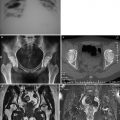
Fig. 6.1
Acute hepatitis, with balloon-like change and acidophilic change of the hepatocytic plasm as well as spots of focally necrotic hepatocytes. H&E, ×200
2.
Changes at the portal area
The portal inflammation is mostly slight or moderate, with inflammatory cell infiltration. The infiltrated cells are predominantly small lymphocytes and commonly small quantities of neutrophilic granulocytes and eosinophilic granulocytes.
Chronic Hepatitis B
The Parenchymal Lesions
1.
Periportal changes: interface inflammation
Except for slightest chronic hepatitis, the inflammatory infiltration in the cases of other chronic hepatitis extends from the portal area into the neighboring parenchyma. The liver cells around the portal area are then damaged to show interface inflammation. In addition, fibrous septum may extend out of the portal area.
2.
Lobular lesions
Different degrees of hepatocellular damages and inflammatory response occur in deep liver parenchyma, which is known as lobular lesions or lobular hepatitis. Lobular lesions are commonly manifested as spots of focally necrotic hepatocyte (Fig. 6.2). However, fused necrosis and bridging necrosis may also be observable. In addition, ground-glass-like liver cells (Fig. 6.3) as well as small round or oval adenoid cluster formed by liver cells, hepatocellular rosette, can also be observable.
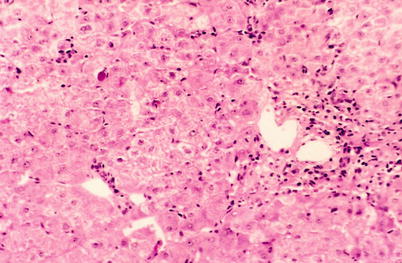
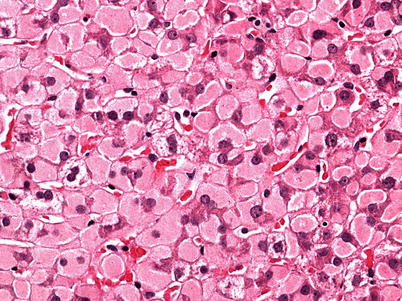
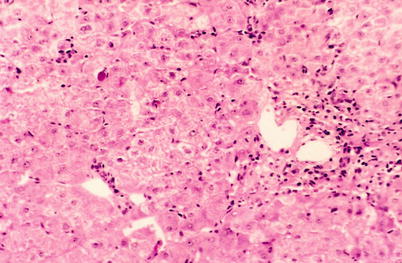
Fig. 6.2
Intralobular multiple spots of focally hepatocyte necrosis. H&E × 100
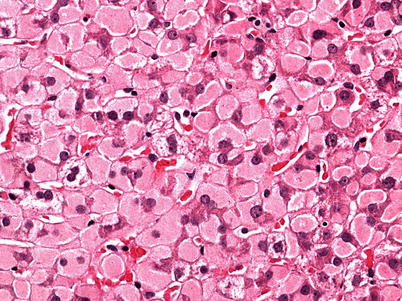
Fig. 6.3
Ground-glass-like hepatocytes. H&E × 400
Changes at the Portal Area
In most small portal areas, different degrees of lymphocytic infiltration can be observed, commonly with a small quantity of plasmocytes but rarely neutrophilic granulocytes. The portal area is commonly enlarged with accompanying different degrees of fibrosis. The bile ducts within hepatic lobule may be damaged, sometimes with observable bile ductule proliferation.
Based on the inflammation of the portal area and the interface as well as intralobular inflammatory activeness and fibrotic degree, the inflammatory activeness is graded as G0 ~ 4 and fibrosis is staged as S0 ~ 4 (Figs. 6.4, 6.5, 6.6, and 6.7). Chronic hepatitis can be defined as mild, moderate, and severe based on inflammatory activeness.
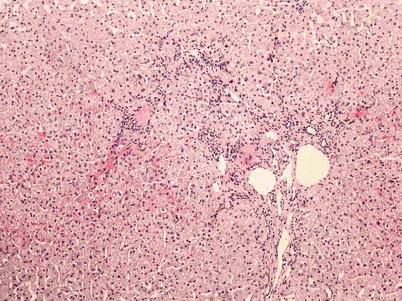
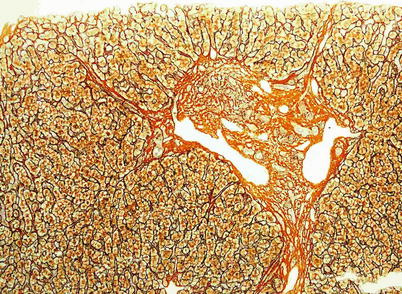
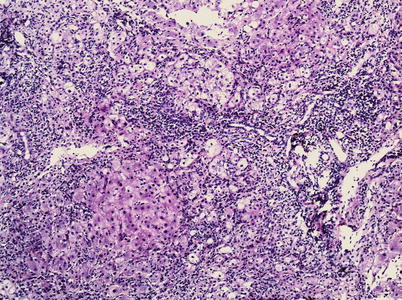

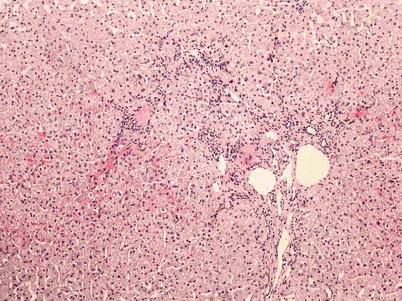
Fig. 6.4
Enlarged portal area with interface inflammation and the inflammatory activeness graded as G2. H&E × 100
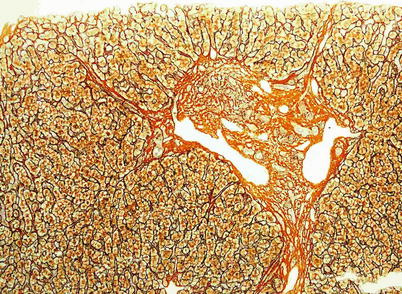
Fig. 6.5
Fibrosis at the portal area with accompanying formation of septum and fibrosis staged as S2. Reticular fiber × 200
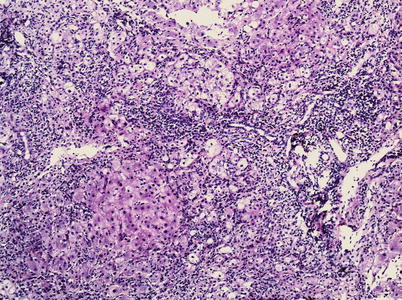
Fig. 6.6
Extremely enlarged portal area with severe interface inflammation and the inflammation activeness graded as G4. H&E × 100

Fig. 6.7
Early stage of liver cirrhosis with formation of pseudolobule. Gorden & Sweets, ×100
Detection of HBV at Liver Tissue Section
By immunohistochemistry, the expression of HBsAg, HBcAg, Pre-sl, HBeAg, and HB×Ag in hepatocytes can be detected (Figs. 6.8 and 6.9).
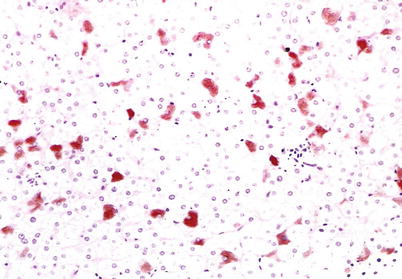
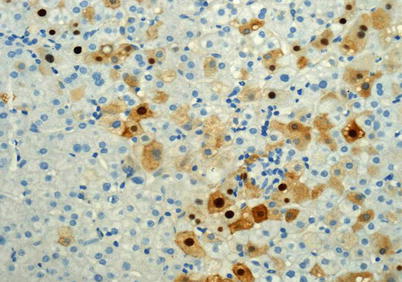
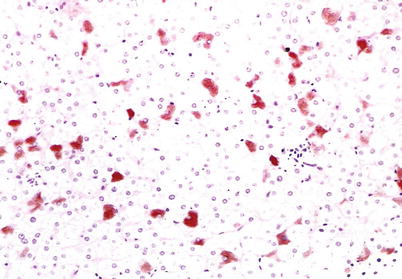
Fig. 6.8
Expression of HBsAg in hepatocyte as plasma and inclusion. Immunohistochemistry × 100
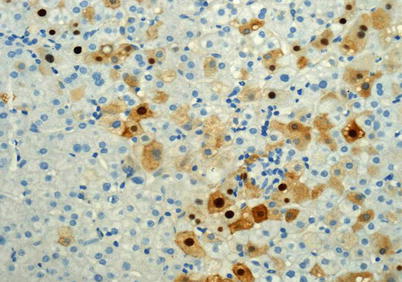
Fig. 6.9
Expression of HBcAg in hepatocyte as cytoplasm and nucleus. Immunohistochemistry × 400
6.4.2.3 Pathology of Hepatitis C
The pathologic changes of hepatitis C resemble to those of other types of hepatitis, showing inflammation and necrosis of the liver cells as well as infiltration of lymphocytes. Hepatitis C commonly develops into chronic condition.
Acute Hepatitis C
Histologically, acute hepatitis C resembles to acute hepatitis induced by other types of hepatitis viruses. Under a light microscope, acidophilic degeneration of plasma is obvious with formation of apoptotic bodies, which commonly scatter near the central vein. The portal area and the hepatic lobule are shown with infiltration of lymphocytes, plasmocytes, and even neutrophilic and eosinophilic granulocytes. In some cases, the infiltration of lymphocytes within the hepatic sinus appears like strings of beads. In the cases with dense lymphocytes in the portal area, formation of lymphatic follicles can be observed.
Chronic Hepatitis C
Chronic hepatitis C is histologically characterized by: (1) aggregation of lymphocytes in the portal area (Fig. 6.10), (2) damages to the small bile ducts, (3) hepatocyte fat degeneration (Fig. 6.11), and (4) activation of the hepatic sinus cells.
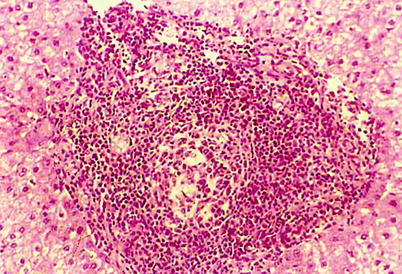

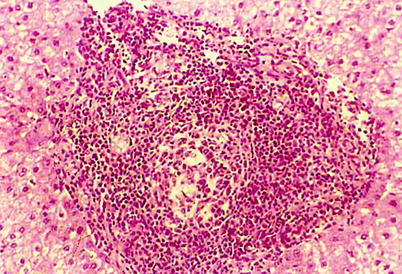
Fig. 6.10
Chronic hepatitis C with infiltration of dense lymphocytes in the portal area and formation of lymphatic follicles. H&E × 200

Fig. 6.11
Scattering distribution of fatty degenerated hepatocytes in the hepatic lobules. H&E × 200
Molecular Pathological Examination
In liver tissue, the detection rate of hepatitis C-related antigens is low and the percentage of hepatocytes with positive antigen is also low. HCAg is expressed as nucleus and plasma (Fig. 6.12). Due to highly variant genes of HCV, the positive rates of HCV RNA in the liver tissue by in situ hybridization are commonly inconsistent.
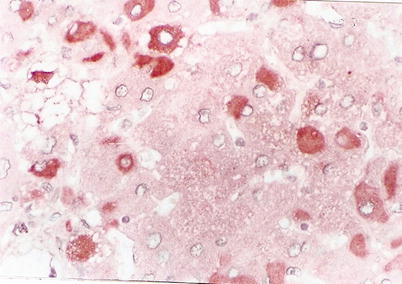
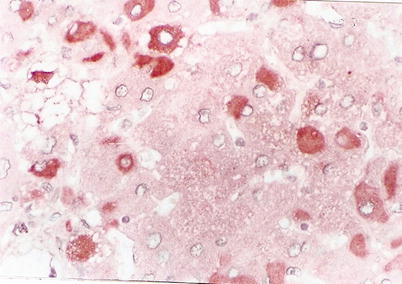
Fig. 6.12
Expression of HCV NS3Ag-positive signal in hepatocyte plasma. Immunohistochemistry × 400
6.4.2.4 Viral Hepatitis D
Simplex HDV infection is extremely rare. Histologically, acute and chronic hepatitis D resemble to that of other types of acute and chronic hepatitis, with the same modes of necrotic inflammation and fibrosis. In most cases, HDV and HBV infections are concurrent or overlapping, with more serious histological changes than simplex HBV infection. The histological changes include balloon-like changes, more hepatocytes with focally distributed acidophilic change fatty degeneration, more serious focal necrosis, fragment-like necrosis, bridging necrosis, and multilobular fusing necrosis. Severe interface inflammation is commonly serious.
6.4.2.5 Hepatitis E
The histologic changes of hepatitis E resemble to those of hepatitis A, with classical and bile-stasis changes of lobular hepatocytes in the cases of acute hepatitis. The classical pathological changes include spots of hepatocellular focal necrosis, formation of apoptotic body, balloon-like change, as well as infiltration of lymphocytes in hepatic lobule and the portal area (Fig. 6.13). Some of the bile-stasis-type lesions resemble to those of hepatitis A, with cholangiolar bile stasis and adenoid structural changes of the hepatocytes. However, the hepatocyte degeneration and necrosis are not so obvious as those in the cases of classical acute hepatitis. Although the infiltrated inflammatory cells are predominantly lymphocytes, large quantities of neutrophilic granulocyte and plasmocyte can be observed to infiltrate in the hepatic lobule and the portal area (Fig. 6.14). No fibrosis can be observed in the portal area. The inflammatory response of Kupffer cell proliferation in the hepatic lobule is mild. The hepatocytes are shown with fatty degeneration and bile stasis, and formation of bile thrombus in bile capillaries is common.
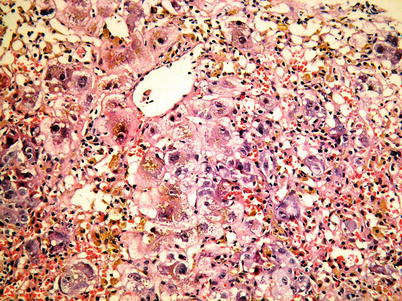
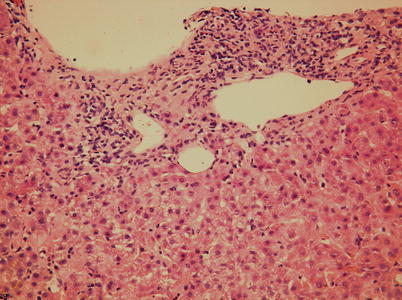
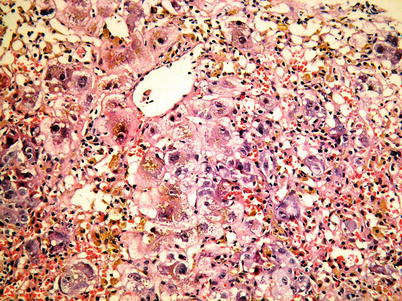
Fig. 6.13
Balloon-like change of intralobular hepatocyte, bile stasis, and inflammatory cell infiltration. H&E × 400
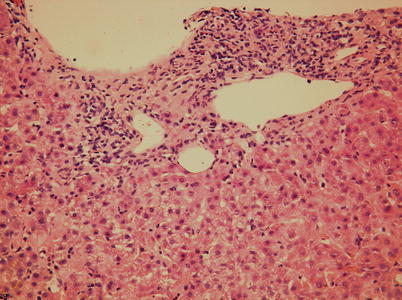
Fig. 6.14
Infiltration of predominant lymphocytes in the portal area, with observable plasmocytes. H&E × 200
6.5 Clinical Diagnosis
The clinical diagnosis of viral hepatitis is mainly based on the epidemiological data, clinical manifestations, and laboratory tests.
6.5.1 Epidemiological Data
For the diagnosis of hepatitis A and hepatitis E, data about local prevalence of hepatitis should be collected and analyzed. In addition, the history of intaking possibly contaminated food should also be taken into account. And the history of vaccination preventing hepatitis A and E acts as reference for the diagnosis.
For the diagnosis of hepatitis B and C, the history of transfusion blood or blood products and the history of unsterilized injection should be reported. Other histories, such as history of vaccination preventing hepatitis B and history of family hepatitis B virus infection, especially history of HBsAg positive in mother of infant patient, facilitate the diagnosis of hepatitis B.
6.5.2 Etiological Diagnosis
6.5.2.1 Hepatitis A
Hepatitis A can be etiologically diagnosed based on the following finding: (1) serum anti-HAV IgM positive in patients with acute hepatitis, (2) at least four times increase of serum anti-HAV antibody titer at the acute and convalescent stages, (3)detected hepatitis A virus particle in the stool or detected hepatitis A virus antigen, and (4) detected hepatitis A virus RNA in serum or stool. Patients with any ONE positive finding of above conditions can be defined with recent infection of hepatitis A.
6.5.2.2 Hepatitis B
Chronic HBV infection can be categorized into the following conditions:
1.
Chronic hepatitis B
Based on HBeAg positive or negative, chronic hepatitis B can be categorized into HBeAg-positive chronic hepatitis B and HBeAg-negative chronic hepatitis B.
2.
HBV carriers
The chronic HBV carriers are defined to be HBsAg and HBV DNA positive as well as HBeA or anti-HBe positive. Within 1 year, follow-ups show serum ALT and AST levels to be within normal range for at least consecutive three times, with negative findings by biopsy of liver tissue.
The nonactive HBsAg carriers are defined to be serum HBsAg positive, HBeAg negative, anti-HBe positive or negative, and HBV DNA lower than the lowest limit. Within 1 year, consecutive follow-ups show at least three times of ALT level within the normal range. Histological examination of the liver tissue demonstrates the Knodell hepatitis activity index (HAI) to be lower than four or qualitatively mild condition by other semiquantitative scoring systems.
3.
Latent chronic hepatitis B
Latent chronic hepatitis B refers to the condition of serum HBsAg negative but serum/liver tissue HBV DNA positive with clinical manifestations of chronic hepatitis B. In addition to HBV DNA positive, the patients may also show serum anti-HBs, anti-HBe, and/or anti-HBc positive. However, in about 20 % patients with latent chronic hepatitis B, HBV DNA is positive, but all other serological indicators are negative.
6.5.2.3 Hepatitis C
In patients with both HCV RNA and anti-HCV positive, the diagnosis of hepatitis C can be defined. Anti-HCV negative but HCV RNA positive can be detected in patients receiving hemodialysis or intense immunosuppressive therapy.
6.5.2.4 Hepatitis D
The patients with current HBV infection and serum HDV antigen or HDV antibody IgM or high titer of serum HDV antibody IgG or serum HDV RNA positive can be diagnosed with hepatitis D. Otherwise, the patients with current HBV infection and intrahepatic HDV antigen or HDV RNA positive can be diagnosed with hepatitis D.
6.5.2.5 Hepatitis E
The diagnosis of hepatitis E can be defined based on detected anti-HEV IgG and/or IgM antibodies. In the cases with high titer of anti-HEV IgG during the acute stage, or with a change from low titer to high titer along with the progress of the condition, or with a change from high titer to low titer and even negative, the diagnosis of acute HEV infection can be made.
6.6 Imaging Diagnosis of Hepatitis and Its Related Diseases
6.6.1 Ultrasound
6.6.1.1 Ultrasound of Severe Viral Hepatitis
In the cases of severe viral hepatitis, the ultrasonic demonstrations are characteristic, including:
1.
Shrinkage of the liver with abnormal shape and unsmooth liver capsule or with folds.
2.
Echo from the hepatic parenchyma is reticular, patchy, or granular due to interlace scattering large masses of necrosis and residual liver tissues, which is known as maplike liver or worm-bitten-like liver (Fig. 6.15).


Fig. 6.15
Severe hepatitis. Echo from the liver parenchyma is worm-bitten-like due to the scattering large masses of necrosis
3.
When the supporting framework collapses due to large masses of necrosis, the portal vein may be twisted to shift its primary position. Such a sign demonstrated at the early stage or to be serious indicates a poor prognosis.
6.6.1.2 Ultrasonic Changes of the Common Conditions Complicating Viral Hepatitis Portal Hypertension
1.
The luminal diameter of the trunk of portal vein ≥14 mm indicates occurrence of portal hypertension. In the cases with complicating dilation of superior mesenteric vein and splenic vein as well as splenomegaly, the diagnosis of portal hypertension can be defined.
2.
Decreased blood flow rate in the portal vein (<14 ~ 15 cm/s) or the blood flow directing away from the liver indicates occurrence of portal hypertension.
3.
Formation of portosystemic collateral circulation with luminal diameter of the coronary vein >5 mm indicates the occurrence of portal hypertension. The reopening of adult umbilical vein is demonstrated as extending duct-like non-echo structure from sagittal part of the portal vein toward the abdominal wall, with portal-vein-like blood flow signal inside.
Pleural Effusion and Ascites
Pleural effusion is ultrasonographically demonstrated as crescent-shaped or large flaky liquid dark area at the inferior thoracic cavity. Ascites is ultrasonographically demonstrated as flaky irregular liquid dark area at the inferior abdominal cavity, anterior liver, interspace between the liver and kidney, as well as interspace between the spleen and kidney.
6.6.1.3 Viral Hepatitis and Liver Cirrhosis
Direct Signs
1.
The liver section is morphologically abnormal, with disproportional liver lobes. The volume of liver is diffusively enlarged (at the early stage) or shrunk (at the advanced stage), with obvious shrinkage of the posterior segment of the right liver lobe. The lateral segment of the left liver lobe and the caudate lobe is commonly demonstrated with proliferation and swelling.
2.
The surface of the liver is unsmooth, with wavelike, serration-like, or humplike change.
3.
The echo from liver parenchyma is disordered, with unevenly distributed intrahepatic light spots. The echo is thickened and enhanced, possibly with reticular and poorly defined patches of changes. Repeated hepatocellular destruction and regeneration can be demonstrated as low-echo or high-echo nodules with three-dimensional profile.
4.
The intrahepatic tubal system is demonstrated with no abnormality at the early stage. At the advanced stage, the lumen of hepatic vein is thinner or uneven, possibly with compressed vascular wall. The hepatic vein is twisted, stiff, or even absent. The hepatic artery may be compensatorily widened, and the minor branches of intrahepatic portal vein are twisted and thinner, with enhanced echo from the vascular wall. The trunk of portal vein as well as its secondary- and third-graded branches is widened, sometimes with portal thrombus and portal sponge degeneration.
Indirect Signs
1.
Spleen
The spleen is displayed with enhanced echo from its parenchyma, with a thickness of ≥40 mm and a length of ≥120 mm. Even megalosplenia may be shown. The splenic vein is dilated and tortuous. In the cases with obviously dilated splenic vein, the splenic hilum can be demonstrated as a honeycomb-like no-echo area, with splenic vein engorgement. The lumen of the splenic vein may exceed 9 mm and may even larger than the lumen of portal vein.
2.
Formation of ascites
Ascites is commonly demonstrated as liquid no-echo area with favorable sonolucency. A small quantity of ascites is commonly found anterior or peripheral to the liver and sometimes can be observed at the lower abdomen. Occasionally, a small quantity of ascites is confined anterior to the liver, at the hepatorenal recess, or at the lower abdomen.
3.
Portal hypertension
Portal hypertension may be demonstrated as:
(a)
increased luminal diameter of the portal vein, with the luminal diameter of the portal venous trunk mostly being ≥14 mm. The luminal diameter does not change along with respiration. Colored Doppler ultrasound shows decreased velocity of the blood flow in the portal vein, possibly with bidirectional blood flow or reverse directional blood flow, the velocity of blood flow in the portal vein mostly within 15 cm/s.
(b)
Splenomegaly.
(c)
Open collateral circulation, including open umbilical vein and dilated coronary vein (the left gastric vein).
4.
Thinner hepatic vein
In patients with liver cirrhosis, the hepatic vein can be demonstrated to be twisted, thinner, or poorly defined. The normal three-phase oscillogram of the hepatic vein may be absent, which may be related to decreased adaptability of the hepatic vein induced by liver parenchyma fibrosis around the hepatic vein and its fatty degeneration.
5.
Short-circuit formation of the hepatic artery and vein
By ultrasonography, the hepatic artery and vein are demonstrated with shortened filling period, mostly less than 12 s.
6.6.1.4 Primary Liver Cancer
Ultrasonic Typing of HCC and the Direct Signs
The typing of HCC by ultrasound resembles to its pathological typing, including the huge-mass type, the nodular type, and the diffuse type.
The Huge-Mass Type
A huge solid mass in the liver parenchyma can be demonstrated, with a diameter of >10 cm. The mass is mostly found at the right liver lobe, rarely with an exophytic growth. It has vascularized pedicle attached to the liver.
The mass mostly grows in a spherically expanding manner, with well-defined but irregular boundary (Fig. 6.16). In rare cases, the mass has an infiltration-like growth in the liver parenchyma, with poorly defined boundary. In the cases with isointense echo of the mass, the diagnosis can be missed.


Fig. 6.16
The huge-mass type HCC. A mass in size of 14.3 cm × 13.5 cm was demonstrated at the right liver lobe in expansive growth, with well-defined but irregular boundary
In most cases, the mass has hyperintense echo, which is thick and uneven. Within the hyperintense echo, heterogenous hypointense echo is mostly present with necrotic liquefied cavities at the center.
Around the mass, small nodules are sometimes demonstrated with a diameter of 1–2 cm.
At marginal mass, hypointense acoustic halo is demonstrated, which is thin with poorly defined external boundary but well-defined internal boundary.
The typical sign of rapid-in-rapid-out of the contrast agent can be demonstrated by ultrasonography.
The Nodular Type
The nodules in the liver parenchyma are relatively small, whose diameter is commonly <5 cm. The lesion is mostly singular but rarely multiple.
Within the nodules, the echo is commonly heterogenous, which may be hypointense, isointense, hyperintense, or mixed intense (Fig. 6.17).


Fig. 6.17
The nodular type of HCC. It was demonstrated with oval-shaped hyperintense echo nodule in the liver parenchyma, which had well-defined boundary and peripheral light acoustic halo
The nodules are commonly round or oval, with well-defined boundary.
The nodules with hyperintense echo are demonstrated with lateral acoustic shadow. However, the nodules with isointense or hypointense echo may be demonstrated with slightly enhanced posterior echo.
By colored Doppler, the nodules are demonstrated with inner or peripheral arterial blood flow signal.
By ultrasonography, the typical sign of rapid-in-rapid-out of the contrast agent can be demonstrated.
6.6.2 CT Scan
6.6.2.1 Hepatocirrhosis After Viral Hepatitis by CT Scan
In China, the most common hepatocirrhosis includes hepatocirrhosis after viral hepatitis and schistosomiasis hepatocirrhosis.
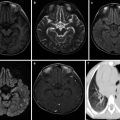
Direct Signs (Fig. 6.18)
Fig. 6.18
Direct signs of hepatocirrhosis after viral hepatitis. (a) Plain scan; (b) arterial phase; (c) portal venous phase; (d) delayed phase
1.




Change of liver size
Extensive fatty degeneration at the early stage causes enlargement of the liver. However, at the advanced stage, the liver shrinks with disproportional liver lobes (especially transverse diameter ratio of the caudal lobe to the right lobe). The right lobe is commonly demonstrated with atrophy and the caudal lobe with compensatory enlargement. The left lobe is normal or shrinks or has its lateral segment enlarged.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree