20
Hepatobiliary Tumors
Eugene C. Lin and Abass Alavi
The primary value of positron emission tomography (PET) is in detection of extrahepatic disease and monitoring treatment.
- Primary tumor detection
- PET has limited sensitivity for well-differentiated hepatocellular carcinoma (HCC) (Fig. 20.1).
- PET has no role in screening for HCC in patients with cirrhosis.3
- Extrahepatic disease
- The primary tumor must have fluorode-oxyglucose (FDG) uptake for PET results to be valid.
- PET can detect distant disease for staging and recurrence, altering management in up to 30% of patients.4
- PET may be valuable in patients with treated HCC and a rising serum α-feto-protein and normal conventional imag ing. In these cases, the accuracy of PET for detecting recurrence is 74%.5
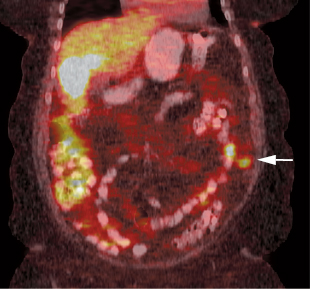
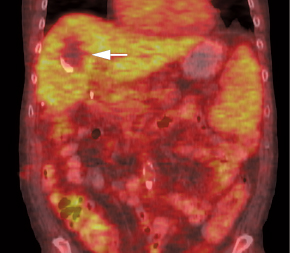
- Monitoring therapy. PET is more accurate than computed tomography (CT) (after iodized oil injection) for evaluating tumor viability postchemoembolization (Fig. 20.2).6 PET may also detect recurrence after radio- frequency ablation earlier than CT.7
- Prognosis
- A standardized uptake value (SUV) ratio (tumor to nontumor SUV) > 2 predicts poor prognosis after resection.8
- Tumor recurrence is more likely after liver transplantation in patients with PET-positive HCC.9
- Primary lesion detection
- PET. Sensitivity 50 to 70%10,11
- Low sensitivity is due to low uptake in well-differentiated HCC.
- Tumors that are visualized by PET (Fig. 20.1) usually are higher grade and larger in size, with elevated circulating α-fetoprotein.
- PET is less sensitive than CT, magnetic resonance imaging (MRI), or ultrasound.
- Extrahepatic disease.12 PET has a relatively high detection rate (83%) for extrahepatic metastases > 1 cm in size but a low detection rate for metastases < 1 cm.
- PET can detect lesions that are negative or equivocal on conventional imaging.
- Patients with rising tumor markers and negative PET exams usually do not have extrahepatic metastases; however, HCCs are often detected in the liver within months. Thus, these patients should be closely followed with liver imaging.
Fig. 20.1 Hepatocellular carcinoma: high-grade versus low grade. (A) Axial T2-weighted magnetic resonance imaging scan demonstrates a focal area of hyperintensity corresponding to a hepatoma (arrow) in the right dome of the liver. (B) Axial positron emission tomography (PET) scan demonstrates increased uptake in this high-grade hepatoma. (C) Axial computed tomography (CT) in a different patient demonstrates a mostly isodense right lobe lesion with an enhancing capsule and a peripheral area of low density (arrow). (D) Axial PET/CT at the same level demonstrates that this low-grade hepatoma has uptake equal to normal liver.
Fig. 20.2 Hepatic chemoembolization. Coronal positron emission tomography/computed tomography scan demonstrates lack of fluorodeoxyglucose uptake in hepatoma (arrow) after chemoembolization.
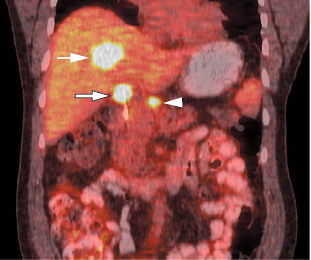
Fig. 20.3 Metastatic cholangiocarcinoma. Coronal positron emission tomography/computed tomography scan demonstrates both intrahepatic (arrow) and extrahepatic (open arrow) cholangiocarcinoma and a local nodal metastasis (arrowhead).
- SUV. HCCs usually have lower SUVs than metastases or cholangiocarcinoma.13
- Fibrolamellar HCC. Fibrolamellar HCCs, which are pathologically low grade, can have increased FDG uptake (these tumors have intratumoral fibrous stromata, which are associated with increased FDG uptake).4
- Delayed imaging. Delayed imaging at 2 or 3 hours may detect more lesions.14
- Cirrhosis/hepatitis. Patients with cirrhosis and chronic hepatitis can have slightly increased FDG activity in the liver, which could limit detection of HCC.
PET can detect the primary tumor, regional lymph nodes (Fig. 20.3), and distant disease (Fig. 20.4). The primary value is in detecting distant disease. In patients with cholangio-carcinoma and gallbladder carcinoma, PET/CT findings change management in 17% of patients deemed resectable after initial work-up.15
 Hepatocellular Carcinoma1,2
Hepatocellular Carcinoma1,2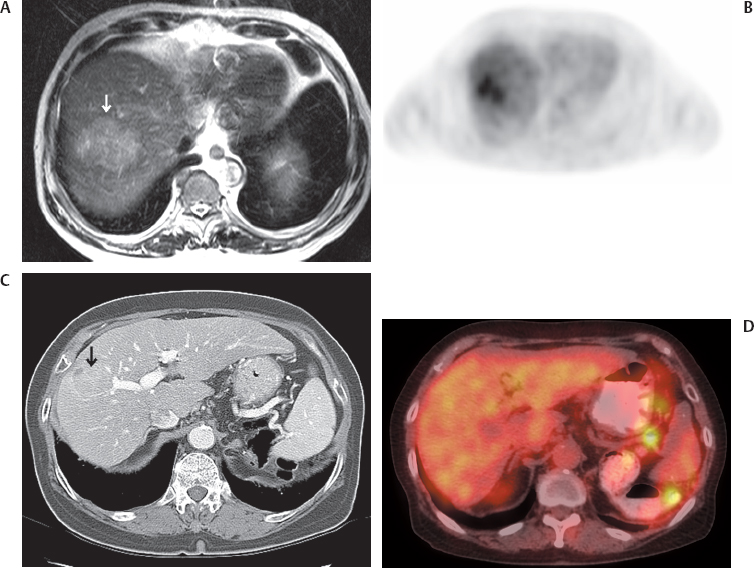
 Cholangiocarcinoma1
Cholangiocarcinoma1