Head, Neck, and Craniofacial Pathology
Ramesh S. Iyer, MD
LEARNING OBJECTIVES
1. Distinguish between periorbital and orbital cellulitis.
2. Identify retinoblastoma on CT or MR.
3. Identify features of acute, chronic, and fungal sinusitis on CT.
4. Generate a differential diagnosis for congenital midline nasal masses.
5. Identify juvenile nasal angiofibroma on contrast-enhanced CT or MR.
6. Generate a differential diagnosis for cervical cystic lesions.
7. List at least two clinical or imaging features distinguishing thyroglossal duct cysts from branchial cleft cysts.
8. Describe the two most common types of branchial cleft cysts.
9. List the two most common pediatric cervical tumors.
10. Identify sagittal craniosynostosis on CT.
INTRODUCTION
There are a large variety of congenital, inflammatory, and neoplastic disorders that arise in the head and neck. There is similarly complex anatomy and embryology for each of the compartments. An exhaustive discussion covering all of these topics is beyond the scope of this textbook. Instead, we will present an overview of the pathologies that are most common or specific to children. Crosssectional imaging is typically required for disease characterization.
ORBITAL PATHOLOGY
Periorbital and orbital cellulitis
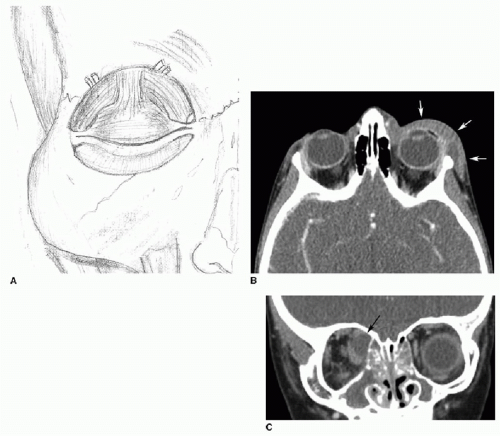
Infections of the orbit are divided by their relationship to the orbital septum. The septum is a fibrous membrane that is continuous with the bony orbit and the tarsal plate of the eyelids (Fig. 35.1A). It serves as a barrier between the orbit and the soft tissues external to the orbit.1 Periorbital cellulitis refers to infection anterior to the septum, involving the superficial soft tissue of the eyelids. Orbital cellulitis involves infection posterior to the septum. This distinction carries great clinical importance— orbital cellulitis increases the risk of blindness, abscess, intracranial extension, sinovenous thrombosis, and death.2 Rhinosinusitis is by far the most common cause of pediatric orbital infections. Gram-positive bacteria—Staphylococcus and Streptococcus—are the typical causative organisms for orbital infections. Children present with unilateral erythema, swelling, and tenderness of the eyelid. Ophthalmoplegia, proptosis, and blurred vision should raise suspicion for orbital cellulitis and possible abscess.3
Contrast-enhanced CT or MR should be performed to assess for orbital cellulitis and its complications. In periorbital cellulitis, there is soft tissue thickening and edema exclusively anterior to the orbital septum (Fig. 35.1B). In orbital cellulitis, there are similar inflammatory changes posterior to the septum involving either the intraconal or extraconal compartments (within or outside of the extraocular muscles, respectively) (Fig. 35.1C). A common complication of orbital cellulitis is subperiosteal abscess. This frequently involves the medial orbital wall, or lamina papyracea, in association with ethmoid sinus disease.1,2,4
Periorbital cellulitis is managed with oral antibiotics. The majority of cases of orbital cellulitis, including those with small abscesses, are successfully treated with intravenous antibiotics alone. Surgical intervention is generally required only for large abscesses or for intracranial extension of disease.3,5,6
Retinoblastoma
Retinoblastoma is the most common intraocular tumor of childhood. Its incidence is 1 in 17,000 live births. This aggressive malignancy arises from the immature retina, and 95% of cases are diagnosed in children less than 5 years old. Retinoblastoma is divided into two broad groups—sporadic and heritable. In both groups, there is a mutation in the tumor suppression gene RB1 located on chromosome 13q14. Sixty percent of retinoblastomas arise from sporadic mutations, while 40% are the result of heritable mutations. Heritable disease is associated with earlier onset of retinoblastoma—often less than 2 years old—and bilateral and multifocal tumors, along with increased risk of other malignancies. Sporadic mutations tend to cause solitary unifocal tumors.
About 5% of heritable cases also develop primitive neuroectodermal tumors (PNETs) of the suprasellar or pineal regions, called “trilateral retinoblastomas.” The hallmark clinical sign of retinoblastoma is leukocoria, or white pupillary reflex, on fundoscopic examination.7, 8, 9 and 10
About 5% of heritable cases also develop primitive neuroectodermal tumors (PNETs) of the suprasellar or pineal regions, called “trilateral retinoblastomas.” The hallmark clinical sign of retinoblastoma is leukocoria, or white pupillary reflex, on fundoscopic examination.7, 8, 9 and 10
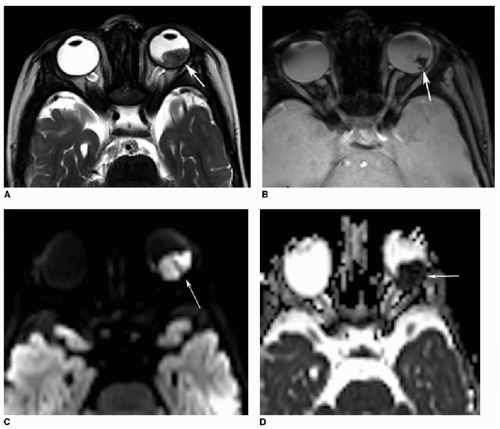
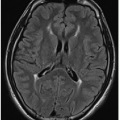
On CT, retinoblastoma is usually a high-density soft tissue mass within the globe, exhibiting calcification and contrast enhancement. Calcification is the most important differentiating feature of retinoblastoma, observed in over 95% of cases. Contrastenhanced MR has become the mainstay for diagnosis and staging of retinoblastoma (Fig. 35.2). The tumor is slightly T1-weighted hyperintense and T2 hypointense compared to the surrounding fluid in the posterior chamber of the globe, and enhances heterogeneously. Susceptibility-weighted imaging (SWI) is exquisitely sensitive for lesional calcification. The tumor often restricts diffusion because of its high cellularity. In less than 10% of children, there is extraocular extension of the lesion through the sclera that forms the outer portion of the globe. In these cases, retinoblastoma may invade the optic nerve or disseminate intracranially through either CSF (more common) or hematogenous pathways.7, 8, 9, 10, 11, 12 and 13
The treatment of retinoblastoma has evolved substantially over time. Historically, patients usually presented with advanced disease and survival rates were dismal. Enucleation was the mainstay of therapy for many years. Recently, focus has shifted from preservation of life to that of sight.9 Newer therapies include systemic chemotherapy, plaque radiotherapy, cryotherapy, and photocoagulation. Enucleation is performed when there is no reasonable chance of vision preservation. The cure rate for noninvasive intraocular retinoblastoma is now 90% to 95%. However, prognosis drops precipitously for extraocular spread of tumor.9,13
Optic nerve glioma
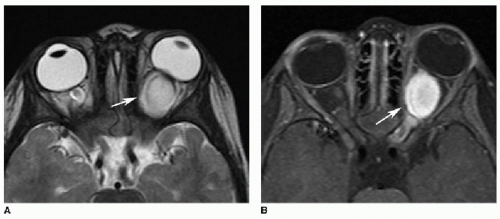
Optic nerve glioma is the most common primary tumor of the optic nerve in children. This lesion may present either sporadically or in the context of NF type 1 and is also discussed in Chapter 32. There is fusiform enlargement of the optic nerve, with T1-weighted hypointense and T2-weighted hyperintense signal on MR (Fig. 35.3A). Enhancement is either homogeneously avid or peripheral with central necrosis (Fig. 35.3B). Patients with sporadic optic nerve gliomas typically have unilateral disease, but there is more frequent posterior extension to involve the optic chiasm, hypothalamus, and other intracranial structures. NF1-associated optic nerve gliomas are more often bilateral, but are usually confined to the optic nerve.1,14
Other orbital tumors
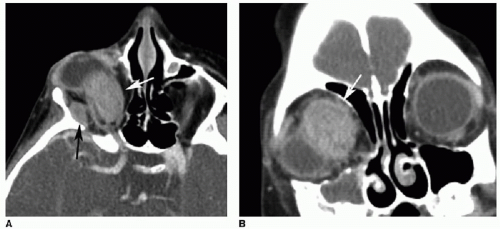
Rhabdomyosarcoma is a common pediatric extraocular tumor that arises from primitive mesenchymal cells that differentiate into skeletal muscle. The head and neck are among the most common locations for this malignancy. Within the head and neck, the orbits and paranasal sinuses are frequently involved. The mean age of presentation is 6 years. Most orbital rhabdomyosarcomas are extraconal, but intraconal components may occur. On CT, the mass is isodense to muscle with heterogeneous enhancement (Fig. 35.4). On MR, most tumors are T1-weighted hypointense and T2-weighted hyperintense to muscle and enhance heterogeneously.1,2,15
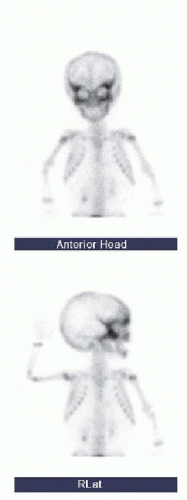
Neuroblastoma is the most common metastatic tumor in young children. The orbital walls, skull base, and calvarial sutures are common sites of disease in the head and neck. The patient may experience sudden pain or proptosis due to tumoral hemorrhage.2 Diffuse orbital metastases from neuroblastoma are associated with the “raccoon eyes” sign, referring to either a clinical appearance or a scintigraphic finding. The clinical appearance is a result of bilateral periorbital ecchymoses. The imaging sign, seen on both bone scans and MIBG studies, reflects confluent radiotracer deposition around bilateral orbital walls (Fig. 35.5).16,17
SINONASAL PATHOLOGY
Choanal atresia
Choanal atresia is the most common congenital abnormality of the nasal cavity. It represents obstruction of the posterior opening of the nasal cavity. It is caused by bony obstruction in 30% of patients and a mixed bony-membranous anomaly in the remaining 70%. It is unilateral in about half of cases. Neonates with choanal atresia are identified after inability to pass a nasogastric tube. Noncontrast CT is the modality of choice, which shows medial bowing and thickening of the lateral nasal walls and thickening of the posterior vomer (Fig. 35.6). The condition is treated with surgical repair.18,19
Sinusitis
Acute bacterial sinusitis is a common complication of viral upper respiratory tract infections. Bacterial sinusitis is clinically suspected when a child has persistent nasal discharge or cough lasting
longer than 10 days, a worsening course, or severe onset such as a high fever. Uncomplicated bacterial sinusitis is typically a clinical diagnosis, and imaging is not recommended. Contrast-enhanced CT or MR is reserved for when orbital or CNS complication such as abscess is suspected.20 Noncontrast CT examinations are also performed to screen for sinusitis in immunosuppressed children with fever of unknown origin.
longer than 10 days, a worsening course, or severe onset such as a high fever. Uncomplicated bacterial sinusitis is typically a clinical diagnosis, and imaging is not recommended. Contrast-enhanced CT or MR is reserved for when orbital or CNS complication such as abscess is suspected.20 Noncontrast CT examinations are also performed to screen for sinusitis in immunosuppressed children with fever of unknown origin.
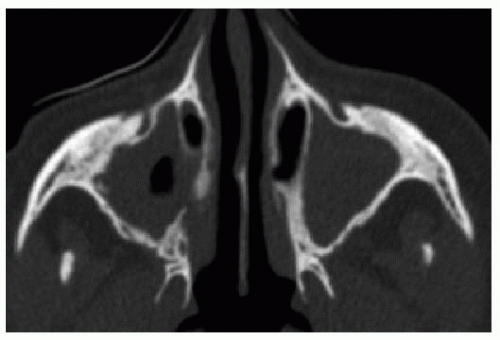
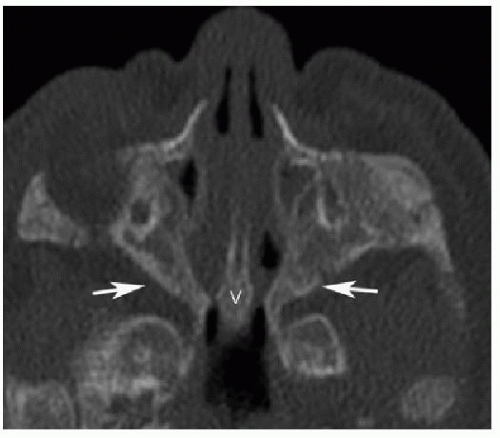 FIG. 35.6 • Choanal atresia in a female neonate. Axial CT image illustrates medial bowing and thickening of the lateral nasal walls (arrows) and thickening of the posterior vomer (V). |
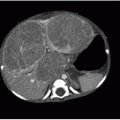
Acute sinusitis on imaging may manifest as air-fluid levels or frothy fluid within one or more paranasal sinuses (Fig. 35.7). It should be noted, however, that sinus fluid and mucosal abnormalities are very common in asymptomatic young children, and therefore, clinical correlation is required. In chronic sinusitis, the sinus walls may be become thickened and sclerotic along with mucosal thickening (Fig. 35.8). In allergic sinusitis, the sinus becomes expanded with high-density contents, and polyps may be present.
The treatment of acute bacterial sinusitis generally consists of oral antibiotics for 10 to 14 days.20 Chronic sinusitis may be addressed with a longer course of antibiotics, nasal irrigation, decongestants, and intranasal or oral corticosteroids.21
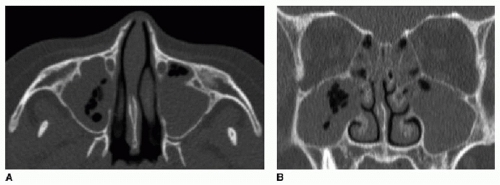 FIG. 35.7 • Acute sinusitis in a 12-year-old female. Axial (A) and coronal (B) noncontrast CT images show fluid throughout the paranasal sinuses. Note the frothy contents in the maxillary sinuses. |
Congenital midline nasal masses
The differential diagnosis of congenital midline nasal masses includes three conditions: nasal dermoid, nasal glioma (cerebral heterotopia), and encephalocele. They result from a persistent dural reflection through the embryologic foramen cecum, located between the nasal bones and developing nasal cartilage. They present as dimples or soft tissue masses anywhere from the tip of the nose to the glabella, the region between the eyebrows (Fig. 35.9). MRI is preferred to assess for intracranial extension. CT better shows the relationship between the lesion and the nasal bones.22,23
Sixty percent of such lesions are nasal dermoids. A dermoid forms when the dural projection adheres to the skin and forms a dimple, with an underlying dermal sinus tract that may track all the way back to the cranial vault at the foramen cecum (Fig. 35.10). Dermoids may be located anywhere along this sinus tract. Hair protruding from a skin dimple is a pathognomonic clinical sign. Nasal dermoids may become infected but are




Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree