2Imperial College London, London, UK
- CT is the investigation of choice in the ER (NB Skull XRs are NOT indicated in head injuries)
- Delayed management of head injuries is a major cause of preventable death
- Have a low threshold to CT or repeat a CT
- MRI is rarely necessary in the acute setting
Computed tomography (CT) is the investigation of choice for cranial imaging in the emergency setting. The main reasons for CT scanning in emergency setting are for trauma, stroke or TIA, suspected subarachnoid haemorrhage or meningitis. Intravenous (IV) contrast is used in perfusion imaging following stroke and if space occupying lesions are detected. Other than in stroke, magnetic resonance imaging does not feature in the acute setting.
Plain skull radiographs (SXRs) have no role in the emergency setting in adults.
CT technique
MDCT allows the spiral acquisition of data through the head with multiplanar reconstruction (MPR). Using different algorithms and altering window settings and MPR software has allowed more detailed analysis depending on which structures are being analysed. Most systems will have automatic selection for window levels to optimise viewing of different structures (Figure 8.1a–c)
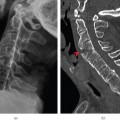
Figure 8.1 (a) Soft-tissue settings; (b) bone window settings demonstrates pneumocephalus with pockets of air (arrow head) and a fracture through the left petrous temporal bone (arrow); (c) bony algorithm and bone windows makes images sharper for bony structures.
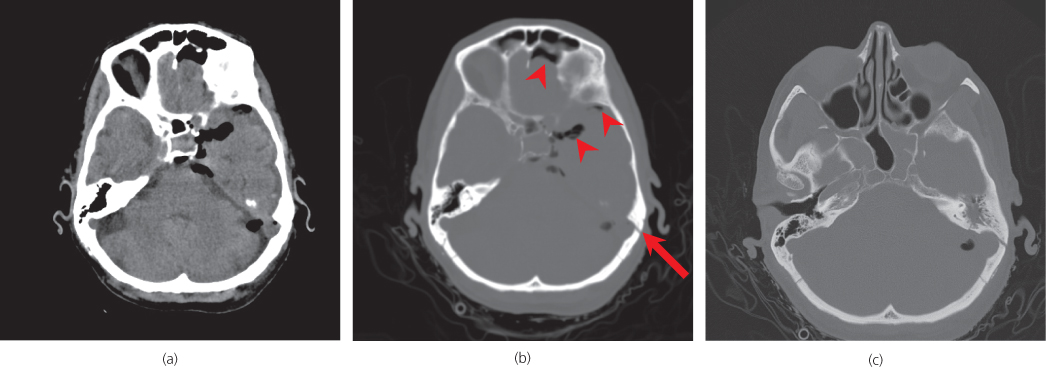
Figure 8.2 (a),(b) 1, Skull left; 2, frontal lobe; 3, anterior horn of left lateral ventricle; 4, third ventricle; 5, occipital horn of the left lateral ventricle; 6, head of caudate nucleus; 7, thalamus; 8, internal capsule; 9, lentiform nuclei; 10, insular; 11, sylvian fissure; 12, occipital lobe; 13, pineal gland—typically calcified; 14, interhemispheric fissure; 15, orbit; 16, temporal lobe; 17, temporal horn of the left lateral ventricle; 18, left cerebellar hemisphere; 19, fourth ventricle; 20, brain stem; 21, basilar artery; 22, pituitary stalk. (c) Beam hardening artefacts—linear black streaks (arrow heads). (d) Partial voluming—the brain parenchyma appears of lower density in the middle scan.
Initially a scout image (scanogram) is obtained and then axial images are obtained without IV contrast (non-enhanced CT). These images are then reviewed and a decision is made whether to give intravenous contrast (contrast enhanced CT) (Box 8.1).
- Non-contrast CT
- Trauma
- Stroke
- Subarachnoid haemorrhage
- Other intracranial haemorrhage
- Hypoxia
- Anoxia
Consider contrast if suspect:
- Meningitis
- Encephalitis (acute confusion)
- Raised intracranial pressure
- Obstructive hydrocephalus
- Following neurosurgery
Give contrast if suspect:
- Focal mass lesion
- Encephalitis
- Subdural empyema
- Venous sinus thrombosis
- Known primary malignancy
- HIV infection
ABCs systematic assessment
- Adequacy
- Airspaces
- Bones
- Brain
- CSF
- Dura
- Eyes
- Face/ Foreign body
- Survey (review areas)
The ABC assessment is a simple systematic approach, which is easy to remember. It is important to review key areas, analogous to the secondary survey.
The key to diagnosis is knowledge of basic anatomy. Understanding and determining if a lesion is within the brain parenchyma (intra-axial) or in the dural or cerebrospinal fluid spaces (extra-axial) is crucial.
It is important to be able to recognise typical common imaging artefacts such as ‘beam hardening’ in the posterior cranial fossa and ‘partial voluming’ in the frontal lobes. Beam hardening can be caused by a lot of bone, as present in the base of the skull vault, or by metal, where the XRs do not penetrate as well. The data manipulation of these areas can be spurious and cause straight high density lines to run across parts of the image. (Figure 8.2c arrow) Conversely in areas of low density, such as CSF within sulci, if the data is not acquired in thin enough slices, part of the low density of the CSF can be included in the data manipulation, giving a false lower density in the brain parenchyma. (Figure 8.2d)
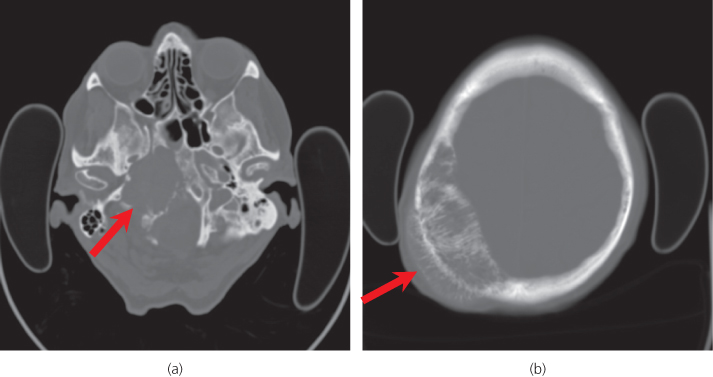
Figure 8.3 (a) Large lytic metastasis of the right skull base. (b) Haemangioma of the right skull vault with coarse trabeculae and hair-on-end appearance.
Adequacy
- Has the patient moved excessively?
- Is repeating the scan going to improve the image?
- Has the top of the skull vault been included?
- Has the foramen magnum and all the intracranial contents been included?
- Would contrast be helpful?
Airspaces/bones Figure 8.3a,b
Look for:
- Sphenoid sinuses—an air-fluid level may indicate a base of skull fracture.
- Opacification of the paranasal sinuses—may be due to sinusitis, which may be the cause of a subdural empyema (infected subdural collection).
- Maxillary and ethmoid opacification—may be seen in facial fractures.
- Mastoid air cells—Fracture or infection leading to venous sinus thrombosis or abscess collection.
- Skull vault fractures (depressed or complex)—check for scalp soft tissue swelling as a marker of an acute injury.
- Focal bone lesions- primary bone tumour or metastases, myeloma
- Erosions at the skull base—foramina or pituitary fossa can be eroded in mass lesions
- Generalised skull vault thickening—Paget’s, sickle cell, anticonvulsant therapy, long term ventricular shunting, diffuse metastatic disease.
Brain
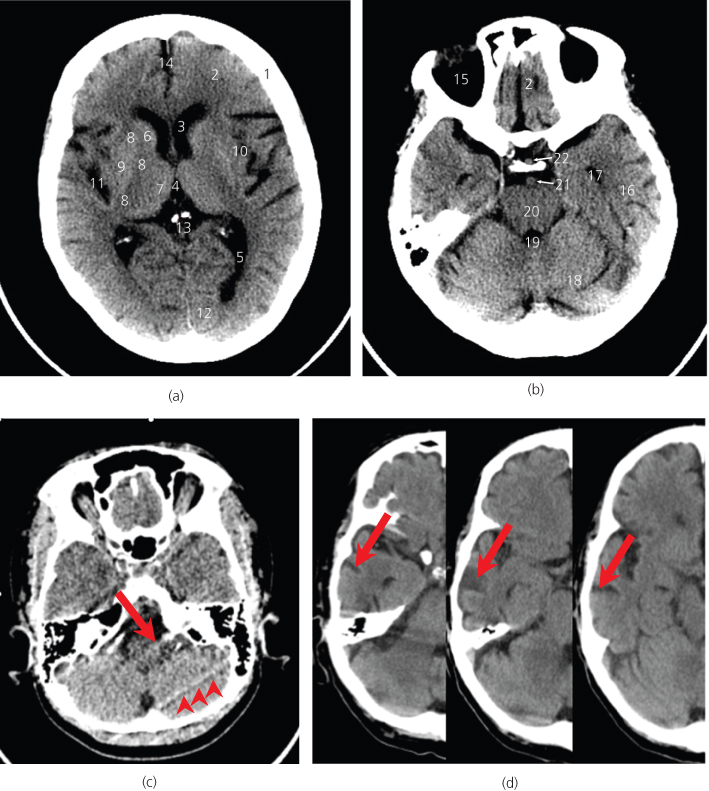
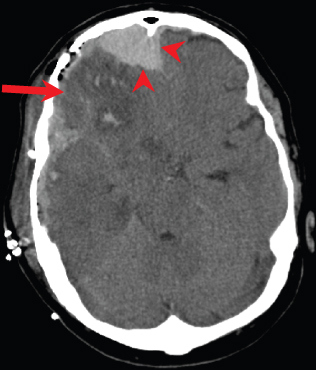
Examination of the brain parenchyma on every slice is necessary for evidence of low or high density lesions or for mass effect (Figure 8.4).
Figure 8.4 Head trauma with mixed density in the right frontal and temporal lobes with non-haemorrhagic contusions (low density areas) and haemorrhagic contusions (high density areas). Note also the right frontal extra-axial haematoma underlying the right frontal fracture (arrow heads).
Low density lesions
In the trauma setting, low density lesions such as non-haemorrhagic contusions or ‘shear’ injuries are typical. The latter include diffuse axonal injury which often occurs at the grey-white matter junction in the frontal and temporal lobes and in the corpus callosum, usually posteriorly.
In non-trauma cases, low density lesions may involve grey and white matter (such as infarcts, encephalitis and low grade gliomas) or white matter only. Demyelination and small vessel ischaemic disease in hypertension are common causes of white matter low density lesions.
Vasogenic oedema (Figure 8.5) is an area of low density around an abscess or tumour, which has finger like projections in to the white matter.
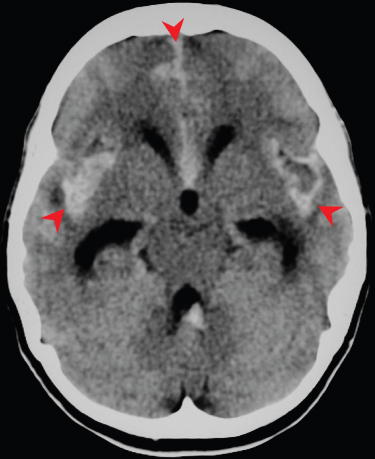
Diffuse low attenuation changes with reduced grey-white matter differentiation and associated generalised swelling usually indicates hypoxic brain injury—for example after cardiac arrest (Figure 8.6).
Other causes of focal low attenuation may be due to cystic lesions, for example, cystic tumours, such as pilocytic astrocytoma, or to areas of necrosis in more aggressive tumours such as glioblastoma multiforme. Similarly, an abscess has a low density core with a thin enhancing wall.
Figure 8.5 Vasogenic oedema. Finger-like areas of low attenuation involving white matter is typical in the presence of peripherally enhancing (arrow head) metastases.
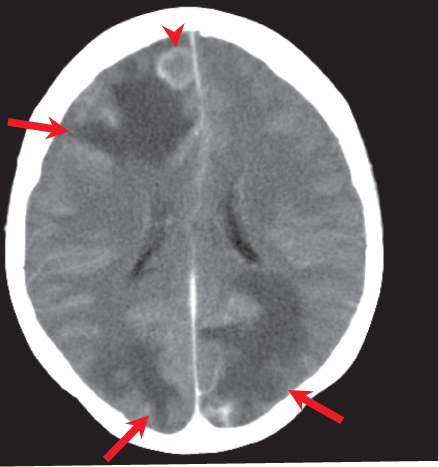
Figure 8.6 Severe hypoxic brain injury with generalised cerebral oedema. Symmetric low attenuation involving the basal ganglia, associated with cerebral swelling and global loss of the differentiation of grey and white matter.
High density lesions
High density lesions usually represent acute haemorrhage (Figure 8.7). Certainly from day 1 to 7, a haemorrhage will be of high attenuation. In the acute setting, there may be surrounding low density, for example, non-haemorrhagic contusion, venous infarction or haemorrhagic tumour. The density of the haemorrhage progressively reduces with time, such that it may not be conspicuous at three- four weeks. In cases of ongoing parenchymal bleeding or in the presence of a coagulopathy, hyperacute haemorrhage can be of low density and may form fluid levels and ‘swirls’. An acute haemorrhage may also be less dense than expected in the context of anaemia.
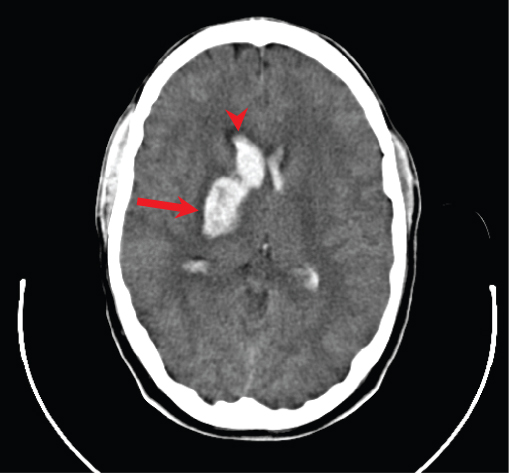
Figure 8.7 Acute parenchymal haemorrhage. High density acute haematoma in the right basal ganglia (arrow) but with intraventricular extension.
Alternatively, very high density areas may reflect calcification, possibly from congenital infection, or they could be related to tumour.
Lesions with high cellular density (Figure 8.8) (for example lymphoma) are often mildly hyperdense, and they usually have mass effect.
Figure 8.8 Mildly hyperdense mass (arrow) in the left cerebellar hemisphere with surrounding vasogenic oedema and mass effect (with effacement of the fourth ventricle) consistent with a highly cellular haemangioblastoma.
Mass effect
Deciding if a lesion has mass effect or if there is evidence of mass effect (without necessarily appreciating the causative lesion) is crucial. If a lesion has mass effect it causes distortion of adjacent structures, initially locally, but when more severe there is a more widespread effect.
- Gyral expansion
- Cerebrospinal fluid space effacement (local or generalised effect on sulci, basal cistern and ventricles)
- Subfalcine herniation
- Crowding of the foramen magnum
- Temporal uncal herniation, which may result in a posterior cerebral artery infarct.
CSF
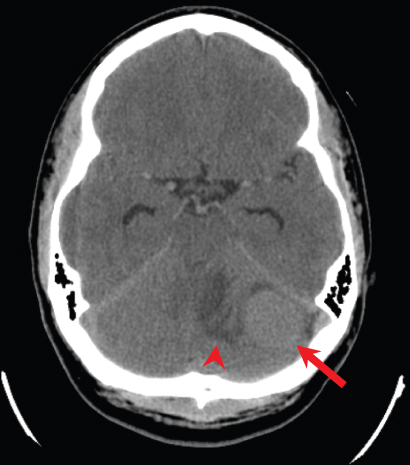
The ventricles, basal cisterns and sulci contain cerebrospinal fluid. All components should be assessed for signs of acute haemorrhage (high density) or mass effect. Acute haemorrhage in the basal cisterns, sulci with or without ventricles is a subarachnoid haemorrhage, the most common causes of which are trauma and cerebral aneurysm rupture (Figure 8.9). Take care to look in the dependent locations, particularly in the occipital horns of the lateral ventricles and the interpeduncular fossa.
Haemorrhage in the sulci results in high density linear lesions between the cortical gyri. Mass effect on the cerebrospinal fluid spaces usually results in the loss of symmetry, for example of the ventricular system or sulci. The spaces are relatively small in normal young patients, so changes may be subtle.
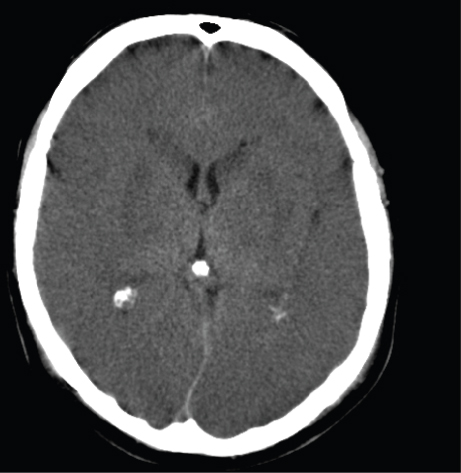
Hydrocephalus
In general, enlargement of the ventricular system may be a compensatory effect related to reduced volume of brain parenchyma seen in old age and certain degenerative conditions, or hydrocephalus. Acute hydrocephalus is usually associated with signs of mass effect such as effacement of sulci and periventricular oedema (low attenuation), and may be caused by obstruction to the flow of CSF somewhere along its pathway, for example at the foramen of Monro by a colloid cyst (Figure 8.10). In this case only the ventricles upstream from the obstruction will be dilated, and in this example only the lateral ventricles.
Figure 8.9 Communicating hydrocephalus with dilatation of all the ventricles in subarachnoid haemorrhage (extensive high density acute blood in the subarachnoid spaces).
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree