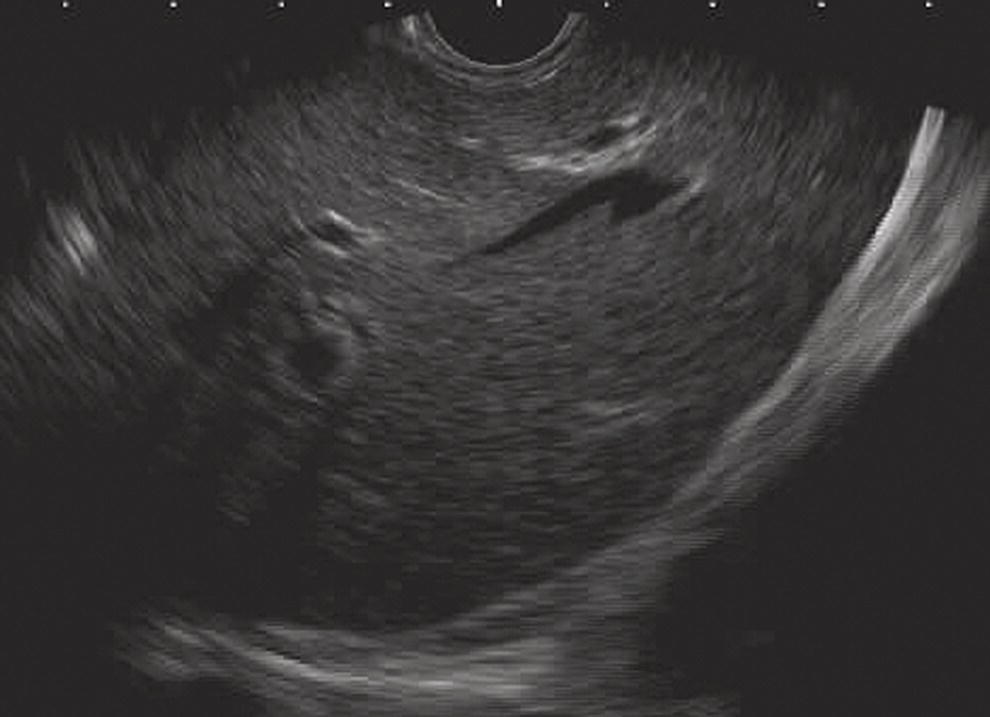
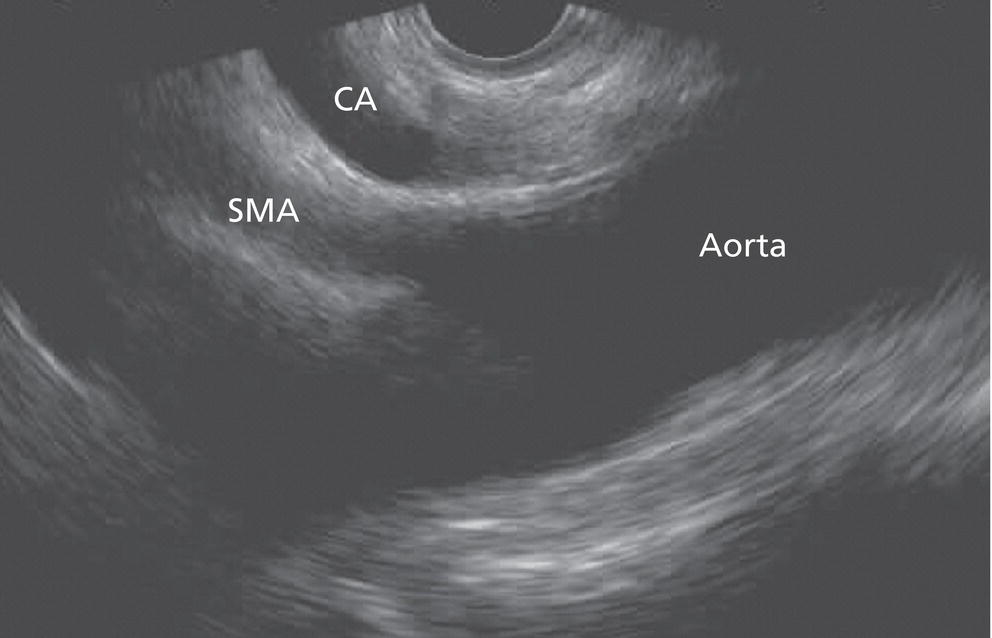
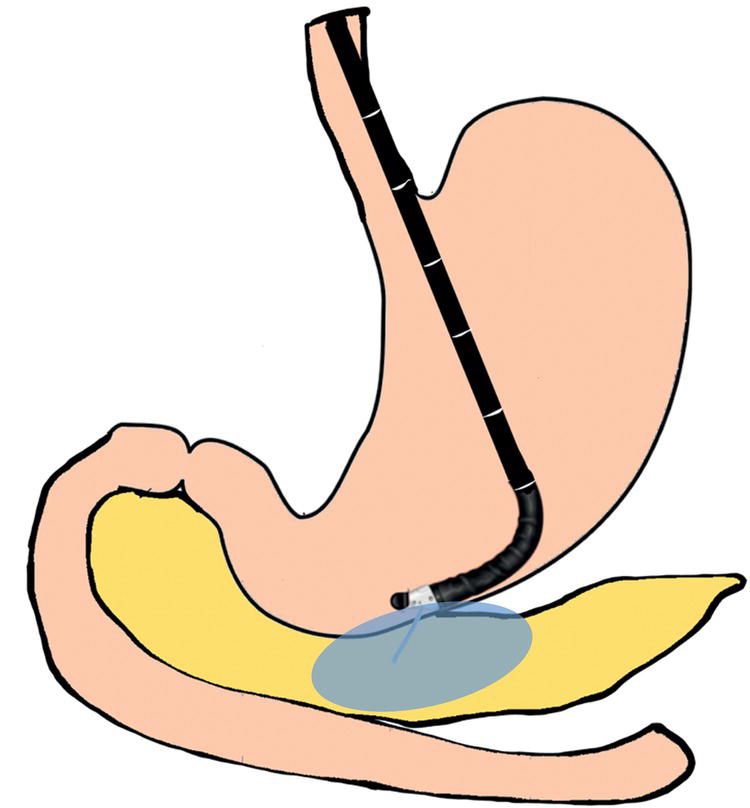
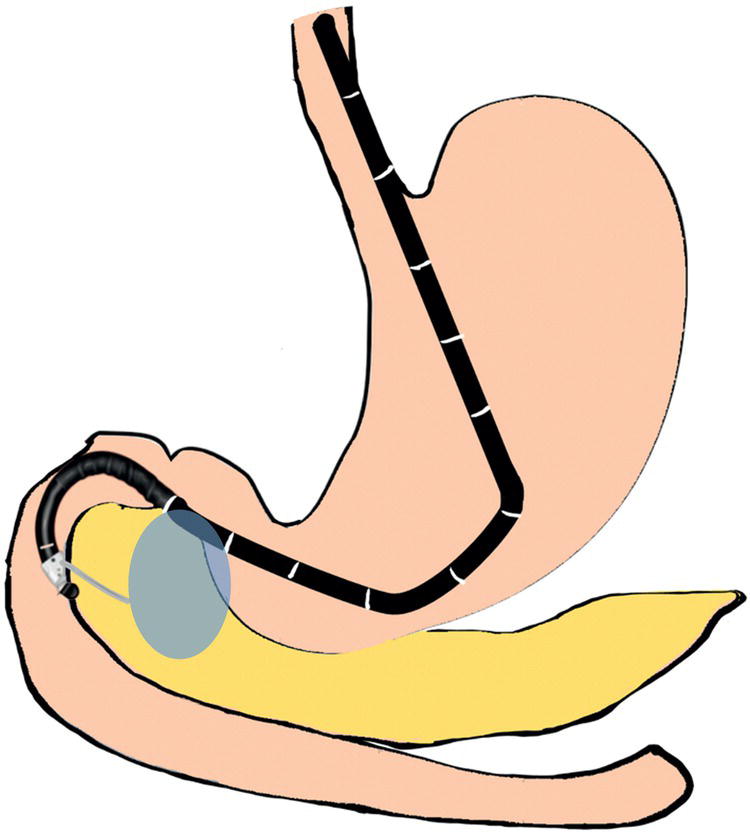
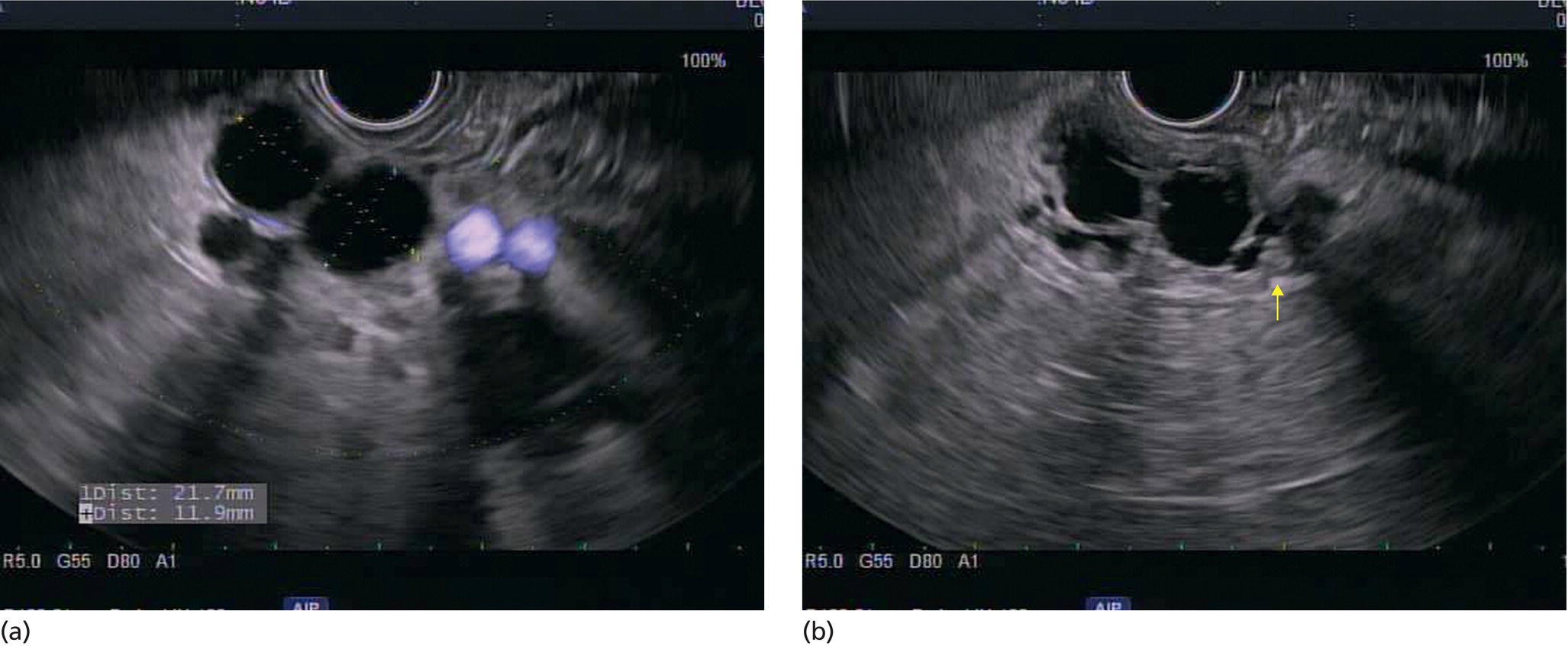
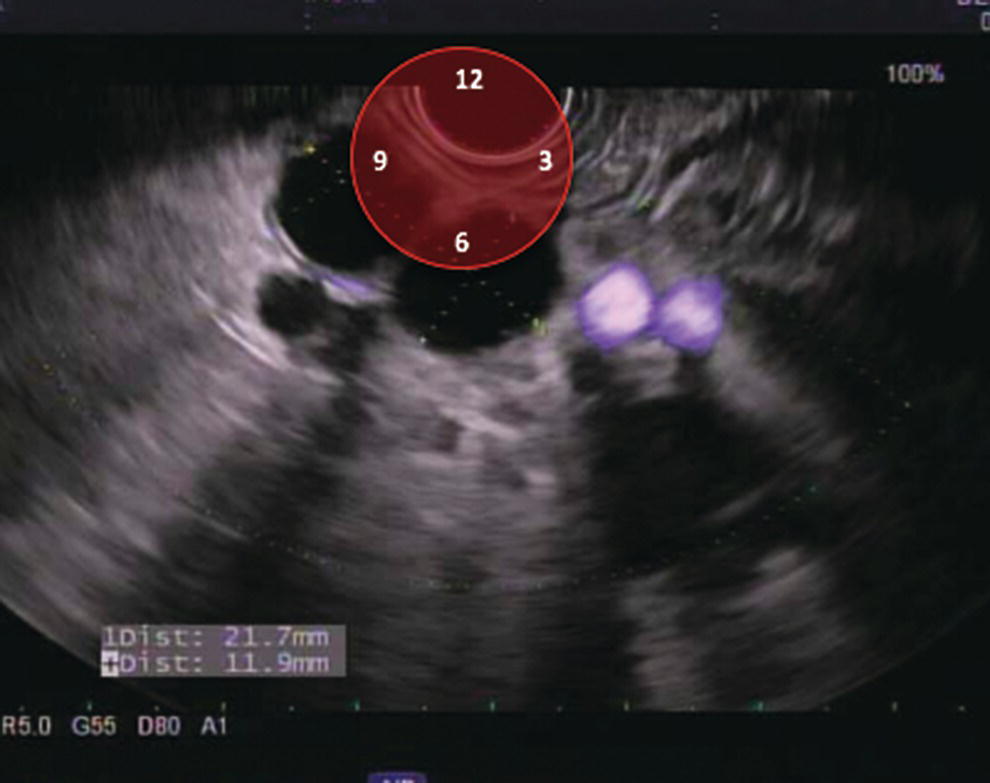
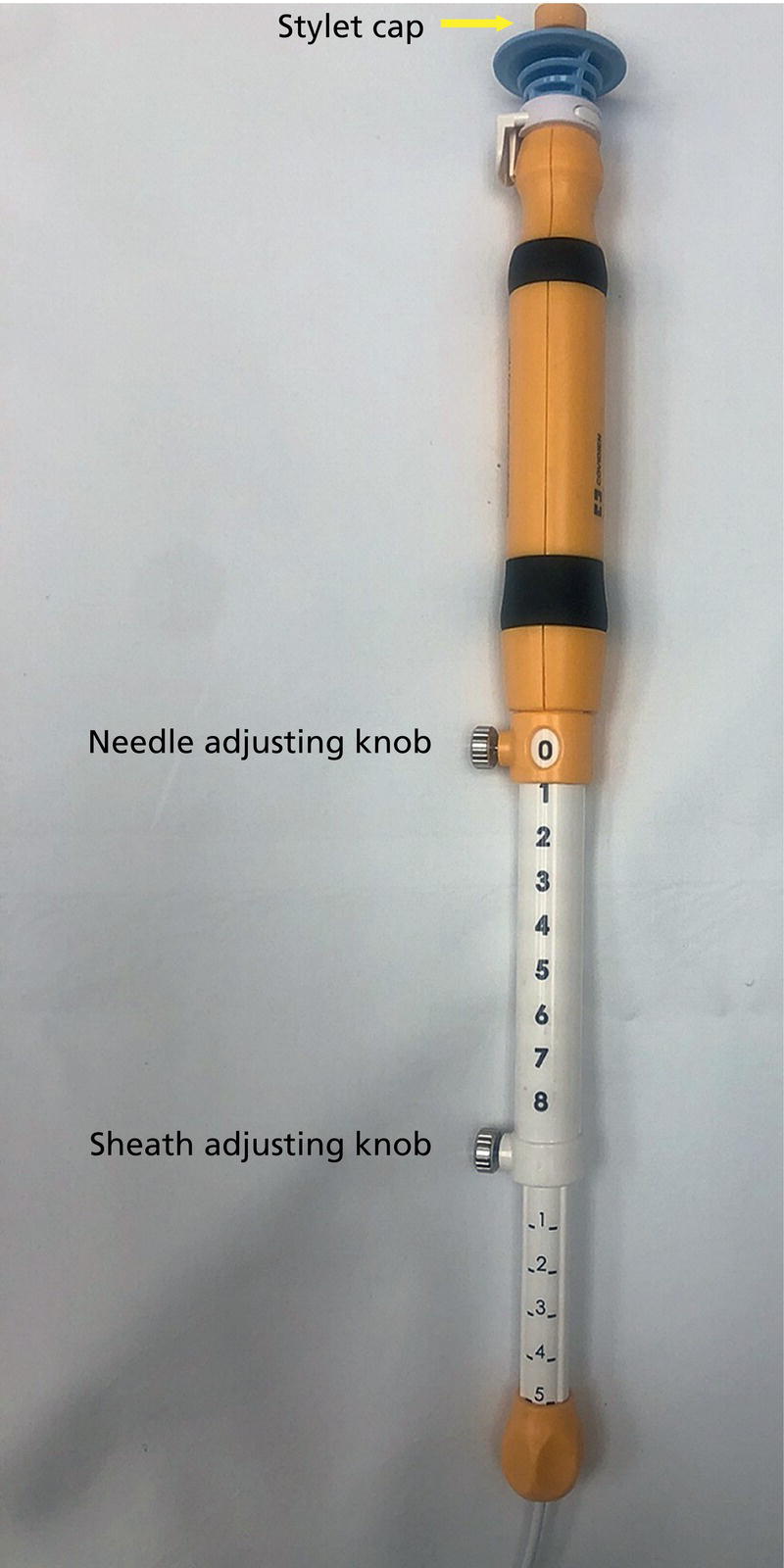
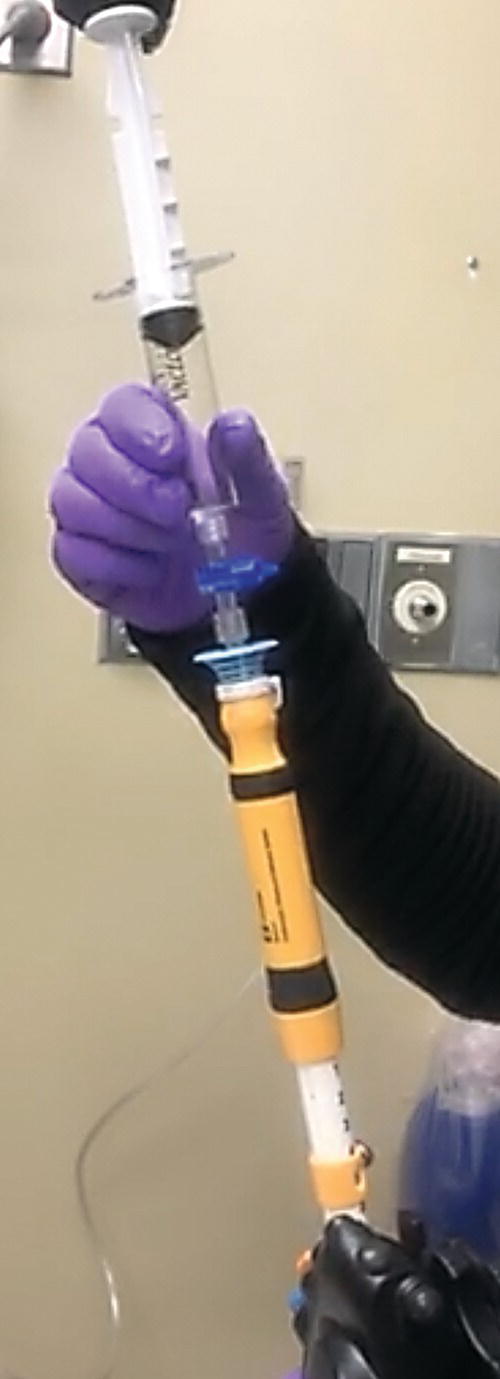
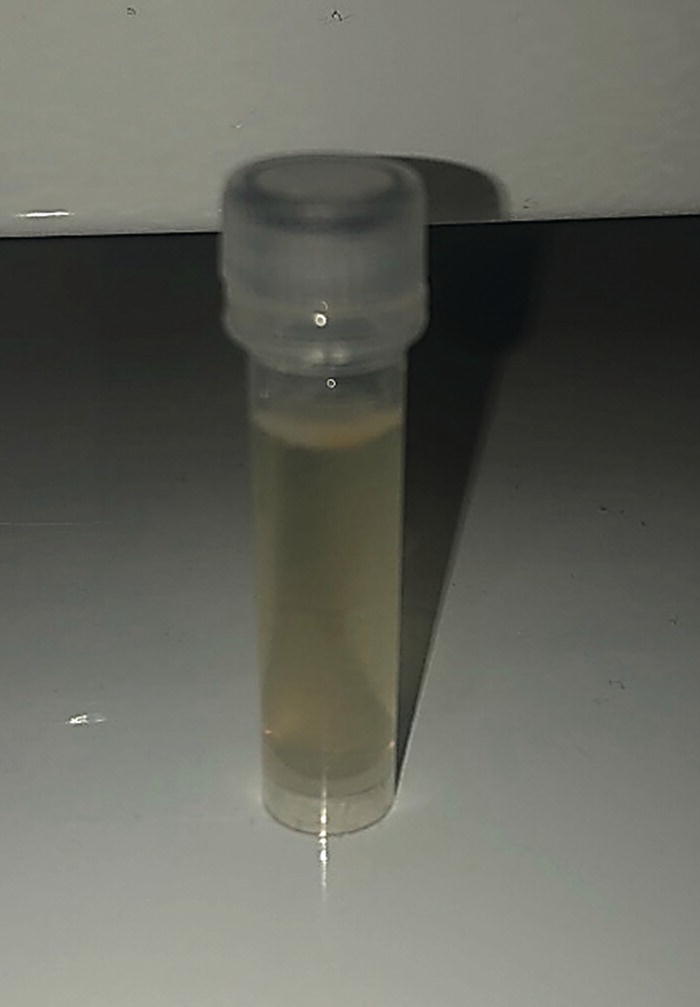
Ahmad Najdat Bazarbashi and Linda S. Lee Division of Gastroenterology, Hepatology and Endoscopy, Brigham and Women’s Hospital, Harvard Medical School, Boston, MA, USA Pancreatic cysts remain a challenge to diagnose and manage. Evaluation should focus on whether the cyst is malignant and, if not, the risk of malignant transformation. While magnetic resonance imaging (MRI) should be performed on all patients with pancreatic cysts if possible, endoscopic ultrasound (EUS) is an important complementary diagnostic tool for indeterminate cysts and cysts with concerning features. The value of EUS lies not only with its imaging of the cyst size, border, content, and surrounding structures, but also in its ability to aspirate cyst fluid and tissue via fine needle aspiration (FNA) or fine needle biopsy (FNB) for analyses. Because tissue diagnosis via FNA of pancreatic cysts is often limited by the paucicellular specimens, other