and Siddharth P. Jadhav2
(1)
Department of Radiology, University of Texas Medical Branch Pediatric Radiology, Galveston, TX, USA
(2)
The Edward B. Singleton Department of Pediatric Radiology, Texas Children’s Hospital, Houston, TX, USA
Abstract
This chapter deals with injuries of the hip and femur. Various types of fractures and other injuries are presented. MR is discussed where it significantly adds to evaluation of these injuries.
Normal Fat Pads and Joint Space
The two views generally obtained for evaluating the hip are the anteroposterior and frog-leg views. The fat pads surrounding the hip and the joint space are best assessed on the straight anteroposterior view and include the iliopsoas, gluteus, and obturator internus fat pads (Fig. 9.1). These fat pads do not lie against the joint capsule directly and thus are not displaced outwardly if fluid accumulates within the joint but can be moved outwardly and obliterated secondary to edema around the hip joint (Fig. 9.2a).

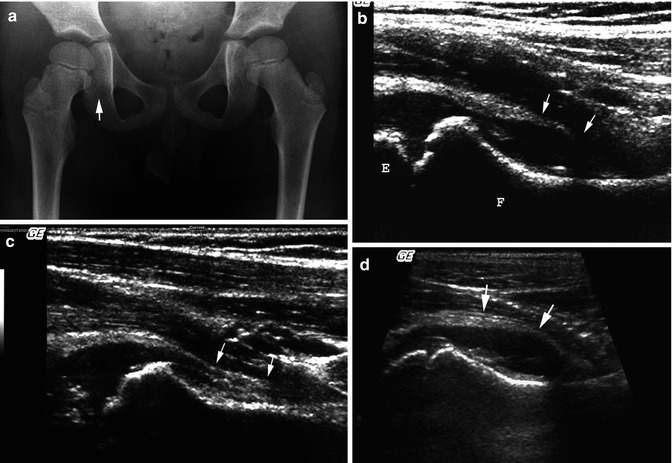

Fig. 9.1
Normal fat pads around the hip. Note the iliopsoas (1), gluteus (2), and obturator internus (3) fat pads
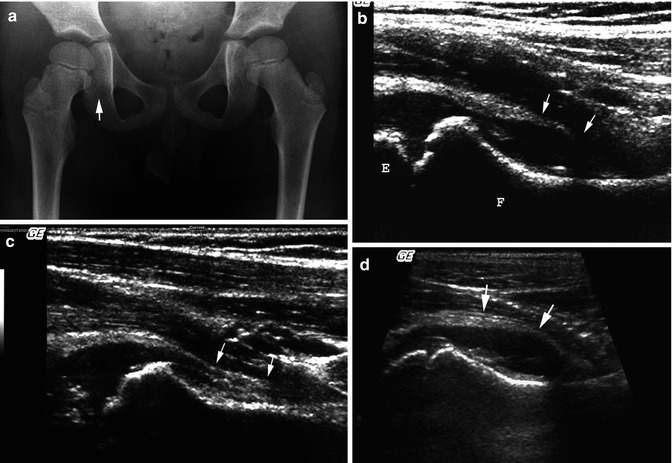
Fig. 9.2
Transient synovitis. (a) On this AP view of the pelvis, note joint space widening (arrow) involving the right hip. (b) Ultrasound demonstrates relatively clear fluid accumulating between the capsule (arrows) and the underlying echogenic cortex of the femoral neck (F). Epiphysis (E). (c) Normal side for comparison. Note the position of the joint capsule (arrows) and that there is no joint fluid present. (d) Transient synovitis with some debris. Note fluid under the slightly thickened joint capsule (arrows) which in this case is a little thickened. The fluid also contains a little debris
Detecting Fluid in the Hip Joint
When fluid (blood, pus, serous fluid) accumulates in the hip joint, the femoral head is displaced laterally in infants and young children because this is the venue of least resistance. At the same time it causes the joint space to become widened (Fig. 9.2a), but this is less commonly seen in older children because the ligaments and muscles are stronger and resist displacement. Detecting fluid in the hip joint is now best accomplished with ultrasonography [1] where with imaging in the sagittal plane one easily can detect joint fluid, the commonest cause of which is transient synovitis (Fig. 9.2b, c). In some cases some degree of synovial thickening may be seen. In addition, in some cases a little joint fluid debris may be present (Fig. 9.2d), but usually it is clear. With pus, as part of septic arthritis, the joint fluid is dirty, the synovium thickened, and the overlaying iliopsoas muscle thick and edematous (Fig. 9.3).
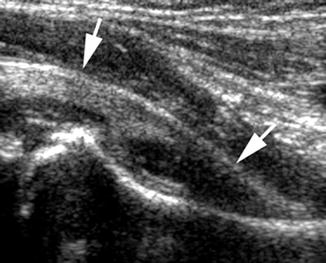
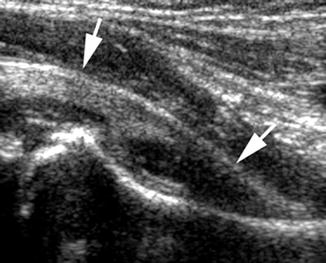
Fig. 9.3
Septic arthritis: ultrasound. Note thickening of the synovium and capsule (arrows), joint fluid with some speckled debris, and thickening of the overlying muscle
Injuries of the Upper Femur
Fractures through the femoral neck and intertrochanteric region of the femur are distinctly less common in children than in adults, but they do occur (Fig. 9.4). These usually result from axial loading on the femur and hip. Very often these fractures are first considered to be the result of child abuse, but this type of fracture is very uncommon with child abuse (see Chap. 12). Salter–Harris epiphyseal–metaphyseal fractures on the other hand are more common and most often are Salter–Harris type I or II injuries [2]. In assessing the upper femur for the presence of these fractures, one first should look for an increase in the width and radiolucency of the involved epiphyseal plate and then for widening of the medial joint space (Fig. 9.5). The first finding indicates the presence of an epiphyseal–metaphyseal separation and the second the presence of associated joint fluid/blood. With Salter–Harris type II fractures, a metaphyseal corner fracture is seen.

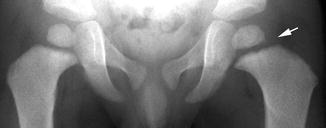

Fig. 9.4
Fractures; proximal femur. (a) Note the transverse impacted intertrochanteric fracture (arrow). (b) Older child with an intertrochanteric fracture (arrow)
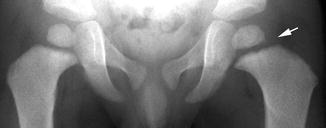
Fig. 9.5
Salter–Harris I fracture. Note widening of the epiphyseal plate on the left (arrow) characteristic of a nondisplaced Salter–Harris I fracture
Anterior or posterior dislocation of the hip is not particularly common in childhood [3]. The reason for this is that the epiphysis is still open and as such represents the weakest point of the femoral head/neck complex. Therefore, Salter–Harris type I and II injuries are more likely to occur. Of course, in the older child, with epiphyseal closure a dislocation is more likely and, as in adults, posterior dislocations are more common. Acetabular rim fractures can be associated injuries, but in childhood the fracture more often is one which involves the triradiated cartilage. Avulsion injuries of the lesser and greater trochanters are not particularly common, but with the apophysis of the lesser trochanter, the findings can be chronic as part of the problem of spasticity and contractures in cerebral palsy. Unlike adults, avulsion of the lesser trochanter in a skeletally immature child should not raise suspicion of underlying metastatic malignancy.
Legg–Perthes Disease
Legg–Perthes disease or aseptic necrosis of the femoral capital epiphysis is common, but its etiology is not known. It generally is held that as many as 10 % of patients who present with symptoms initially suggesting transient synovitis actually turn out to have early Legg–Perthes disease [4]. In my experience, however, confusing the two entities is not that common, but follow-up is necessary if symptoms do not resolve and the initial diagnosis is transient synovitis.
Early on in Legg–Perthes disease, increased density and smallness of the involved femoral head occur (Fig. 9.6a). These are the earliest findings in Legg–Perthes disease, and although subchondral fractures (Fig. 9.6b) also occur relatively early, they are not nearly as common [5]. Other findings include lateral displacement of the femoral head with widening of the medial joint space and atrophy of the surrounding muscles [5]. Lateral displacement of the femur results in less pressure on the medial acetabular wall and development of the so-called teardrop sign [6] (Fig. 9.6a). However, positioning is crucial and must be near perfect to avoid misinterpretation of this finding which may appear to be present if the pelvis is rotated. Eventually the femoral head becomes more sclerotic and fragmented and finally is resorbed (Fig. 9.6c). If the femoral head is kept within the acetabulum during the healing phase, it will heal in a normal rounded fashion. However, if the femoral head remains dislocated, one will end up with the typical coxa vara, coxa magna, and coxa plana deformity (Fig. 9.6d). In addition to the foregoing findings, in many cases associated irregularities of the metaphyses [7] occur (Fig. 9.6c). These changes are secondary to reactive fibrous tissue. Generally, they are considered a poor prognostic sign.


Fig. 9.6
Legg–Perthes disease. (a) Early changes consist of smallness and increased density of the involved femoral capital epiphysis (arrow). The joint space also is widened and a tear drop sign is present. (b) Subchondral fracture (arrow). (c) More advanced changes. The femoral capital epiphysis is fragmented and partially resorbed (arrow). There is widening of the joint space and persistent subluxation of the hip. Also note lucent areas in the metaphysis. (d) Healing phase: poor outcome. Because the femoral head was not constantly located within the acetabular roof with subsequent healing, one ends up with the typical coxa magna, vara, and plana deformity
Finally, if plain film findings are equivocal, or normal, and one still suspects Legg–Perthes disease, one can turn to nuclear scintigraphy or MR imaging [8, 9]. There are those who believe that MR imaging is more sensitive, but nuclear scintigraphy is less expensive. With nuclear scintigraphy, one looks for photon deficiency of the femoral head, usually laterally, while with MR imaging, there is loss of the normal high signal of fatty marrow on T1-weighted images.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree