Fig. 4.1
Necrosis of pulmonary tissue and infiltration of inflammatory cells H&E ×100
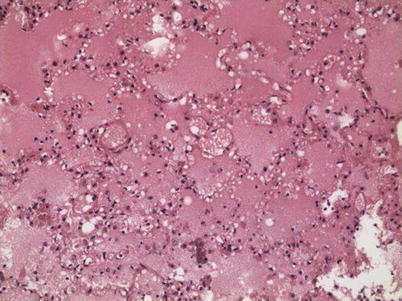
Fig. 4.2
Pulmonary edema, with the alveolar cavity filled by homogeneous acidophilic exudates H&E ×100
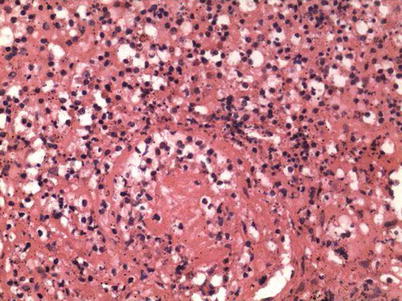
Fig. 4.3
Necrosis of pulmonary vascular wall and infiltration of inflammatory cells H&E ×200
Observation by Electron Microscopy
Virus particles can be observed both within and out of the infected cells in alveolar cavity of pulmonary tissue. The virus is round or oval in shape with a diameter of averagely about 88 nm, and some viruses are surrounded by spikelike structure in a length of about 12 nm.
4.3.2.2 Other Major Systems
Cardiovascular System
The heart is slightly heavier. Under a light microscope, myocardial cells are degenerated, with myocardial breakage, myocardial interstitial edema, infiltration of small quantity or no inflammatory cells, and degeneration of atrial ganglion cells (Figs. 4.4, 4.5, and 4.6).
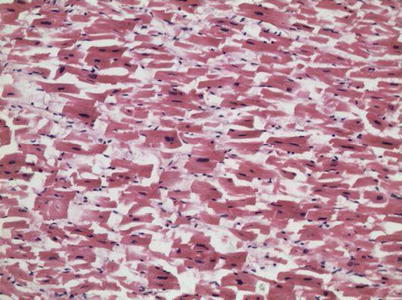
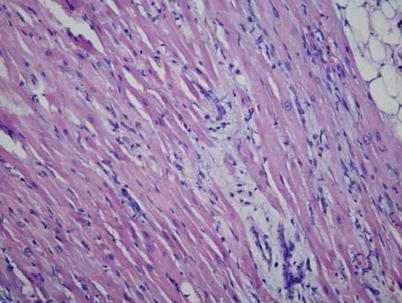
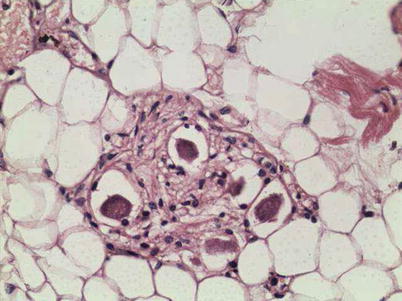
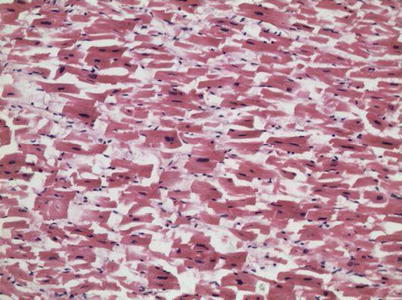
Fig. 4.4
Myocardial breakage, degeneration of myocardial cells, and myocardial interstitial edema H&E ×400
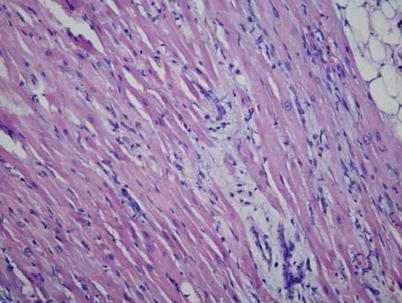
Fig. 4.5
Infiltration of inflammatory cells at the myocardial tissue space H&E ×200
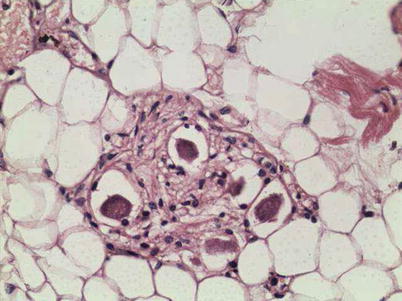
Fig. 4.6
Degeneration of atrial ganglion cell H&E ×200
Digestive System
The liver can be observed with congestion, focal hepatocytic swelling and fatty degeneration, and infiltration of small quantity mononuclear cells at the portal area. Erythrocytophagy can be observed (Fig. 4.7).
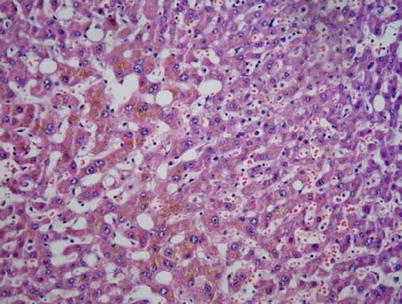
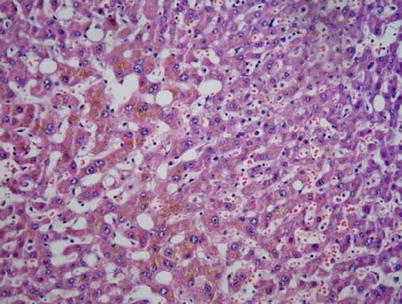
Fig. 4.7
Bullous fatty degeneration of hepatocytes, cholestatic hepatocytes, and dilated hepatic sinus H&E ×200
Urinary System
The kidney can be observed with congestion. Under a light microscope examination, glomerular congestion is observed, with edema of renal tubular epithelial cells but no microthrombus and renal tubular necrosis.
Central Nervous System
The pathological changes include cerebral edema and congestion, with visible hemorrhagic focus, focal liquefactive necrosis at the capsule, and neuronal degeneration (Fig. 4.8).
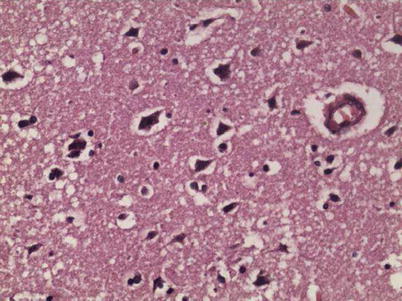
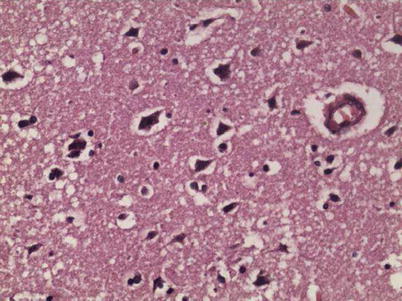
Fig. 4.8
Degeneration of brain nerve cells H&E ×400
Lymphoid Hematopoietic System
Hemophagocytic phenomenon can be observed at some lymph nodes and bone marrow (Fig. 4.9). The spleen can be observed with reduced lymphocytes, histiocytosis, and hemophagocytic phenomenon (Fig. 4.10).
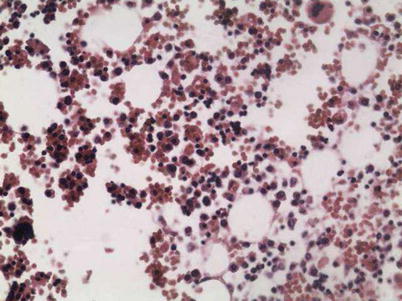
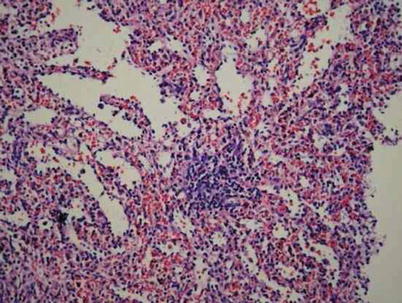
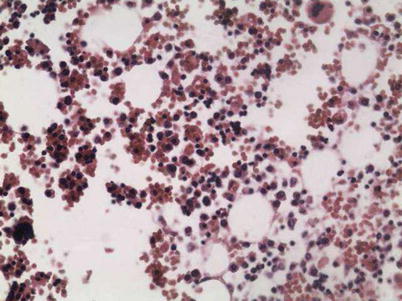
Fig. 4.9
Prominent hemophagocytic phenomenon at bone marrow H&E ×200
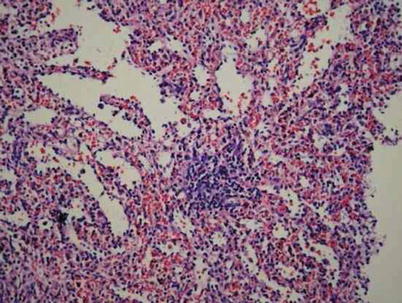
Fig. 4.10
Dilation and congestion of splenic sinus, atrophy of splenic corpuscle, and decreased lymphocytes H&E ×200
4.3.2.3 Secondary Infection
The patients with influenza A (H1N1) can develop secondary bacterial and fungal infections. The pathogenic bacteria are mainly gram-positive coccus.
4.3.2.4 Molecular Pathology
The nucleoprotein antigen of influenza A (HIN1) virus is located at the nucleus and cytoplasm of infected cells, including epithelial cells at airway, submucosal glands of airway, and detached and lining epithelial cells at alveolus. In addition, the antigen can also be found at the hyaline membrane and rarely vascular endothelial cells. Double labeling has revealed that the target cell of viral infection is pulmonary epithelial cells, predominantly type II alveolar epithelial cells (co-labeled with cytokeratin) and occasionally macrophages.
No viral antigen of influenza A (H1N1) virus is immunohistochemically detected in nonrespiratory tissue. By RT-PCR, the nonrespiratory tissue is also detected negative for influenza A (H1N1) virus.
4.4 Clinical Symptoms, Signs, and Laboratory Tests
Influenza A (H1N1) is a self-limited respiratory disease. Its clinical manifestations resemble to those of seasonal influenza, being mild in most patients. However, the patients from high-risk populations are more likely to develop into severe cases and even death.
4.4.1 Incubation Period
The incubation period of influenza A (H1N1) generally lasts for 1–7 days, mostly 1–3 days, which is longer than that of common influenza and avian influenza.
4.4.2 Clinical Symptoms and Signs
The patient usually experiences influenza-like symptoms, including fever (axillary temperature ≥37.5 °C), sore throat, runny nose, nasal congestion, cough, expectoration, headache, general soreness, and fatigue. In some cases, the patients experience vomiting and/or diarrhea. In rare cases, the patients only experience mild upper respiratory symptoms with no occurrence of fever.
The signs mainly include pharyngeal congestion and swollen tonsils.
4.4.3 Laboratory Tests
4.4.3.1 Peripheral Blood Test
Total WBC count is commonly within or lower than normal range. In some severe pediatric cases, the total WBC count may increase. The common cases commonly show normal or lower WBC count, while the severe cases show normal or increased peripheral WBC count. The increase of WBC count in severe cases may be related to complicated infections. It should be paid close attention that, compared to common cases, the severe cases have obviously decreased percentage and absolute count of peripheral blood lymphocytes. Peripheral blood lymphocyte count <800 cells/ml is a high-risk factor for patient with influenza A (H1N1) to develop respiratory failure. The decrease of both percentage and absolute count of peripheral lymphocytes is an indicator for early prediction.
4.4.3.2 Blood Biochemistry
Blood Biochemistry
The blood biochemistry for liver function is commonly normal in most patients. Only in rare cases, the levels of aspartate aminotransferase (AST), alanine aminotransferase (ALT), and lactate dehydrogenase (LDH) can be tested with increase.
Myocardial enzyme of creatine kinase (CK) exists in the cytoplasm and mitochondria of skeletal muscle, heart, brain, and other tissues, which is an important kinase directly related to intracellular energy transformation, muscle contraction, and ATP regeneration. Its level increases in the cases with myocardial damage.
The blood glucose level in both critical cases and death cases is higher than that in severe cases, which may be related to responses of host to stress.
Electrolyte
In some cases, hypokalemia or hypocalcemia occurs. Relevant studies have demonstrated that hypocalcemia is an important indicator predicting poor prognosis of influenza A (H1N1).
4.4.3.3 Assay for Cellular Immunity
The infection of influenza A (H1N1) virus can cause allergic reaction. In critical cases, the serum cytokine significantly increases, with increased permeability of pulmonary and cerebral vascular vessels, to cause respiratory failure and pulmonary edema. Therefore, the test for serum cytokines plays an important role in assessing conditions of influenza A (H1N1) and guiding clinical prevention and treatment.
4.4.3.4 Etiological Examination
Test for Viral Nucleic Acid
The test for viral nucleic acid is currently the main diagnostic examination for influenza A (H1N1). The respiratory specimens, including throat swabs, nasal swabs, nasopharyngeal or tracheal extracts, and sputum, are tested by using RT-PCR (more favorably real-time RT-PCR). The cases of influenza A (H1N1) show positive results.
Virus Isolation
In the cases of influenza A (H1N1), the pathogenic virus can be isolated from respiratory specimens. In the cases with influenza A (H1N1) complicated by viral pneumonia, the virus can also be isolated from the lung tissue.
Serum Antibody Test
In the cases of influenza A (H1N1), dynamic tests of double sera specimens show at least four times increase of the neutralizing antibody specific to influenza A (H1N1) virus. The result may facilitate to define the diagnosis and the retrospective diagnosis.
4.5 Clinical Diagnosis
The patients with influenza A (H1N1) experience different degrees of fever, cough, expectoration, chest distress, shortness of breath, fatigue, headache, and myalgia, all of which are collectively referred to as the flulike symptoms. Although the influenza A (H1N1) virus is a new mutant of influenza virus, the symptoms of infected patients can be hardly distinguished from infections of respiratory syncytial virus, parainfluenza virus, rhinovirus, adenovirus, Coronavirus, and Legionella pneumophila. Therefore, the diagnosis cannot be defined based only on the symptoms, but needs to combine findings of specific laboratory tests, such as serological test, viral nucleic acid test, and pathogen isolation.
4.5.1 Suspected Cases
The case with the following ONE condition can be diagnosed as a suspected case:
1.
The patient has a history of close contact to patient suspectively or definitively diagnosed with influenza A (H1N1) at its infectious stage within 7 days prior to the onset of influenza-like symptoms. Close contact refers to attending to patients with influenza A (H1N1) in its infectious stage with no effective protection; living together with the patient and exposure to the same environment with the patient; and direct contact to the airway secretions, body fluids, and other contaminated utensils from the patient.
2.
The patient has a history of visiting the country or region with epidemic of influenza A (H1N1) (continuous spread of virus from person to person and community-based prevalence and outbreak) within 7 days prior to the onset of influenza-like symptoms.
3.
The patient experiences influenza-like symptoms and shows positive to test for influenza A (H1N1) virus, but infection of previous influenza virus subtypes has not been further excluded.
The cases with ONE of the above three conditions should be etiologically tested for influenza A (H1N1), if possible.
4.5.2 Clinically Diagnosed Cases
The clinical diagnosis should be made based only on the following condition. During the same epidemic event of influenza A (H1N1), the patient with influenza-like symptoms has not definitively diagnosed by laboratory test but has been excluded from other diseases with influenza-like clinical manifestations. Such patients can be clinically diagnosed as influenza A (H1N1).
Outbreak of influenza A (H1N1) refers to abnormally increased occurrence of influenza-like disease in one region or unit within a short period of time, and the disease is defined to be influenza A (H1N1) by laboratory tests.
If possible, the clinically diagnosed patients should receive etiological examination.
4.5.3 Definitively Diagnosed Cases
The cases with influenza-like symptoms and at least ONE of the following laboratory findings can be definitively diagnosed as influenza A (H1N1).
1.
The viral nucleic acid of influenza A (H1N1) virus is tested positive by real-time RT-PCR or RT-PCR.
2.
The serum level of neutralizing antibody specific to influenza A (H1N1) is tested with at least four times increase.
3.
The influenza A (H1N1) virus is isolated.
4.5.4 Diagnosis of Severe and Critical Cases
4.5.4.1 Severe Cases
The severe cases can be defined based on ONE of the following conditions.
1.
Persistent fever lasting from more than 3 days, accompanied by severe cough, purulent and/or bloody sputum, or chest pain
2.
Rapid respiratory rate, dyspnea, cyanotic lips
3.
Consciousness changes, including delayed response, drowsiness, restlessness, and convulsions
4.
Severe vomiting and diarrhea, dehydration
5.
Radiological findings of pneumonia-like signs
6.
Rapid increases of myocardial enzyme levels, such as creatine kinase (CK), creatine kinase M isoenzyme (CK-MB), etc.
7.
Obviously aggravated previous underlying disease
4.5.4.2 Critical Cases
The critical cases can be defined based on ONE of the following conditions:
1.
Respiratory failure
2.
Septic and toxic shock
3.
Multiple organ dysfunction
4.
Other severe clinical conditions in need of monitoring treatment
4.6 Selection of Radiological Modalities
Influenza A (H1N1) is commonly complicated by diseases of respiratory and central nervous system. The selection of radiological modalities is mainly based on the two systems.
4.6.1 Radiology of the Respiratory System
4.6.1.1 Chest X-Ray
The suspected cases should receive upright posterior-anterior chest X-ray. For the severe cases of inability going to the radiology department, a bedside chest X-ray can be performed to assess the condition at a posture of sitting or lying. If possible, a special stand for upright chest X-ray or seated chest X-ray can be used. The children patients capable of standing should receive upright chest X-ray. For patients unable of standing due to severe conditions, seated chest X-ray is preferred.
Indications for Bedside Radiological Examination
The indications for bedside radiological examination are as the following:
1.
Persistent fever lasting for at least 3 days
2.
Cough with/without expectoration
3.
Positive finding in viral nucleic acid test for influenza A (H1N1)
4.
Signs of pulmonary inflammation by the first radiological examination
When a patient with suspected diagnosis of influenza A (H1N1) experiences above conditions 1, 2, and 4, a bedside radiological examination should be performed. If a patient with suspected diagnosis of influenza A (H1N1) experienced the above condition 3, the bedside radiological examination is NOT necessary.
Protection Principles During Bedside Radiological Examination
The patients, radiological technicians, and other healthcare workers should be protected against radiohazards. Data revealed that the average radiation dose at the chest surface of the patient by a bedside X-ray machine is 1.45 mGy/time, and its maximum dose is 3.39 mGy/time. The radiation dose by other digital chest X-ray machines is about (0.36 ± 0.05) mGy/time. The radiation dose of bedside X-ray machine is significantly different from that of other digital chest X-ray machine.
Protective Measures Against Cross-Infection
Before entering into the isolation ward, the radiological technicians should receive training for knowledge and skills about disinfection and isolation. The procedures should be constantly improved.
The patients with influenza A (H1N1) experience rapid changes of lung lesions. Therefore, reexamination of chest X-ray within a short period of time facilitates to assess the condition. During the convalescent stage, chest X-ray should be regularly performed to assess the absorption of lesions and the residual lesions.
4.6.1.2 Chest CT Scan
In recent years, based on the application of new detectors and new algorithm for image reconstruction, the low-dose CT scan can be routinely performed. CT scans are favorable in detecting chest lesions and their characteristics, which can be applied for patients whose diagnosis cannot be defined by chest X-ray. CT scan can display occult lesions posterior to the heart shadow and at the posterior costophrenic angle, which can effectively avoid misdiagnosis and increase the detection rate of the lesions.
4.6.2 Radiology for the Central Nervous System
MRI has the absolute advantage in displaying lesions at the central nervous system due to its capabilities in multiparameter imaging, 3D imaging, and functional imaging. Therefore, MRI is the choice of radiological modalities for the examination of central nervous system. CT scan is applied only when MRI is inapplicable.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree