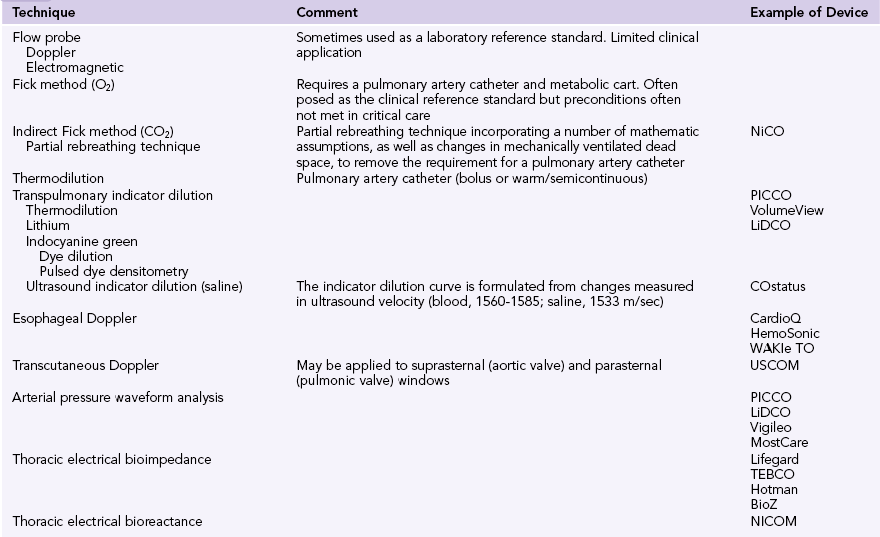
36 William Harvey: De motu cordis. In The circulation of the blood and other writings (1628), translated by Kenneth J. Franklin (1957), Chapter 8, pp 57-58. In critical care, the goals of hemodynamic monitoring include mainly detection of cardiovascular insufficiency and diagnosis of the underlying pathophysiology. At the bedside, clinicians are faced with the challenge of translating concepts such as preload, contractility, and afterload into determinants of stroke volume and hence cardiac output. Ultrasound and echocardiography offer unique insight into ventricular filling and systolic function. In recent years there has been a general trend away from invasive hemodynamic monitoring. This was initially motivated by published data suggesting an association between the pulmonary artery catheter (PAC) and excess mortality in critically ill patients.1 Despite specific risks, subsequent randomized controlled trials have not sustained the concerns about excess mortality.2 The PAC should not be regarded as obsolete. An overview of critical care hemodynamic monitoring would be incomplete without putting ultrasound in the context of the techniques available for estimating cardiac output, including nonultrasonic modalities. This broader topic is covered well in the literature3 and is outlined only briefly here. Demonstrating an association between any monitoring modality and improved outcome is challenging. Monitoring must be coupled with an effective change in therapy for a positive association to be observed. Clinical practice is characterized by the subtleties of interpretation, ongoing review, and titration of therapy to response. This does not translate easily into large-scale, randomized, controlled trial designs. Any form of hemodynamic monitoring (Table 36-1) should be viewed as an adjunct to the clinical examination and must be interpreted as an integration of all available data.3–5 These may include the patient’s mental state, urine output, and peripheral perfusion (temperature and capillary refill time). Heart rate, arterial blood pressure, jugular venous pressure (or central venous or right atrial pressure [RAP]), and electrocardiography should also be incorporated. Other adjuncts to the interpretation of hemodynamic data might include Svo2, Scvo2, lactate, blood gases, capnography, gastric tonometry, or other assessment of the microcirculation. Ultrasound indicator dilution is a novel application of ultrasound technology. Unlike transpulmonary thermodilution, which bases estimates of cardiac output on changes in blood temperature, ultrasound indicator dilution measures changes in ultrasound velocity. Normothermic isotonic saline is injected into a low-volume arteriovenous loop between arterial and central venous catheters. The change measured in ultrasound velocity (blood, 1560 to 1585; saline, 1533 m/sec) allows the formulation of an indicator dilution curve and calculation of cardiac output.6 As mentioned previously, observational studies raised questions about increased morbidity and mortality with the use of PACs1; however, subsequent randomized trials indicated that PACs are generally safe and may yield important information.2 The PAC has a trailblazing role in defining cardiovascular physiology and pathophysiology. The method provides “cardiodynamic insight” that other hemodynamic monitoring technologies still fail to elucidate. A PAC is not a therapy and cannot affect the prognosis, but it can be used to guide therapy. The usual clinical indications for placement of a PAC are shown in Box 36-1. A comprehensive echocardiographic examination is time-consuming. In the management of potentially unstable, critically ill patients, physicians will often prefer to focus their examination on pertinent variables. Several focused hemodynamic echocardiographic protocols have been developed and applied. Among others, these protocols include FOCUS (focused cardiac ultrasound7), ELS (Echo in Life Support8) and HART scanning (hemodynamic echocardiographic assessment in real time9). As well as being minimally invasive (transesophageal [TEE]) or noninvasive (transthoracic [TTE]), echocardiography also offers unique diagnostic insight into a patient’s cardiovascular status. The presence of intracardiac shunts renders many hemodynamic monitoring devices invalid. Such shunts may be difficult to diagnose without echocardiographic techniques. Likewise, pericardial effusions, collections, and tamponade can also be difficult to diagnose without echocardiography.
Hemodynamic monitoring considerations in the intensive care unit
Overview
Hemodynamic monitoring devices
Invasive hemodynamic monitoring
Echocardiographic hemodynamic monitoring