Hepatobiliary
Abdominal pain is consistently one of the top reasons that patients present to the ED.1 In 2009, 668970 ED visits resulted in a diagnosis of gallbladder or bile duct pathology. Overall, 39% of these cases required admission and 80% were diagnosed with acute gallbladder and bile duct-related conditions such as cholecystitis. When the emergency physician diagnosed gallstones without acute inflammatory conditions, 88% of cases were discharged from the ED.2 Consequently, emergency physicians who can effectively perform point-of-care ultrasound have the potential to efficiently impact the care of patients with right upper quadrant abdominal pain.
 CLINICAL CONSIDERATIONS
CLINICAL CONSIDERATIONS
The primary tools in the evaluation of acute hepatobiliary disease are ultrasound, hepatobiliary iminodiacetic acid scintigraphy (commonly referred to as HIDA scan or cholescintigraphy), computed tomography (CT), and endoscopic retrograde cholangiopancreatography (ERCP). Prior to the late 1980s and early 1990s, several imaging modalities were in use to diagnose hepatobiliary disease, such as oral and IV cholangiography. These methods were time consuming, required the ingestion or injection of potentially harmful contrast agents, and exposed the patient to radiation.3 Ultrasound largely replaced these imaging modalities in the 1990s. Ultrasound can be performed rapidly at the bedside and does not expose the patient to ionizing radiation. Ultrasound also has the highest sensitivity for detecting the presence of gallstones, while HIDA has a reportedly higher sensitivity for detecting the presence of acute cholecystitis.4 Data derived solely from ED patients, however, suggest that point-of-care ultrasound of the gallbladder may prove as accurate for the detection of acute cholecystitis as HIDA.5,6 HIDA has very limited utility for the detection of acute cholecystitis when the point-of-care ultrasound examination is normal.7 Although CT is limited by its inability to detect 25% of gallstones, CT may play a greater role when other causes of abdominal pain are being considered.8,9 ERCP is time consuming and resource heavy, and its complications include iatrogenic pancreatitis, perforation, and even death.
 CLINICAL INDICATIONS
CLINICAL INDICATIONS
Indications for clinicians to perform point-of-care hepatobiliary ultrasound include the evaluation of
 Biliary colic
Biliary colic
 Acute cholecystitis
Acute cholecystitis
 Jaundice and biliary duct dilatation
Jaundice and biliary duct dilatation
 Sepsis
Sepsis
 Ascites
Ascites
 Hepatic abnormalities
Hepatic abnormalities
BILIARY COLIC
In the United States, more patients undergo cholecystectomies (both elective and emergent) than appendectomies. Emergency physicians expect to see biliary pathology in up to a third of all patients with abdominal pain, making the differentiation of acute and subacute pathology important.10,11 The classic presentation of biliary colic portrays an obese woman of childbearing age with recurrent colicky pain in the right upper quadrant shortly after the consumption of a fatty meal. While gallstones are more prevalent in young, multiparous women than in young men, the effect of gender disappears with advancing age.12 In older patients, the pain does not wax and wane after meals but is constant and occurs mostly at night at predictable times, lasting for an average of 1–5 hours.13 Prospective data on the prevalence of gallstones and cholecystitis in the pediatric and adolescent population has not been reported. One study suggests that these patients do not have a classic presentation, are often misdiagnosed, and have a delay in diagnosis due to a low suspicion on the part of pediatric providers.14 Retrospective data on gallstones in this population note that the cause is often due to hemolytic anemia, long-term IV antibiotic therapy, or idiopathic in nature.15
Physiologic studies conducted on patients while they were undergoing cholecystectomy concluded that a majority of patients with cholelithiasis experience epigastric discomfort or dyspepsia with mechanical stimulation of the gallbladder. Symptoms may not migrate to the right upper quadrant until the inflamed gallbladder irritates the peritoneum.16–18 Patients with biliary disease may also complain of right flank pain, scapular pain, or chest pain.19
Since the differential diagnosis for the patient with upper abdominal pain is extensive, point-of-care ultrasound of the gallbladder can reduce the number of diagnoses the clinician must consider.20 Patients with isolated epigastric pain may not routinely get a biliary ultrasound exam, especially if their pain resolves. However, one study showed that one-third of patients with isolated epigastric pain had gallstones, and one-third of the patients with gallstones had cholecystitis.21 Many patients who present to the ED with biliary disease have ongoing pain, and in these patients point-of-care ultrasound can expedite the diagnosis, and focus the clinician’s effort and use of resources.10,22 An algorithmic approach to the patient presenting with suspected biliary colic is outlined in Figure 10-1.
Figure 10-1. Biliary colic algorithm. This flow diagram outlines some of the decision points to consider for patient disposition based on clinical parameters and ultrasound findings. (Courtesy of James Mateer, MD)
Several studies demonstrate that emergency physicians with adequate experience acquire and interpret ultrasound images with skill similar to traditional imaging providers, especially in the detection of gallstones.7,15,23,24 In the hands of emergency physicians, the sensitivity and specificity for detecting gallstones (86–96% and 88–97%, respectively) resembled the pooled sensitivities and specificities in data gathered from imaging specialists (84% and 99%, respectively). On average, emergency providers take 10 minutes to conduct a focused ultrasound examination of the gallbladder. This expedient and accurate information has been shown to effectively decrease ED length of stay and influence provider’s probabilistic judgments especially when diagnosing diseases that are not readily apparent by the clinical presentation.10,25
Providers must use caution, however, when interpreting the findings of gallstones in a patient with atypical symptoms. Cholelithiasis is a prevalent disease and a majority of patients are asymptomatic. Although it may be convenient to attribute a patient’s symptoms to biliary disease, the astute clinician will always remember that biliary colic remains a clinical diagnosis and not a sonographic diagnosis.
ACUTE CHOLECYSTITIS
Classically, the patient presenting with right upper quadrant abdominal pain, fever, and a leukocytosis on laboratory examination raises the concern for a diagnosis of acute cholecystitis. In the ED, however, these findings are not present in a majority of patients. The lack of clinical sensitivity makes the definitive diagnosis of acute cholecystitis dependent on imaging studies (Figure 10-2).26,27
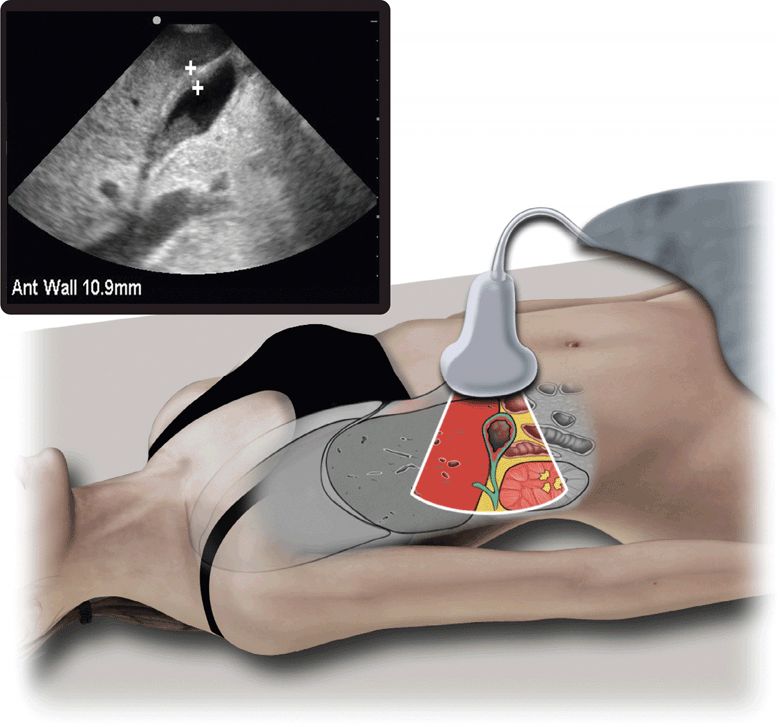
Figure 10-2. Acute cholecystitis. Ultrasound techniques and findings are outlined in the corresponding sections of this chapter.
In general, ultrasound has a 94% sensitivity and 84% specificity for making the diagnosis of cholecystitis.4 One study showed that point-of-care ultrasound performed by emergency physicians had a 91% sensitivity and a 66% specificity for making the diagnosis; however, most of the providers using ultrasound in this study had no structured training. Ninety-five percent to ninety-nine percent of patients with acute cholecystitis have gallstones.28 The sonographic Murphy’s sign (pain elicited by pressing over the fundus of the gallbladder with an ultrasound transducer) may be present in 98.8% of cases, but is not by itself specific for cholecystitis. In a pooled sample of emergency biliary ultrasound studies, the sensitivity of the sonographic Murphy’s sign for cholecystitis was 75% when an emergency physician performed the test but only 45% when performed by the department of radiology.11,24–29 Nevertheless, the sonographic Murphy’s sign helps localize the source of the abdominal pain. When focal tenderness is present, along with an ultrasound study demonstrating gallstones, the patient likely has at least a diagnosis of biliary colic (Figure 10-1). Although no single ultrasound finding predicts cholecystitis with sufficient accuracy for definitive diagnosis, multiple studies have shown that a combination of positive findings increases the accuracy of ultrasound for this diagnosis. One prospective study reported a positive predictive value of 92%, for the combination of gallstones and a sonographic Murphy’s sign, whereas a combination of gallstones and gallbladder wall thickening had a positive predictive value of 95% for the diagnosis of acute cholecystitis.28
In general, the emergency physician can rely on the presence of gallstones and a thickened gallbladder wall in conjunction with the clinical presentation and laboratory findings to identify cases with a high probability of acute cholecystitis. Gallstones are the most common obstruction causing acute cholecystitis, but other causes such as sludge or tumor may be visualized.
JAUNDICE AND BILIARY DUCT DILATATION
When a patient presents to the ED with jaundice, the emergency physician must elucidate the cause as a physical obstruction of the biliary tree or as another disease process. Ultrasound is useful for detecting dilatation of intrahepatic ducts or the common hepatic and bile ducts.30 Once an obstructive process is detected, the next concern is whether the patient is presenting with clinical signs of cholangitis (fever, leukocytosis), which may precipitate the need for urgent ductal decompression (by surgery, ERCP, or transhepatic stenting). Ultrasound is less sensitive at defining the exact etiology of obstruction, which may include a common bile duct stone, pancreatic head tumor, ampullary carcinoma, or bile duct compression from another cancer.31 While ultrasound may detect dilated ducts and the presence of gallstones, other modalities such as CT and ERCP may be needed to determine the ultimate diagnosis and direct treatment.
SEPSIS
Patients who present to the ED with severe sepsis benefit from early goal-directed therapy.32 Identifying and treating the source of sepsis remains a core component that significantly contributes to the success of the protocol. Identifying the source of sepsis is challenging, especially in the elderly population.33 It has been reported that acute cholecystitis and acute cholangitis are responsible for 25% of intra-abdominal sepsis.34 Point-of-care ultrasound may offer prompt and accurate diagnosis in these cases.35
ASCITES
Detection of peritoneal fluid by physical examination is notoriously insensitive. Although the finding of a “fluid wave” has been described and is classically taught, the accuracy of this sign is low. In the emergency and acute care settings, determining whether a patient has ascites may influence initial management and disposition. For example, in a patient with abdominal pain and/or a fever with abdominal ascites, the clinician must consider bacterial peritonitis as a potential cause. Ultrasound can also be used to assess for ascites in patients with an unknown cause of abdominal distention.
HEPATIC ABNORMALITIES
Several hepatic abnormalities have a characteristic ultrasound appearance, such as cirrhosis, metastatic liver disease, liver mass, liver abscess, or hepatomegaly.36
 ANATOMICAL CONSIDERATIONS
ANATOMICAL CONSIDERATIONS
The predominant organ in the right upper quadrant of the abdomen is the liver, bordered superiorly by the diaphragm and coronary/triangular ligament confluence, inferomedially by the duodenum and head of pancreas, and inferiorly by the gallbladder, hepatic flexure of the ascending colon, and superior pole of right kidney. The gastric fundus is located posterolateral to the left hepatic lobe. The liver is divided into right and left lobes by the major lobar fissure, which contains the middle hepatic vein and extends from the gallbladder fossa anteriorly to the inferior vena cava posteriorly. The right lobe is divided into anteromedial and posterolateral segments by the right hepatic vein, and the left lobe is divided into anterior and posterior segments by the left hepatic vein. After draining the liver of venous blood, all hepatic veins converge at the inferior vena cava posteriorly, just inferior to the atriocaval junction. The main portal vein courses from the intestinal venous drainage arcades, through the lesser omentum to the hepatic hilum, where it bifurcates into right and left branches and enters the liver (Figure 10-3A).
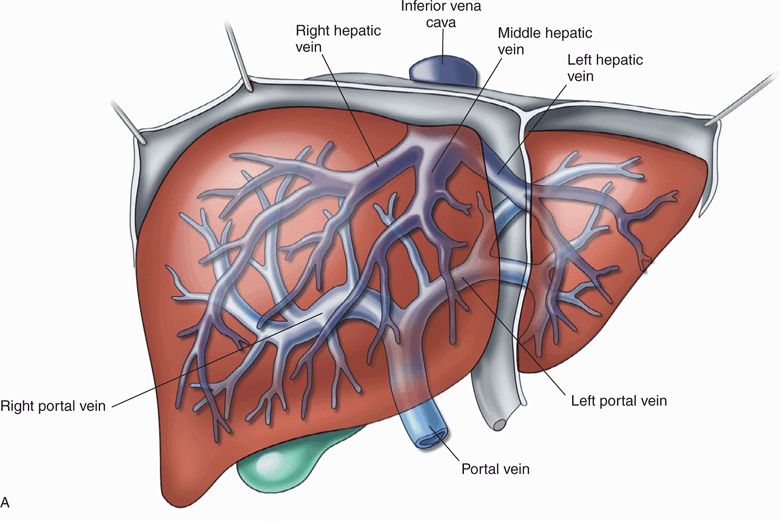
Figure 10-3. (A) Surgical anatomy of the liver. (Redrawn from Feliciano et al. Trauma. 3rd ed. New York, NY: Appleton & Lange/McGraw-Hill, 1996:489.) (B) Normal anatomy. The diagram depicts the relationships in the porta hepatis. The triangle of Calot is bordered by the edge of the liver, the cystic duct, and the hepatic duct. (Redrawn from Schwartz et al. Principles of Surgery. 6th ed. New York, NY: McGraw-Hill, 1994:1368.)
The hepatic artery courses toward the hepatic hilum in the lesser omentum, occupying a position anterior to the main portal vein. At the hilum, the hepatic artery divides into right and left branches and enters the liver parenchyma (Figure 10-3B).
The biliary system begins with the intrahepatic right and left hepatic ducts, which course toward the hilum, uniting to form the extrahepatic common hepatic duct. After exiting the hilum, the common hepatic duct is joined by the cystic duct (from the gallbladder) to form the common bile duct, which courses anterior to the main portal vein, and usually to the right of the hepatic artery in the lesser omentum before entering the duodenum (Figure 10-3B). It is important to remember the anatomical relationships of the hepatic artery, common bile duct, and main portal vein. They traverse the lesser omentum in the region of the hepatic hilum to form the main portal triad. Within the liver, branches of the main portal vein, proper hepatic artery, and biliary tree follow parallel pathways of distribution to the liver parenchyma in bundles known as lesser portal triads. Hepatic venous tributaries do not follow this system.
The gallbladder is divided into the fundus, body, and neck. The body of the gallbladder is contiguous with the inferior surface of the liver and narrows at the neck. The neck often contains spiral valves known as spiral valves of Heister that are occasionally misdiagnosed as impacted stones. The neck is continuous with the cystic duct, which empties into the common hepatic duct to create the common bile duct.
 GETTING STARTED
GETTING STARTED
Patient positioning and respiratory maneuvers play an important role in the hepatobiliary ultrasound examination. The gallbladder is not a fixed organ in the right upper quadrant.
When the patient’s gallbladder lies inferior to the lower rib cage, the patient can be scanned in the recumbent position. The right lower rib cage overlies the gallbladder and may interfere with direct visualization of the gallbladder. The patient may then be asked to take and hold a deep breath. This maneuver shifts the liver and gallbladder inferiorly, so it can be visualized below the costal margin. When the gallbladder cannot be well visualized in the recumbent position, moving the patient to the left lateral decubitus position may significantly improve visualization (Figure 10-4A). In this position, the liver and gallbladder move with gravity toward the patients left, contacting the anterior abdominal wall and providing a better “acoustic window” below the costal margin. Rarely, the patient must roll past the left lateral decubitus position to a nearly prone position in order to allow good visualization of the gallbladder. It may also be helpful to scan patients in the upright position, especially when good images cannot be obtained in the supine or left lateral decubitus positions.
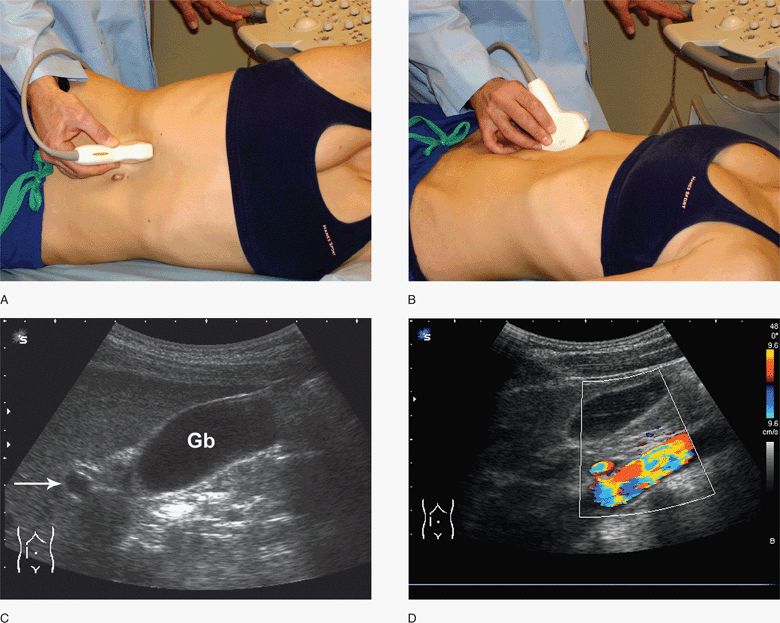
Figure 10-4. Longitudinal views of the gallbladder. Initial transducer position with patient in lateral decubitus (A) and supine positions (B). Gallbladder imaging is often facilitated with a deep inspiratory hold. Transducer is angled cephalad under the rib margins. Corresponding ultrasound image (C) with main portal vein indicated (arrow). Color Doppler may assist in delineating large vascular structures (D). Gb, gallbladder. (Courtesy of James Mateer, MD)
Adjusting the depth, focus point(s), and gain optimizes most sonographic images. Adjust the depth so that the gallbladder fills at least two-third of the screen. Direct the focus point(s) at the structures of interest.37 Do not set the gain too high or low because image quality may be distorted. Tissue harmonic imaging may help identify smaller stones that are typically difficult to visualize.38
 TECHNIQUE AND NORMAL ULTRASOUND FINDINGS
TECHNIQUE AND NORMAL ULTRASOUND FINDINGS
The goal of point-of-care ultrasound is to answer focused questions that facilitate the diagnostic, therapeutic, or procedural workup of the patient. A low- to medium-frequency (2–5 MHz) curvilinear ultrasound transducer will suffice for most ultrasound examinations of the gallbladder. A phased array transducer can be helpful when there is no option but to image between ribs. Less commonly, a linear transducer for a very anterior gallbladder in a thin patient may be required. (See Video 10-1: Hepatobiliary Normal)
Initially, position the transducer sagittally (transducer indicator toward the patient’s head) just inferior to the right costal margin to help locate the gallbladder. Color flow Doppler can be used to confirm that the cystic structure is not a vessel. Since there is great variability in anatomy, transducer position can vary widely from patient to patient. After localizing the gallbladder, orient the transducer to obtain standard images in the long- and short-axis view of the gallbladder.
EVALUATION OF THE GALLBLADDER AND COMMON BILE DUCT
Components necessary to complete the focused evaluation of the gallbladder in cases of suspected biliary colic and acute cholecystitis are as follows:
1. View the gallbladder in two orthogonal planes (long and short axis).
2. Trace the gallbladder from the fundus to the neck, carefully examining for small stones impacted in the neck.
3. Measure the anterior gallbladder wall at its clearest point, which is usually in the mid-portion of the ultrasound image. If focal wall thickening is encountered, make several measurements, one of which includes the focally thickened area.
4. Measure the common bile duct and trace it as far medially as possible.
5. Assess the gallbladder for pericholecystic fluid.
6. Assess for tenderness (sonographic Murphy’s sign) by applying ultrasound-guided pressure directly on the gallbladder.
7. The gallbladder size is less relevant, although it may have clinical implications when it is especially enlarged.
Begin with a sagittal orientation to locate the gallbladder (Figure 10-4B). Place the transducer under the right costal margin at about the mid-clavicular line with the transducer marker directed toward the patient’s head, then sweep the right upper quadrant until an image of the gallbladder is obtained (Figure 10-4C). Ask the patient to take and hold a deep breath. Color and power Doppler aid in distinguishing large vascular structures. The gallbladder should have no Doppler signal and is typically the most anterior cystic structure in the right upper quadrant (Figure 10-4D). Additionally, identify the main portal vein to help identify the gallbladder. Typically, the main portal vein connects to the gallbladder via the main lobar fissure. Locating the main portal vein and following the main lobar fissure to the gallbladder is a good way to locate the gallbladder when it is collapsed or in an odd position.
Obtain a sagittal view of the gallbladder by rotating or sweeping the transducer to align it with the long-axis view of the gallbladder. Examine the gallbladder neck and consider having the patient take and hold a deep breath, to help identify the main portal triad adjacent to the neck of the gallbladder. One of the most difficult skills for the novice operator is the technique of moving between long-axis views and short-axis views. To change planes, move the transducer slowly and keep some element of the gallbladder in view. This is the time to adjust the patient’s position or perform respiratory maneuvers if the gallbladder is not well visualized. Obtain short-axis views after long-axis views, by rotating the transducer about 90° counterclockwise, with the transducer marker toward the patients right (Figure 10-5). Visualizing the gallbladder from multiple views helps to differentiate normal anatomy and artifacts from abnormal findings. If imaging remains difficult after patient positioning and deep inspiratory efforts, consider imaging the gallbladder from intercostal views (Figure 10-6). Intercostal views may be obtained with the patient in the supine or lateral decubitus position. These are helpful when the gallbladder is positioned under the ribs and/or the patient is unable to take a deep breath. Many emergency providers like using intercostal views because the position of the transducer is similar to that used when visualizing Morison’s pouch during the FAST exam. A phased array transducer with a narrow “footprint” may be particularly helpful for intercostal imaging.
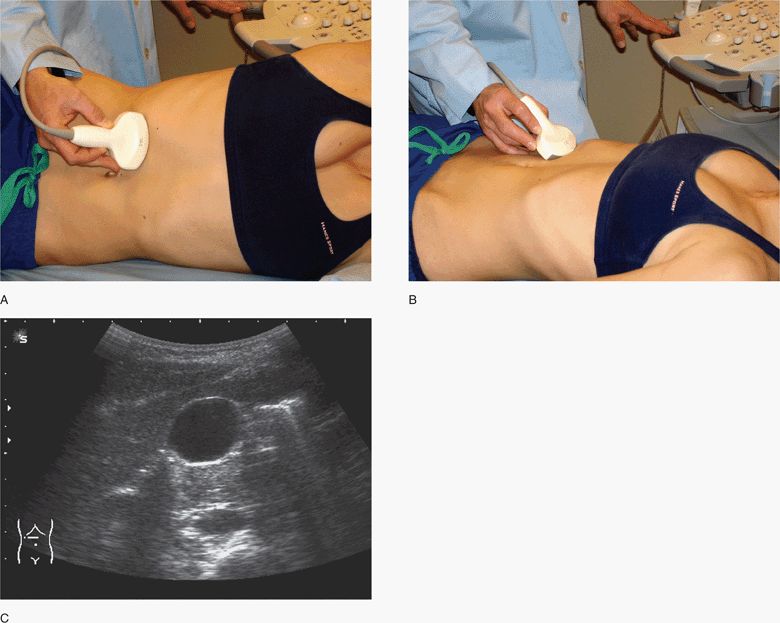
Figure 10-5. Transverse views of the gallbladder. Initial transducer position with patient in lateral decubitus (A) and supine positions (B). Note the deep inspiration used and cephalad angulation of the transducer to view under rib margins. Corresponding ultrasound image (C). Shadowing is from adjacent bowel gas outside the gallbladder. (Courtesy of James Mateer, MD)
Figure 10-6. Intercostal views of the gallbladder. Initial transducer position with patient in lateral decubitus (A). Initial imaging plane is aligned parallel to the ribs. Corresponding ultrasound image (B). A small segment of the portal vein is seen below the neck of the gallbladder. (Courtesy of James Mateer, MD)
It is not clear how much training is required to gain competency in emergency gallbladder ultrasound. One report suggests that novice operators who perform and interpret at least 25 gallbladder ultrasound exams demonstrate excellent proficiency in detecting gallstones.39
Gallbladder ultrasound images should be examined and assessed for the presence of gallstones, for the determination of wall thickness, and for the presence of pericholecystic fluid. An accurate measurement of wall thickness is made on the anterior wall that is perpendicular to the imaging plane (>3 mm is considered abnormally thick). If gallstones are detected, change the patient’s position (roll to the left lateral decubitus or prone position) to document that they are mobile.
Visualization of the portal vein in the sagittal plane aids in identifying the main portal triad (Figure 10-7A). The portal vein will have bright echogenic walls compared with the hepatic veins. It can usually be visualized coursing toward the porta hepatis. The main portal triad is made up of the main portal vein, hepatic artery, and the common bile duct. By rotating the transducer 90° (counterclockwise) from a sagittal orientation, a transverse image of the portal vein with the associated common bile duct (anterior/lateral) and hepatic artery (anterior/medial) may be visualized (Figure 10-7B). This is referred to as the “Mickey Mouse sign.” Use color or power Doppler to identify vascular structures. The portal vein and hepatic artery will demonstrate color Doppler signals while the common bile duct will not (Figure 10-7C,D). Measure the common bile duct at the level of the porta hepatis from inner wall to inner wall, which is normally <6–7 mm.40–42,43 (C) Tissue harmonic imaging may help delineate the common bile duct. However, tissue harmonics increase the apparent thickness of walls and must be used with caution. Common bile duct dilatation is an indirect indication of obstruction. The site of common bile duct obstruction from stones is often near its termination close to the pancreatic head and is difficult to visualize in most patients (Figure 10-8).
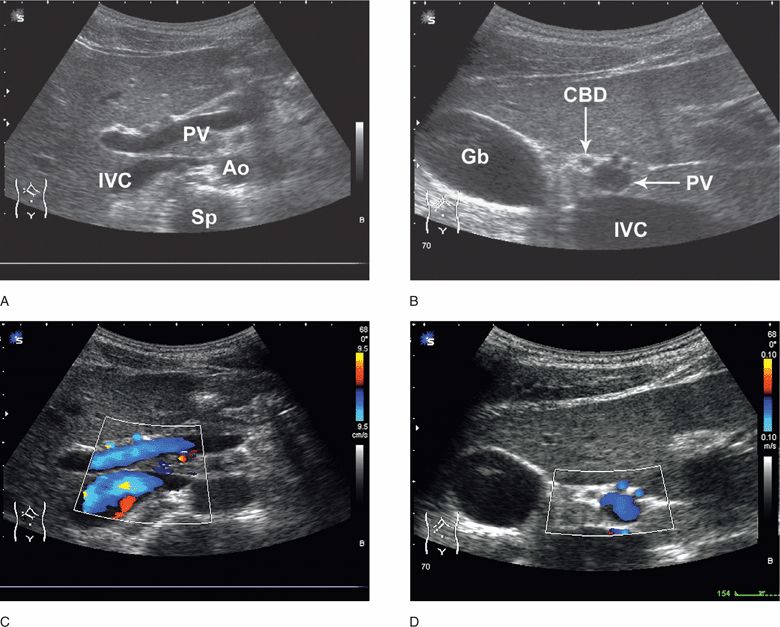
Figure 10-7. Portal vein and normal common bile duct. Longitudinal view of the portal vein (A). Transverse view of the portal vein (B). Corresponding color Doppler images (C,D). Patient has a duplicated hepatic artery. IVC = inferior vena cava, PV = portal vein, Ao = aorta, Sp = spine, Gb = gallbladder, CBD = common bile duct. (Courtesy of James Mateer, MD)
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


 CLINICAL CONSIDERATIONS
CLINICAL CONSIDERATIONS CLINICAL INDICATIONS
CLINICAL INDICATIONS ANATOMICAL CONSIDERATIONS
ANATOMICAL CONSIDERATIONS GETTING STARTED
GETTING STARTED TECHNIQUE AND NORMAL ULTRASOUND FINDINGS
TECHNIQUE AND NORMAL ULTRASOUND FINDINGS COMMON AND EMERGENT ABNORMALITIES
COMMON AND EMERGENT ABNORMALITIES COMMON VARIANTS AND SELECTED ABNORMALITIES
COMMON VARIANTS AND SELECTED ABNORMALITIES PITFALLS
PITFALLS CASE STUDIES
CASE STUDIES