diagnostic tests and tools have been explored including cyst fluid analysis and, more recently, FNB. EUS‐FNB may safely increase diagnostic yield and requires further study. What tests to send for cyst fluid analysis continue to evolve and may include amylase, carcinoembryonic antigen, glucose, molecular analysis, cytology and/or histology. Prior to EUS, the patient should undergo a thorough history and focused physical examination including history of pancreatitis, family history of pancreatic cancer, and smoking and alcohol intake as these may influence the differential diagnosis of the pancreatic cyst. Anticoagulation should be held after discussion with the prescribing clinician. Radiology images should be carefully reviewed to understand the patient’s anatomy and location of the pancreatic cyst(s), and to anticipate any potential difficulties in finding and sampling the lesion. When consenting patients, the endosonographer should detail the nature of the procedure, risks, benefits and alternatives. Risks to highlight include bleeding, infection, abdominal pain, pancreatitis, and perforation. Realistic expectations should be set for the patient, indicating that cyst fluid analysis and FNA/FNB are imperfect and do not always provide definitive diagnosis of the cyst. Antibiotic prophylaxis has been recommended by the American Society for Gastrointestinal Endoscopy for EUS‐FNA of pancreatic cystic lesions (typically a fluoroquinolone administered peri‐procedure and for three days afterwards). Esophagogastroduodenoscopy (EGD) is often performed prior to EUS to ensure there are no anatomical abnormalities that may interfere with passing the echoendoscope or with visualizing the pancreas and surrounding structures, for example an unknown surgery. Linear echoendoscope is preferred over radial echoendoscope since it allows for FNA or FNB. EUS examination should proceed methodically to avoid missing visualizing certain areas. One may begin by identifying important anatomical structures such as the liver (Figure 32.1) and aorta/celiac trunk (Figure 32.2). The pancreas can be found by gently pushing the echoendoscope forward in the stomach after identifying the celiac trunk and following the SMA to the pancreas or by rotating 180 degrees from the thickest portion of the left lobe of the liver. The genu, body, and tail are examined from the transgastric station (echoendoscope positioned towards the posterior wall of stomach; Figure 32.3), while the uncinate process and head of the pancreas are usually visualized transduodenally (echoendoscope in the duodenal bulb for the head and second portion of the duodenum for the complete head and uncinate process; Figure 32.4). Once the cyst is identified, it should be evaluated for size, shape, echogenicity, contents (mucin, septations, nodule, solid mass), thickness of wall, and communication with main pancreatic duct (Figure 32.5). Mucus appears hypoechoic relative to the adjacent tissue with a well‐defined hyperechoic rim while nodules are isoechoic/hyperechoic without a smooth border or hyperechoic rim. In preparation for biopsy, the cyst should ideally be located near the 6 o’clock position as close to the tip of the echoendoscope as possible using the large dial (Figure 32.6), and Doppler imaging used to ensure no vessels lie in the path of the needle (Figure 32.7). Figure 32.1 EUS of left lobe of liver. Figure 32.2 EUS of aorta, celiac artery (CA), and superior mesenteric artery (SMA). For FNA/FNB, 22G needles are usually used although thinner 25G needles may be considered for transduodenal punctures, especially into the uncinate process. This is because transduodenal punctures are often more difficult than the transgastric approach due to the angulated, long position of the echoendoscope in the duodenum. However, suctioning viscous fluid may be challenging through smaller‐caliber needles while 19G needles facilitate faster and easier aspiration of large and mucinous cysts. After removing the biopsy cap and advancing the needle device down the accessory channel of the echoendoscope, it is attached to the Luer lock at the accessory channel port. Both large and small dials on the echoendoscope should be locked to ensure slight movements or deviations are minimized during needle advancement. The position of the sheath may be adjusted using the bottom adjustable slider on the needle (Figure 32.8), which allows use of the various needles with the different brands of echoendoscopes. Once the sheath is visible, the sheath adjusting knob should be locked. The stylet should be pulled back slightly to expose the needle tip with certain FNB needles. How far to advance the needle can be estimated by measuring the distance from the tip of the echoendoscope into the cyst, and the adjustable needle knob (Figure 32.8) should be locked in place accordingly to prevent the needle from traversing too far. The needle is then slowly advanced out of the sheath; however, if difficulty is encountered, do not force the needle out as this may damage the echoendoscope. Adjust the position of the echoendoscope and unlock the dials to help the needle to exit easily. Once the needle is visible, slowly advance it to the gastric/duodenal wall, adjust the angle of entry as needed using the elevator, recheck Doppler to ensure no vessels are in the path of the needle, and thrust it rapidly and firmly into the cyst (Figure 32.9). The stylet may be pushed in completely to expel any gastric or duodenal wall tissue that may have been captured, after which it is completely removed and a 10‐ or 20‐ml syringe attached to the needle handle for suctioning cyst fluid. To prepare the syringe, air is completely expelled, the stopcock closed, and then the plunger pulled back and turned to lock into position to create a vacuum (Figure 32.10). Ideally the cyst is aspirated completely with one pass. Observe the cyst fluid accumulating in the syringe, and if frank blood is filling it, aspiration should stop. FNA/FNB of the collapsed cyst wall may be performed with short to‐and‐fro movements. If nodules or solid components were noted, these should be sampled in a similar fashion to solid pancreatic masses. Figure 32.3 Transgastric EUS examination of pancreas (genu, body, tail). Figure 32.4 Transduodenal EUS examination of pancreas (head and uncinate process). Figure 32.5 (a) EUS of anechoic septated lobular cyst in tail of pancreas. (b) EUS of anechoic septated lobular pancreatic cyst with nodule (yellow arrow) proven malignant on surgical resection. Source: Frank G. Gress. Figure 32.6 Position lesion at 6 o’clock for FNA/FNB. Source: Frank G. Gress. Figure 32.7 EUS with Doppler showing blood vessels (purple) in path of needle. Source: Frank G. Gress. Once aspiration is complete, suction should be turned off with or without removing the syringe before the needle is withdrawn from the lesion to avoid contamination of the collected specimen. The fully withdrawn needle is locked in position and then the needle removed from the echoendoscope. The fluid should be grossly examined for its color which may range from bloody to brown, serosanguinous, white, or serous (Figure 32.11). String sign should be assessed, if possible, by placing a drop of fluid between the index finger and thumb, pressing both together and then slowly pulling them apart to look for development of string‐like material, which is consistent with a mucinous cyst (Figure 32.12). Alternatively, one may observe for string sign in fluid being expressed from the tip of the EUS needle. The cyst fluid should be placed into a container for cyst fluid analyses. Tissue within the needle may be sent for cytology (FNA) or histology (FNB). Figure 32.8 EUS needle handle. Source: Frank G. Gress. Figure 32.9 FNA needle within pancreatic cyst (yellow arrow indicates tip of needle). Source: Frank G. Gress. Figure 32.10 Vacuum syringe. Source: Frank G. Gress. EUS is an important diagnostic tool for evaluating pancreatic cystic lesions that are indeterminate or have concerning features on radiology imaging. Careful review of imaging is important. Regarding the technique of sampling pancreatic cysts, FNB needles may safely provide higher diagnostic yield than FNA needles and require further study. While smaller‐gauge needles are easier to use in a transduodenal approach, suctioning viscous fluid through them may be more challenging than with a larger‐gauge needle. Ideally one pass is used to aspirate the cyst completely, and the collapsed cyst wall may be sampled. Cyst fluid should be assessed for string sign, if possible, and sent for the desired testing. Nodules and solid masses must be sampled as well. Antibiotics should be administered periprocedurally. Figure 32.11 Serous fluid aspirated from large pancreatic cyst. Source: Frank G. Gress. Figure 32.12 String sign consistent with mucinous cyst. Source: Frank G. Gress.
32
How to do Pancreatic Cyst FNA
Introduction
Technique (Video 32.1)


Summary

Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree