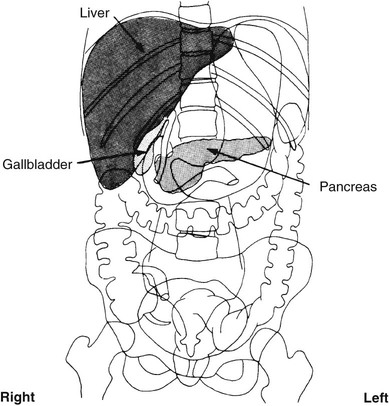
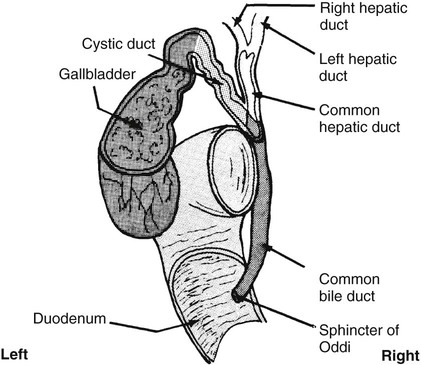
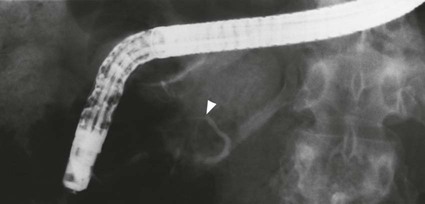
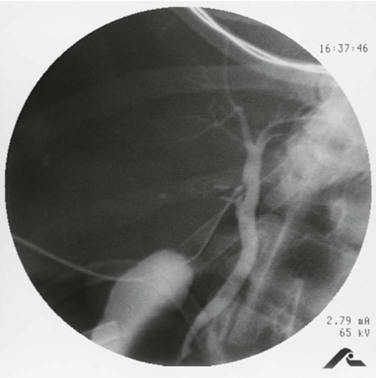
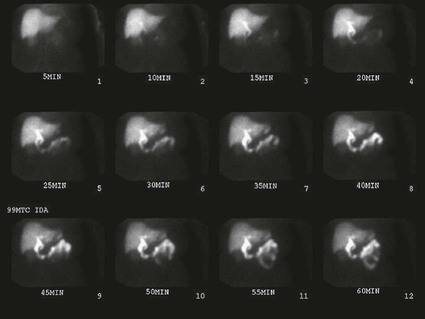
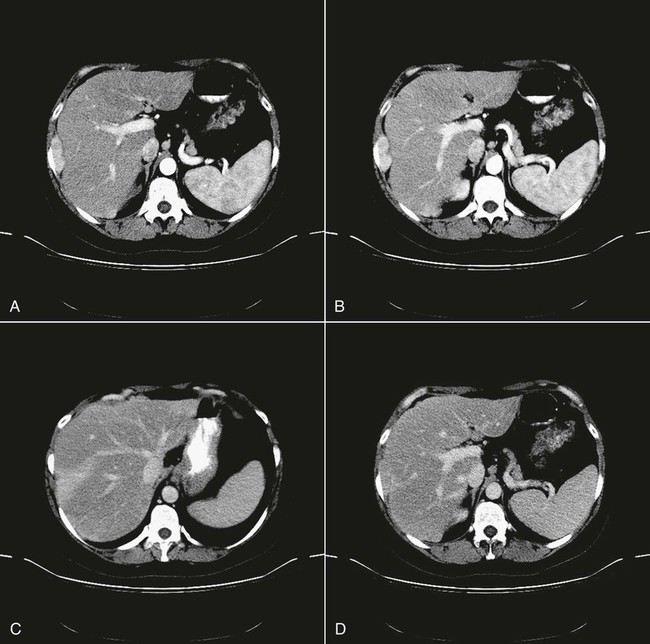
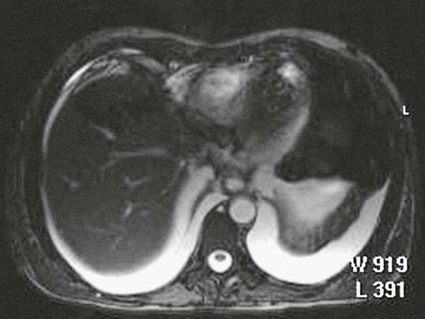
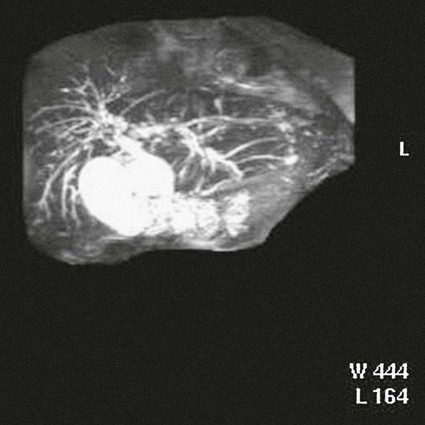
On completion of Chapter 6, the reader should be able to do the following: • Describe the anatomic components of the hepatobiliary system and state how they are visualized radiographically. • Discuss the role of other imaging modalities in imaging of the hepatobiliary system, particularly sonography, magnetic resonance imaging, and computed tomography. • Characterize a given condition as inflammatory or neoplastic. • Identify the pathogenesis of the pathologies cited and the typical treatments for them. • Describe, in general, the radiographic appearance of each of the given pathologies. The hepatobiliary system is composed of the liver, gallbladder, and biliary tree (Fig. 6-1). The pancreas is closely related and shares a portion of the biliary ductal system, hence its inclusion here. A system of ducts acts to drain bile produced in the liver into the duodenum (Fig. 6-2). Bile from the liver’s two main lobes is drained by the right and left hepatic ducts. These unite to form the common hepatic duct, which is joined usually in its midportion by the cystic duct from the gallbladder. Together, the cystic duct and the common hepatic duct form the common bile duct. Percutaneous transhepatic cholangiography (PTC) is used to visualize the biliary tree and involves insertion of a needle into the biliary tree by puncture directly through the wall of the abdomen. With the use of a flexible, 22-gauge, skinny needle (Chiba), this procedure is safe and fairly easy to perform. The subsequent injection of iodinated contrast medium (Fig. 6-3) is useful in distinguishing medical jaundice, caused by hepatocellular dysfunction, from surgical jaundice, which results from biliary obstruction. Also, the examination is useful for detecting the presence of calculi or a tumor in the distal common bile duct. It has a high success rate in imaging the biliary ductal system, is less expensive than an endoscopic retrograde cholangiopancreatogram, and has a low complication rate of approximately 3.5%. It also may be immediately followed by a therapeutic procedure such as a biliary drainage, stone removal or crushing via contact lithotripsy or laser fragmentation, stent placement, or biopsy. This procedure is preferred in the evaluation of proximal obstructions involving the hepatic duct bifurcation, which is difficult to image with the retrograde approach via an endoscopic retrograde cholangiopancreatogram (see next section). The endoscopic retrograde cholangiopancreatogram (ERCP), an imaging procedure performed by a gastroenterologist, is a means of visualizing the biliary system and main pancreatic duct, which provides drainage for the pancreatic enzymes into both the digestive tract and the common bile duct. A fiberoptic endoscope is passed through the duodenal C-loop to visualize the hepatopancreatic ampulla (ampulla of Vater). A thin catheter is then directed into the orifice of the common bile duct or pancreatic duct, followed by an injection of contrast medium (Fig. 6-4). In many cases, the ERCP is preferred over the PTC and is often preceded with a sonographic examination or computed tomography (CT) investigation of the pancreas. Although an ERCP is more expensive than PTC, it is often used to visualize nondilated ducts, distal obstructions, bleeding disorders, and the pancreas. The complication rate (2% to 3%) is similar to that of PTC and also offers the ability to perform therapeutic procedures such as sphincterotomy, stone extractions, stent placement, and biliary dilatation. Cytology and biopsy may also be performed. Operative cholangiography is performed during surgery at the time of a cholecystectomy to detect biliary calculi and the need for common bile duct exploration (Fig. 6-5). A needle is placed directly into the cystic duct or common bile duct by the surgeon, and a small volume (6 milliliters [mL]) of iodinated contrast material is injected, followed by radiography. A second injection of 5 mL is made, followed by radiography a second time. The resulting images are reviewed for possible areas of concern before the surgery is completed. It is imperative that no air bubbles be injected into the ductal system with the contrast agent during this procedure because they can mimic stones. Real-time diagnostic medical sonography is now the modality of choice for evaluating the gallbladder (Fig. 6-6) and biliary tree. This procedure is noninvasive, and the gallbladder can be imaged in almost all fasting patients regardless of the body habitus or clinical condition of the patient. When sonography is performed by a skilled sonographer, it has been proven to be almost 100% accurate in detecting gallstones, which are demonstrated as echogenic areas within the echo-free gallbladder. Thickening of the gallbladder wall is also easily identified. Sonography is also an excellent tool for determining the presence of common bile duct obstruction, evaluation of the intrahepatic biliary ductal system, and identification of abscesses. The liver may be evaluated by sonography because of its ideal location in the RUQ and broad contact with the abdominal wall. Hepatic lesions of 1 cm or greater are easily identified, with cystic lesions appearing echo-free and solid masses appearing echogenic, allowing excellent guidance for aspiration and biopsy of these lesions. The role of CT in the hepatobiliary system is similar to its role in the GI tract. It is the accepted modality for following malignancies and assessing masses, particularly of the gallbladder, liver, and pancreas. It is also helpful in evaluating complications of cholecystitis such as perforations and abscess formations. The use of spiral or helical CT ensures that the entire liver is imaged in one breath, eliminating respiratory artifacts and in many cases demonstrating the liver parenchyma and associated structures better than sonography. In addition to the excellent contrast resolution offered by CT, the use of large-bolus intravenous (IV) iodinated contrast media injections during dynamic CT examination has also improved evaluations of the hepatobiliary ductal system and blood flow via three-phase imaging of the liver to capture the arterial and portal venous blood flow (Fig. 6-7). If a biliary obstruction is not visible on sonographic examination, CT is generally used to identify the location and extent of the obstruction because it is not limited by patient size or the presence of bowel gas. Lacerations of the liver and resultant abdominal bleeding are readily detected on CT (Fig. 6-8), as are metastatic lesions within the liver. CT also demonstrates good visualization of pancreatic tumors and pseudocysts. In addition, CT-guided biopsy procedures for the liver (Fig. 6-9), pancreas, and kidney allow for analysis and drainage and offer significant advantages over conventional surgical biopsy and drainage. Cholescintigraphy performed in nuclear medicine is very useful to confirm cholecystitis and for distinguishing acute cholecystitis from chronic cholecystitis (Fig. 6-10). Radioactive technetium is cleared from blood plasma into bile, demonstrating the physiologic function of the liver, excretion into the biliary ductal system, and visualization of the gallbladder about 1 hour after injection. Delayed visualization or nonvisualization of the gallbladder indicates pathology. In addition, it is a noninvasive method of evaluating biliary drainage, hepatobiliary leaks following trauma or surgery, and segmental obstruction. The role of magnetic resonance imaging (MRI) of the hepatobiliary system has improved greatly as a result of shorter scan times, which allow the acquisition of several images of the abdomen in a single breath. MRI is often used in conjunction with CT to evaluate pathologies and anomalies of the peritoneum, especially the liver and pancreas. MRI may also be used to identify retroperitoneal bleeds following trauma (Fig. 6-11). Contrast-enhanced three-dimensional dynamic scans of the liver imaged at timed intervals help to differentiate certain tumors from hemangiomas. Magnetic resonance cholangiopancreatography (MRCP) is an imaging procedure that uses magnetic resonance to visualize the gallbladder and biliary system. MRCP is noninvasive and does not require the use of a contrast agent (Fig. 6-12). A heavily T2-weighted sequence is used to suppress the tissues around the biliary system, allowing the gallbladder and bile ducts to appear bright and enabling visualization of stones or other obstructions. MRCP usually accompanies other imaging sequences of the liver, but it takes only about 15 seconds to acquire an image. Alcohol is a known toxin, which, when metabolized by the liver, causes cellular damage; alcohol abuse has long been associated with liver disease. Approximately two million Americans have alcohol-induced liver disease, ranging from alcoholic fatty liver to alcoholic cirrhosis of the liver. Alcohol cannot be stored in the human body, and therefore, the liver must convert it, through oxidation, to alcohol dehydrogenase, acetaldehyde, and acetate, all of which reduce cellular function. This leads to interference with carbohydrate and lipid metabolism. Oxidation also results in reduced gluconeogenesis and increased fatty acid synthesis associated with alcohol metabolism. Chronic alcohol abuse often leads to fatty liver, followed by hepatitis, cirrhosis, hepatocellular carcinoma, or all of these diseases. Fatty liver is the most frequent early response to alcohol abuse. Changes in liver function result in a buildup of lipids such as triglycerides, which are deposited in the liver cells. This condition is usually asymptomatic; however, patients may have hepatomegaly. Fatty infiltration may be demonstrated by using CT or sonography, but CT is currently the examination of choice. CT demonstrates the fatty deposits as hypodense areas throughout the liver (Fig. 6-13). Inflammation often follows fatty changes within the liver, leading to alcoholic hepatitis
Hepatobiliary System
Anatomy and Physiology
Biliary Tree
Imaging Considerations
Radiography
Contrast Studies
Percutaneous Transhepatic Cholangiography.
Endoscopic Retrograde Cholangiopancreatogram.
Operative Cholangiography.
Diagnostic Medical Sonography
Computed Tomography

Nuclear Medicine Procedures
Magnetic Resonance Imaging
Inflammatory Diseases
Alcohol-Induced Liver Disease
![]()
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


Radiology Key
Fastest Radiology Insight Engine