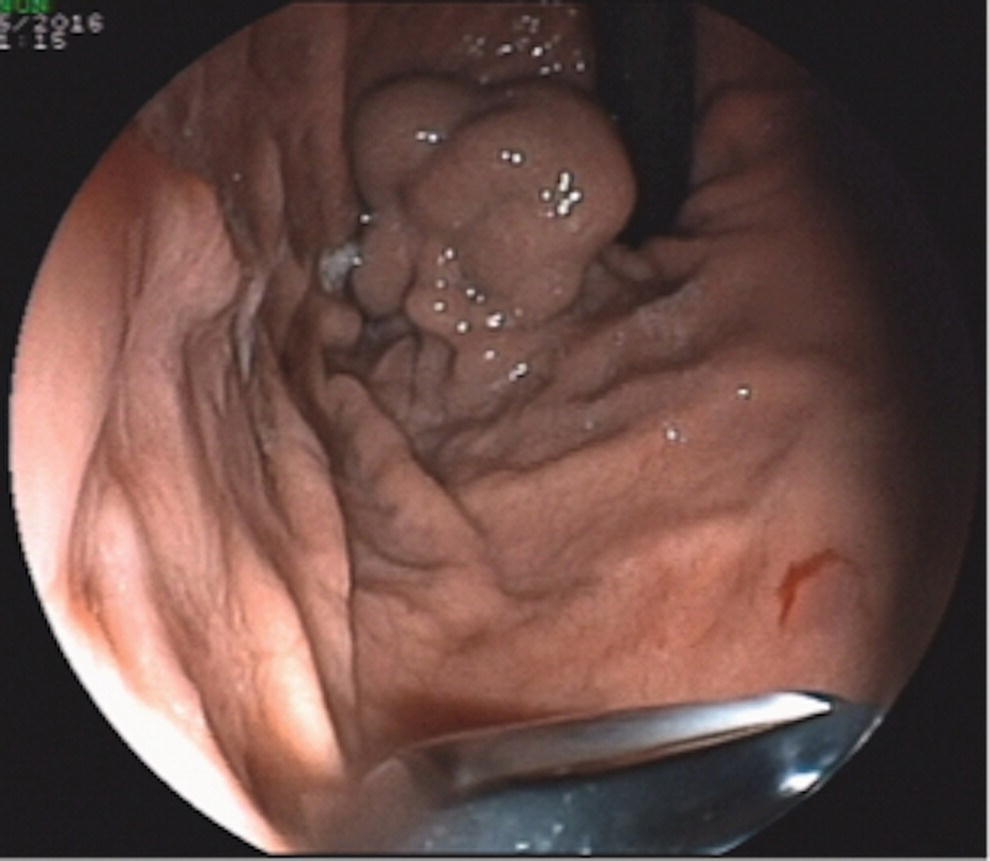
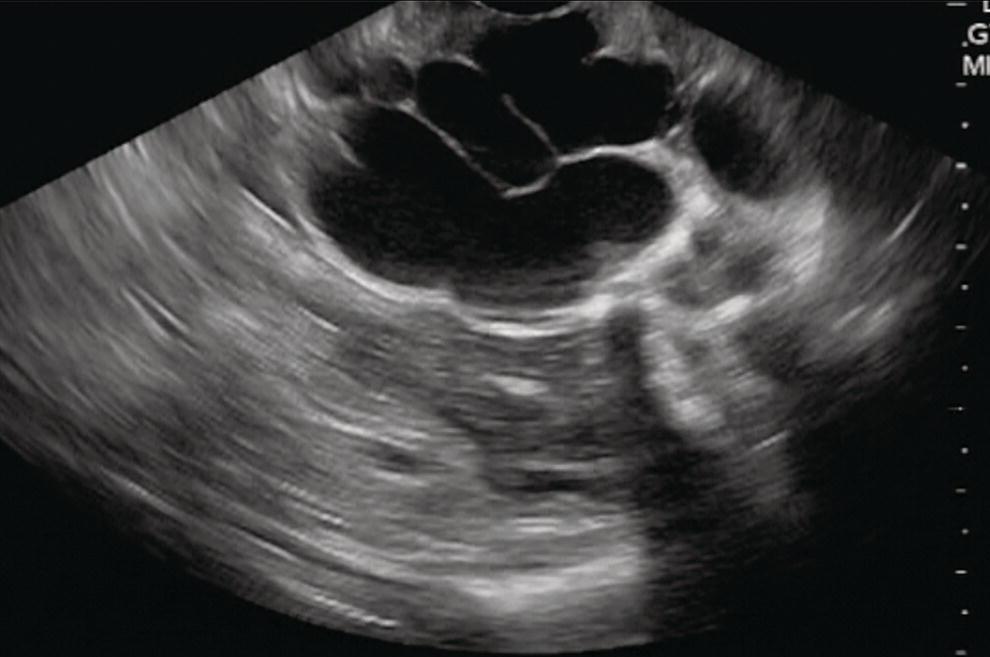
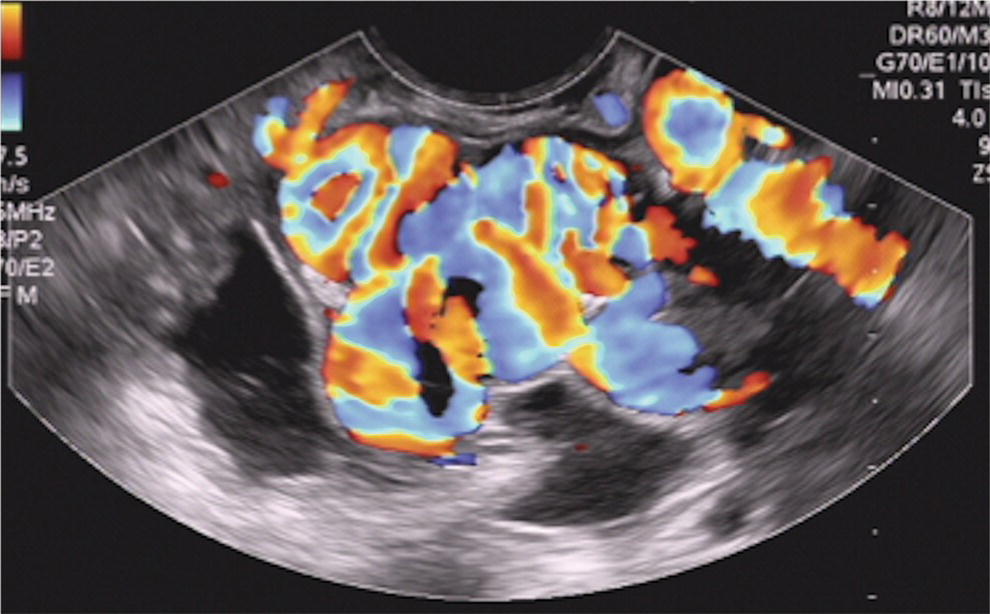
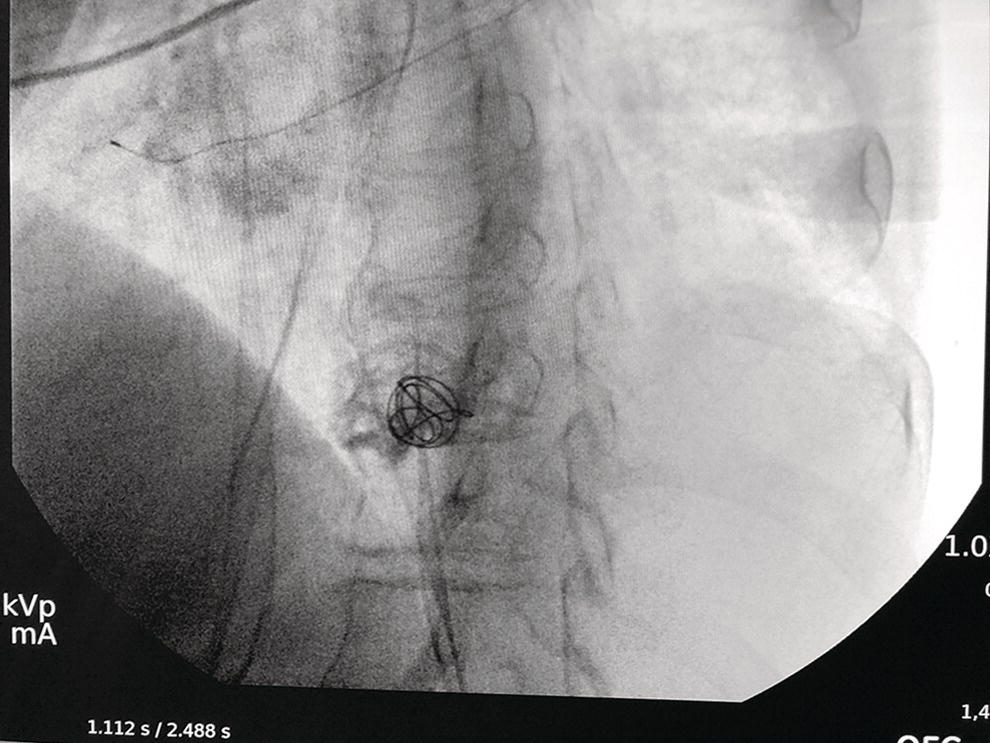
Dalton Marques Chaves and Filipe Tomishige Chaves Gastrointestinal Endoscopy Unit, University of Sao Paulo, Sao Paulo-Brazil Since the initial description of the N‐butyl‐2‐cyanoacrylate injection by Sohendra in 1986 for treatment of bleeding gastric varices, it is still considered the standard treatment for this type of varix, despite the significant incidence of adverse events. More recently, endoscopic ultrasound (EUS)‐guided treatment using cyanoacrylate or coil has showed itself a secure and efficient method, with the advantage of allowing the precise injection of cyanoacrylate into the vessel lumen, even in cases with blood in the gastric lumen. Furthermore, it is also possible to confirm varix obliteration and evaluate recurrences with the Doppler system. In 2007, Romero‐Castro et al. described for the first time the echoguided treatment of gastric varices by injection of cyanoacrylate directly into the varix, with 100% eradication efficiency. However, this method did not decrease the risk of embolism when compared with the normal endoscopic technique, with an incidence of up to 50%. Because of the risk of embolism with cyanoacrylate, the treatment of gastric varices with coil has become an interesting option. These coils, already in use for endovascular therapy, are composed of synthetic fibers connected to a metallic wire that, when released into the bloodstream, may lead to thrombosis. The size of coil to be employed is selected according to the varix diameter. In 2010, Romero‐Castro et al. described for the first time the use of coil in the treatment of gastric varices, treating four patients with success. However, due to the high number of coils necessary for the treatment, cost has been a limitation. In 2011, Binmoeller et al. reported on the successful use of the echoguided technique combining coil and cyanoacrylate. The goal of this combination is to cause the synthetic fiber coils to retain the glue, lowering the risk of embolism and reducing the necessary volume of cyanoacrylate and number of coils. In a prospective randomized study, we compared echoguided treatment (coil plus cyanoacrylate) and conventional cyanoacrylate technique. The volume of cyanoacrylate used in the combined technique was lower (1.4 vs. 3.0 ml), as was the incidence of pulmonary embolism diagnosed by chest computed tomography (25% vs. 50%). A systematic review by McCarty et al. in 2019 that analyzed the three types of echoguided treatment (isolated cyanoacrylate, isolated coil, and coil plus cyanoacrylate combination) suggests that combined treatment is the best option. The steps involved in performing echoguided treatment using coil and cyanoacrylate are as follows. Figure 42.1 Endoscopic imaging of gastric varix. Figure 42.2 Gastric varix seen by endoscopic ultrasonography. Figure 42.3 Gastric varix seen with color Doppler. Figure 42.4 Needle inside the varix. The combined echoguided treatment (coil plus cyanoacrylate) for gastric varices has been shown to be efficient and safe, with technical and clinical success rates of 96–100%. The incidence of side effects varies between 0 and 25%. Pulmonary embolism is the main complication, despite most cases being asymptomatic. In 2016, Baht et al. described a case of symptomatic pulmonary embolism among 152 treated patients. In our study in 2019, when performing chest CT on all treated patients, the incidence of pulmonary embolism caused by Histoacryl was 25%, with all of them being asymptomatic. Most patients have received only one coil and one Histoacryl ampoule (0.5 ml). The success rate after only one treatment session was 73.4% of treated cases. Treatment was repeated if necessary only after 30 days, which is sufficient time for the thrombosis to consolidate. Abdominal pain has also been reported in up to 25% of cases, fever in up to 3%, and minor delayed upper gastrointestinal bleeding from coil/glue extrusion in 3%. Figure 42.5 Obliterated varix right after treatment. Figure 42.6 Radiographic image of the coil inside the varix.
42
How to do EUS‐guided Treatment of Gastric Varices
Introduction
Technique (Video 42.1)

Complicatons

Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree








