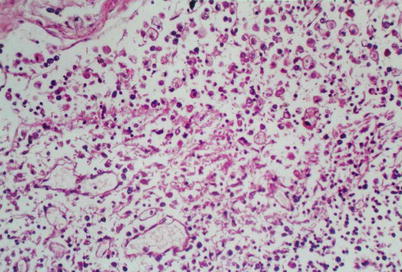
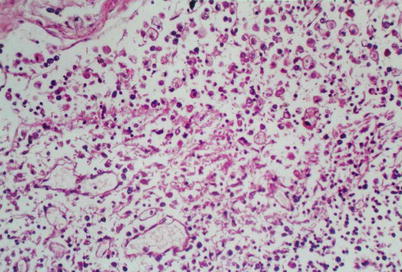
Fig. 2.6
Pulmonary hilar lymph nodes were seen with congestive necrosis and decrease of the innate lymphocytes and lymphoid nodules with atrophy and disappearance. HE ×400
Spleen
The spleen mostly shrinks with soft texture, and has patchy and focal hemorrhage at the surface and sections. Splenic white pulp is detected obviously atrophic or absent, with central arterial wall thickened, endothelial cells swollen and partially shed, peripheral lymphatic sheath lymphocyte depleted greatly, and germinal center disappeared. Splenic corpuscle is observed with plasma protein sedimentation in central arterial walls, white pulp and marginal sinus lymph tissues with large patchy necrosis, and partial remaining lymphocytes with apoptosis. The splenic sinus inside red pulp is revealed with obvious congestion and focal hemorrhagic necrosis as well as proliferation of histiocytes (Fig. 2.7).
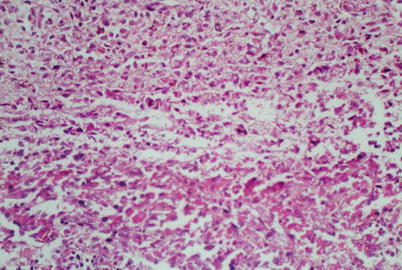
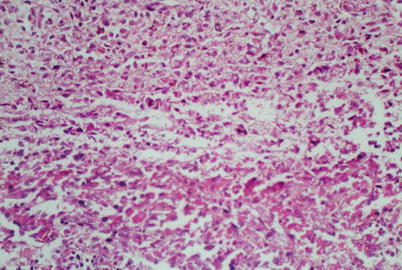
Fig. 2.7
The spleen was visualized with focal hemorrhagic necrosis and red pulp with sparse lymphocytes. HE ×200
Bone Marrow
The number of hematopoietic cells in bone marrow declines, and granulocyte system and megakaryocytic system are relatively inhibited. Polychromatic erythroblasts present with small focal proliferation.
2.4.2.3 Other Main Organs
Tissues of the brain, liver, kidney, and heart demonstrate varying degrees of congestion, edema, degeneration, and necrosis as well as infiltration of a few lymphocytes.
2.4.2.4 Secondary Infection
Secondary bacterial pneumonia and fungal infection may occur (Fig. 2.8).
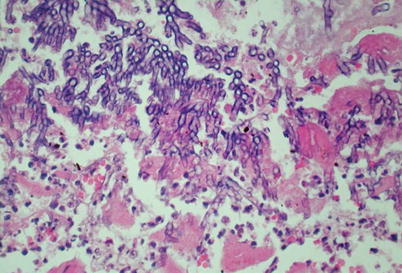
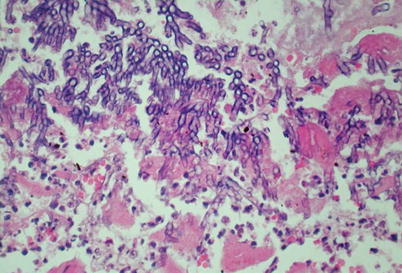
Fig. 2.8
SARS patient developed secondary pulmonary mycotic infection with dendritic hyphae. HE ×400 (Le Xiaohua Lu Jian Lang Zhenhua)
2.5 Clinical Manifestations
The initial symptom of SARS is frequently fever, accompanied by headache and general muscular and joint souring soreness, and often without nasal discharge, sore throat, and other upper respiratory tract catarrhal symptoms. Pulmonary signs are not obvious and signs and distinct systematic symptoms are inconsistent, which is typical to SARS. The clinical manifestations of SARS may vary, which can be divided into light type, common type, severe type, and atypical type, with the common type most commonly seen. Based on the clinical development, it could be divided into early phase, progression phase, and recovery phase.
2.5.1 Incubation Phase
Generally, the incubation phase lasts 2–14 days, with an average of 4–7 days and a median of 6 days, predominantly 2–10 days.
2.5.2 Symptoms
2.5.2.1 Fever
The initial symptom primarily is fever, mostly high fever, accounting for 94.4–100 %. Patient body temperature may reach 38–40 °C and 42 °C at the highest. The fever type varies, including remittent fever, irregular fever and continuous fever. The duration of fever is mostly 5–9 days.
2.5.2.2 Pain
It presents as headache, joint or/and systematic soreness, and chest pain. It is reported that the incidence of headache in SARS patients is 17–90 %.
2.5.2.3 Symptoms of T Respiratory System
Most SARS patients have cough, which is dry with scanty sputum. Generally SARS does not incur upper respiratory tract catarrhal symptoms. Severe cases may suffer from accelerated respiration, shortness of breath, or even acute respiratory distress syndrome, characterized by progressive dyspnea or even distress with respiratory frequency up to >20 times.
2.5.2.4 Palpitation and Chest Distress
Patients complain of heart beat or palpitation accompanied often by precordial discomfort. The incidence is 35–90 %.
2.5.2.5 Digestive System Symptoms
The incidence of diarrhea is reported mostly at 7–44 %, with single case up to 70 %.
2.5.3 Signs
One characteristic of SARS is severe symptoms and light signs. The signs are mostly not obvious or even absent.
2.5.3.1 Dyspnea
Dyspnea presents irregular respiratory frequency, depth, and rhythm. The incidence of dyspnea of SARS patients is 21–57 %. Severe patients may manifest nose fanning, orthopnea, and cyanosis, involvement of accessory respiratory muscles in respiration, as well as “three depression signs” upon inhalation.
2.5.3.2 Tachycardia
According to report, 11 % of typical patients and 14 % of severe patients have sinus tachycardia, and 2.3 % of SARS patients suffer from paroxysmal supraventricular tachycardia.
2.5.3.3 Pulmonary Signs
The pulmonary signs of SARS patients are frequently unobvious or absent in the early phase. Light moist rales may be audible (17–62 %). Patients may also demonstrate pulmonary consolidation sign and attenuated breath sounds. There may also be a few pleural effusions.
2.5.4 Classification
In light of conditions, it could be classified in clinics into light type, common (typical) type, severe type, and special (atypical) type.
2.5.5 Complications
2.5.5.1 Pulmonary Fibrosis
The follow-up visit of 267 SARS patients via X-ray and HRCT by Choi et al. found that about 3–4 % patients developed fibrotic changes of lung interstitium and shrinkage of lung volume.
2.5.5.2 Ischemic Necrosis of the Femoral Head
Application of glucocorticoids could to some extent alleviate lung injury of patients with severe infectious atypical pneumonia. However, long-term and abundant use of glucocorticoids may generate numerous side effects, and it is an undisputable fact that hormones may induce femoral head ischemic necrosis. Literature reports suggest that the incidence of femoral head ischemic necrosis is 5–25 %.
2.6 Laboratory Examinations
2.6.1 Blood Routine Examination
The white blood cell count remains within normal range in majority patients and may decrease in some patients (24.2 %). 95 % of severe patients without secondary infections are revealed with decreased total white blood cell, and normal neutrocyte and monocyte differential white blood cell count. However, 80 % initially diagnosed patients manifest a decrease of absolute lymphocyte count, suggestive of a tendency of gradual decline, and morphocytology change, with abnormal lymphocytes observable. 13.2–41 % patients are examined with thrombocytopenia. Many evidences prove that SARS-CoV could directly invade the immune system and act mainly on lymphocytic system, especially the T lymphocytes, which could lower peripheral blood lymphocytes. The peripheral blood white cell count is normal or decreased in most SARS patients, but CD3+, CD4+, and CD8+ T lymphocyte counts are distinctly lower compared with those of healthy population. The more severe the condition, the more drastically declined the T lymphocyte count.
2.6.2 Blood Gas Analysis
Blood gas analysis reveals hypoxemia of different degrees and commonly no carbon dioxide retention. Generally under 3–5 L/min oxygen uptake, patients with severe hypoxemia are measured of arterial partial pressure from oxygen (PaO2) <70 mmHg or blood oxygen saturation (SpO2) <93 %, or develop acute lung injury (ALI) or acute respiratory distress syndrome (ARDS).
2.6.3 Measurement of Peripheral Blood T Lymphocyte Subgroup
One of the main immunopathogenesis changes in SARS patients is insufficiency of T-lymphocyte-mediated specific cellular immunity, characterized by distinct damages of T lymphocytes and its subgroups, particularly CD3+, CD4+, and CD8+. There exists distinct correlation between the extent of T lymphocyte damages and severity of the disease.
2.6.4 Test of SARS-Specific Antibodies
The method recommended by WHO for test of serum SARS-CoV antibodies is enzyme-linked immunosorbent assay (ELISA). Upon test of the SARS-CoV-specific antibodies in the infected patients, including IgG, IgM, or total antibody, seroconversion or increase by 4 times and above of any serum antibody in progress phase and recovery phase could serve as evidence for definite diagnosis.
2.6.5 PCR Test of SARS Virus
Polymerase chain reaction (PCR), a type of molecular biological test, could identify SARS virus genes from various specimens (blood, feces, respiratory tract secretions, tissue sections, etc.), that is, SARS virus RNA.
2.6.5.1 Positive Results
Presence of any of the following three circumstances could be SARS virus positive:
1.
Clinical specimens from at least two different sites are tested positive (nasopharyngeal secretions and feces).
2.
The same clinical specimens collected by at least 2 days apart are tested positive (two or more specimens of nasopharyngeal excretions).
3.
The same clinical specimen is tested positive by two different methods or in different laboratories.
4.
Repeated PCR examination indicated positive.
2.7 Clinical Diagnosis
2.7.1 SARS Diagnosis and Treatment Regimens
2.7.1.1 Basis of Diagnosis
Epidemiologic History
1.
The patient has a history of intimate contact with patients or is one of the infected populations or consolidated having infected others by definite evidences.
2.
The patient had been to or lived in the areas with SARS patients and secondary infection epidemics.
Symptoms and Signs
The onset is acute and initial symptom is fever, with body temperature >38 °C, and occasionally accompanied by concurrent chillness. Patients may also suffer from headache, joint and muscular soreness, fatigue, and diarrhea, and generally there is no upper respiratory tract catarrhal symptom. Patients may have cough, mostly dry with scanty sputum, and chest dullness. Severe patients demonstrate accelerated respiration, shortness of breath, or obvious respiratory distress. Pulmonary signs are not obvious, and light moist rales may be audible or pulmonary consolidation observable.
Laboratory Examination
There is generally no increase of peripheral white blood cell count or decrease. Besides, the lymphocyte count is found generally declined.
Chest X-Ray Examination
Lungs present different degrees of patchy and plaque-shaped infiltration shadows or reticulate changes, which may progress rapidly into large patchy shadows. These commonly occur at multiple lobes or both sides, and absorption and dissipation of shadows are relatively slow. Pulmonary shadows and symptoms and signs may be inconsistent. If the test indicates negative, reexaminations shall be conducted after 1–2 days.
Effects of the Antibiotics Treatment
There are no remarkable responses to antibiotics.
2.7.1.2 Criteria for Clinical Diagnosis
Criteria for Diagnosis of Suspected Cases
Patients in compliance with any of the following three circumstances are diagnosed as suspected cases.
1.
The patient has a history of intimate contact with patients, or is one of the infected population, or is confirmed having infecting other people by concrete evidences, who also manifest aforementioned clinical symptoms but not high white blood cell count by test of peripheral blood.
2.
The patient has been to or lived in areas reported with infectious SARS patients and patients suffering from secondary infections 2 weeks before the disease onset, who also have abovementioned clinical symptoms and consistent pulmonary shadows on chest X-ray films with the abovementioned characteristics.
3.
Despite the lack of epidemic data, the patient has abovementioned clinical manifestations and not high peripheral white blood cell count, as well as pulmonary shadows on chest X-ray that accord with abovementioned characteristics.
In other words, the patient conform to the aforementioned 1 (1) + 2 + 3 or 1 (2) +2 + 4 or 2 + 3 + 4.
Criteria for Diagnosis of Clinically Diagnosed Cases
In case of any of the three following circumstances, the patient could be clinically diagnosed with SARS.
1.
The patient has a history of intimate contact with patients, or is one of the infected population, or is confirmed having infecting other people by concrete evidences, who also manifest aforementioned clinical symptoms and pulmonary shadows on chest X-ray image.
2.
The patient has been to or lived in areas reported with infectious SARS patients and patients suffering from secondary infections 2 weeks before the disease onset, who also have abovementioned clinical symptoms, not high peripheral blood white cell count and pulmonary shadows on chest X-ray films.
3.
The patient has been to or lived in areas reported with infectious SARS patients and patients suffering from secondary infections 2 weeks before the disease onset, who also have abovementioned clinical symptoms, pulmonary shadows on chest X-ray films, and no obvious response to anti-infectious treatment.
In other words, the patient conform to aforementioned 1 (1) + 2 + 4 or 1 (2) +2 + 3 + 4 or 1 (2) + 2 + 4 + 5.
2.7.2 Clinical Classification and Staging
2.7.2.1 Criteria for Classification of Clinically Diagnosed Cases
Light Type
The conditions are mild without pulmonary fibrosis and other sequela. The prognosis is good.
Common Type
Patients have typical clinical manifestations of the early phase, progression phase, and recovery phase. The onset is acute, and the first symptom is fever, with body temperature generally >38 °C. Besides, the patients have no obvious respiratory distress or hypoxemia. Some patients are auscultated with slight moist rales or observed with pulmonary consolidation. The prognosis is good without sequelae.
Severe Type
Severe type accounts for about 30 %. It is same with the common type in clinical process but presents severe conditions and rapid progression. Some cases may progress to acute pulmonary injury or ARDS, rapidly incurring respiratory failure or even death. The diagnosis could be reached in case of any of the following three circumstances:
1.
Dyspnea adult respiratory frequency is ≥30 times /min, accompanied by one of the following conditions:
The chest imaging shows that the total surface of multilobar lesions or foci occupies more than 1/3 of the two lungs on orthotopic imaging.
Conditions progress, with the focal area increased by over 50 % within 48 h or accounting for over 1/4 of the two lungs on orthotopic imaging.
2.
Obvious hypoxemia is detected, with the oxygenation index lower than 300 mmHg.
3.
Shock or multi-organic dysfunction syndrome occurs.
Miscellaneous
There are still some atypical cases of this disease.
2.7.2.2 Criteria for Staging of Clinically Diagnosed Cases
Early Phase
This generally refers to the first 1–7 days. The onset is acute and initial symptom is fever. Half of the patients are accompanied by the nonspecific systemic symptoms such as chillness, headache, and joint and muscular soreness.
Progression Phase
This phase spans the day 8–14 of the disease course. Infectious toxic symptoms such as fever, fatigue, muscular soreness continue to exist or even aggravate. Patient’s body temperature rises, possibly to 39 °C or higher in a short time, and the high fever is persistent. Lung lesions demonstrate progressive exacerbation. A few patients (10–15 %) may develop ARDS, which is life threatening.
Recovery Phase
It mostly takes place at day 15–21 of disease course. Most patients have good prognosis after recovery for about 2 weeks. Some severe patients could gradually recover within 2–3 months after discharge.
2.8 Imaging Techniques and Protection
2.8.1 Chest Imaging Techniques of SARS
2.8.1.1 Conventional Chest X-Ray Examinations
These mainly encompass standing chest X-ray and bedside chest X-ray, which are economic and effective examination methods and first optional examination for preliminary diagnosis and reexamination. Mobile X-ray bedside imaging should be applied for patients under observation and inpatients. As lung disease of SARS patients progress rapidly, chest X-ray reexamination within a short period could help observe changes of conditions, commonly once every 1–2 days at the early phase and progression phase. Regular chest X-ray also need to be conducted during recovery phase so as to ascertain absorption and dissipation of lesions, residual foci, and pulmonary interstitial fibrosis.
2.8.1.2 Chest CT Scan
For SARS patients, CT scan generally is not a preferred method and, if necessary, could be conducted under strict disinfected quarantine. If the foci could not be absorbed for a long term in SARS recovery phase or patients still have symptoms but normal chest presentations, CT scan need to be carried out for further observation as it can better visualize the subtle pulmonary interstitial changes, such as lung interlobular septum thickening, intralobular septum thickening, subpleural linear shadow, and small ground-glass-density lesion and regional and segmental bronchiectasis, and therefore is helpful for clinical diagnosis of pulmonary interstitial fibrosis. Thin-layer CT scan or HRCT scan can better visualize intrapulmonary low-density small lesions, thus contributory to early diagnosis of pulmonary interstitial fibrosis. CT examination could also aid identification of other concurrent lung lesions.
2.8.2 Protection and Quarantine of Department of Radiology
Medical staff in the room of imaging examination and department of radiology shall prevent infections in strict compliance with SARS disinfection and prevention requirements and meanwhile conscientiously implement X-ray protection.
2.8.2.1 Protection Requirements of Photographs at Bedside or Fever Clinic
1.
Ward shall be equipped with bedside X-ray machine; Imaging for all SARS inpatients shall be conducted in wards and patients shall wear masks.
2.
The personal protection for imaging technician should be subject to the level-two protection requirements and, when necessary (imaging for critically ill patients), to level-three protection requirements.
3.
X-ray film magazine should be put into the isolation bag before imaging (one isolation bag for each person).
4.
The imaging technicians should sterilize their hands before return to the radiological department and then remove protective clothing, gloves, and protective glasses at the designated place. They should wash hands thoroughly, gargle, take a shower, and change clean working clothes before work.
2.8.2.2 Disinfection and Protection of Department of Radiology
1.
The department must strengthen interior ventilation and air disinfection . Ultraviolet irradiation may be assumed at night, 2–3 times per day, 30 minutes per time, and peracetic acid spray conducted 2 times per day.
2.




Rigorous isolation measures: all subjects must wear masks. The operation staff must wear protective masks, gloves, and gowns, with masks changed every 4 h and gowns replaced in time, and should use disposal bed sheet and shoe covers, and dispose of and replace them timely after the examination.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree