How to Optimize CT for PET/CT
Gerald Antoch
Andreas Bockisch
Dual-modality positron emission tomography plus computed tomography (PET/CT) imaging systems permit the combined acquisition of functional and morphological data within a single session (1). Diagnostic advantages of PET/CT for staging compared to CT alone or PET alone have been reported for many different malignant diseases (2,3,4,5). By integration of CT with PET, PET/CT overcomes the major limitation of CT alone, which is the lack of relevant functional data. Compared to PET alone, correlation of function with CT offers the opportunity for accurate location of a lesion in question. However, the question now is, how good must the quality of CT be to optimize anatomical correlation for PET? When comparing CT protocols in use for PET/CT imaging worldwide, a wide variety of imaging protocols have been proposed and applied, and the “correct” way of acquiring the CT portion of the combined examination has been a matter of great debate. Are low-dose and noncontrast enhanced CT data sufficient or does diagnostic PET/CT require contrast-enhanced and full-dose CT? Does the quality of the CT component affect the diagnostic accuracy of the combined imaging procedure? If contrast agents are of benefit, do we need contrast-enhanced CT in every PET/CT or should we decide on a case-by-case basis? To address these questions this chapter will give an overview of currently available CT imaging protocols and will discuss in which clinical situation each protocol may be beneficial. It also must be recognized that this field continues to evolve rapidly, so the final and optimal combination of PET and CT for diagnosis is not yet fully resolved for all clinical situations.
CT Contrast Agents
Oral Contrast Agents
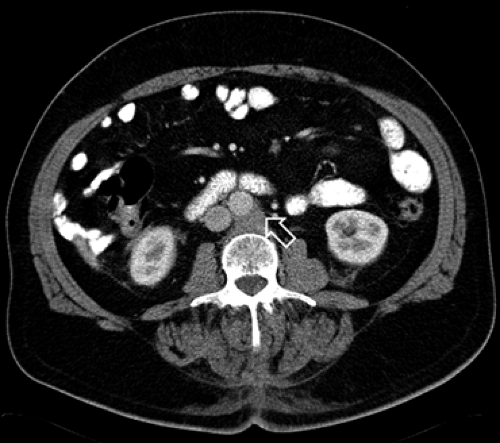
Nondistended intestinal structures, adjacent organs, and lymph nodes are characterized by similar Hounsfield units, which range from 30 to 60 H, slightly higher than that of water (Fig. 8.2.1). An oral contrast agent is required to differentiate the bowel from adjacent structures and potential pathological findings. Oral contrast agents have been in use for PET/CT imaging for some years, and their value in marking intestinal structures has been accepted by most groups worldwide. There are two oral contrast agents available: positive and water-equivalent (negative) agents.
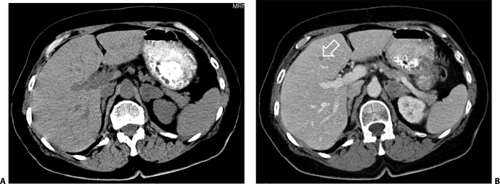
Positive oral contrast agents lead to an increase in the Hounsfield units of the intestine. By marking the intestinal lumen, the bowel can be differentiated from surrounding structures (Fig. 8.2.2). For positive intestinal contrast, either a barium-based or an iodine-based contrast agent may be applied. Barium is usually administered as a 1.0% to 2.5% suspension in water, while the iodine-based agent is often administered as a 1% to 3% solution in water. The concentration of the contrast agent may differ among institutions. However, the maximal concentration of the positive oral contrast agent is limited by two factors: (a) higher concentrations of the oral contrast agents may lead to artifacts on CT, and (b) artifacts may occur in the PET image if PET attenuation correction is based on the CT data from a PET/CT study (see below). Based on the increase in intraluminal Hounsfield units, positive oral contrast agents are valuable to differentiate the intestine from adjacent structures including pathological lymph nodes. However, intraluminal lesions and the bowel wall cannot be accurately assessed if there is only limited intestinal distension.
Water-equivalent oral contrast agents distend the intestinal lumen. These contrast agents have also been referred to as negative contrast agents because they do not opacify the intestine, although they do make it visible. Since air has been widely known as a negative contrast agent for conventional radiography, the term negative may be somewhat misleading, as water-based agents are used for intestinal distension rather than the ones based on air in PET/CT. The water-based agent leads to intestinal distension with intraluminal Hounsfield units of 0 to 20. To avoid intestinal absorption of water during the PET/CT scan, different substances may be added; currently a combination of 1.5 L of water containing 2.5% mannitol and 0.2% of locust bean gum is used. The osmotic property of mannitol improves bowel distension, and locust bean gum has a gelling quality that avoids water resorption (6). This water-equivalent contrast agent is pharmacy provided within some hospitals, but other water-equivalent oral contrast agents have become commercially available. Hausegger et al. (7) have evaluated a commercially available vegetarian-based negative oral contrast agent for PET/CT.
Excellent intestinal distension was reported in 85% of patients in this study.
Excellent intestinal distension was reported in 85% of patients in this study.
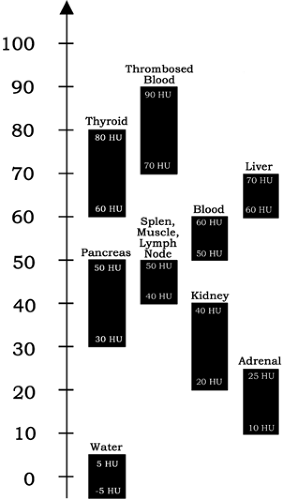 Figure 8.2.1. Densities of different organs and of pathology as expressed in Hounsfield (H) units. The most clinically relevant structures have similar Hounsfield units ranging between 10 and 90 H. |
The intestinal distension provided by water-equivalent oral contrast agents offers a more accurate assessment of the intestinal wall. This can be of benefit over positive oral contrast agents if a tumor adjacent to the bowel is suspected to invade the intestinal wall. Furthermore, the detection of intraluminal tumors may be easier than with positive oral contrast agents (Fig. 8.2.3). A limitation of water-equivalent contrast agents is the differentiation of a distended bowel loop from a centrally necrotic lymph node. In patients with suspected lymph node necrosis, a positive oral contrast agent may be more valuable than a water-equivalent agent. As oral contrast agents are prepared, it is important to avoid using lemonade or other materials that contain glucose as these can raise serum glucose and insulin levels, thus degrading scan quality.
Intravenous Contrast Agents
Parenchymal organs, blood vessels, muscles, and lymph nodes have similar density, as represented by Hounsfield units in the range of 30 to 70 H (Fig. 8.2.1). Even when considering a soft-tissue CT window, differentiation of these anatomical structures from one another often will be limited due to overlapping tissue densities. Parenchymal lesions, such as liver metastases, frequently have similar Hounsfield units as their harboring organ (Fig. 8.2.4). To overcome this limitation of noncontrast enhanced CT data sets, intravenous contrast agents can be applied. Since uptake characteristics of the contrast agents differ in parenchymal organs, in other organs, and in pathological tissue, this leads to more accurate differentiation of anatomical structures (8,9,10) and to a higher accuracy in lesion detection (11,12). If more than one contrast-enhancing phase is acquired, this can aid in more accurate characterization of a lesion’s etiology on CT.
Intravenous contrast agents are iodine-based, nonionic substances with low osmolarity. Compared to former ionic agents, nonionic contrast has been reported to cause fewer adverse events.
However, although adverse events are less common than with ionic contrast agents, they may occur with nonionic contrast agents. These may include nephrotoxicity, thyrotoxic effects, and allergic reactions to the contrast material.
However, although adverse events are less common than with ionic contrast agents, they may occur with nonionic contrast agents. These may include nephrotoxicity, thyrotoxic effects, and allergic reactions to the contrast material.
Acute adverse reactions have to be differentiated from delayed allergic reactions. Although acute effects occur within the first 30 minutes after the injection of the contrast material, delayed allergic reactions may occur up to 48 hours following the contrast media administration. Based on the contrast agent used, the concentration of iodine may differ between 200 and 370 mg iodine/mL. For most CT studies, as well as for contrast-enhanced PET/CT, a contrast agent with a concentration of 300 mg iodine/mL seems adequate. Higher concentrations are used for special indications such as visualization of hypervascular lesions with CT.
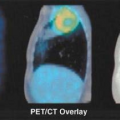
Effect of CT Contrast Agents on Attenuation-corrected PET Data
To potentially improve PET image quality and reduce examination times by as much as 30%, the CT data are generally used for attenuation correction purposes in combined PET/CT. Based on the two-step scaling algorithm implemented for attenuation correction in all currently available PET/CT scanners (13), PET attenuation can be overestimated in the presence of positive contrast agents (14,15,16,17). A threshold is set to separate soft tissue from bone. To obtain the corresponding attenuation map at 511 keV, CT values are scaled with a scaling factor for either soft tissue or bone. Compared to annihilation photons of 511 keV used in PET, CT and x-rays with energies of 70 to 140 keV are attenuated substantially more by structures containing elements of high atomic numbers such as iodine and barium. If not accounted for, contrast agents may lead to a bias in the estimated attenuation coefficients, which may translate into artifacts in the corrected PET images.
These artifacts are correlated with Hounsfield units on CT images. The higher the Hounsfield units based on positive contrast enhancement, the more distinct the area of apparently increased tracer uptake (18,19). When considering intravenous contrast agents these PET artifacts may be found in coregistration with a contrast-enhanced blood vessel, typically in thoracic veins carrying undiluted contrast following contrast injection (18) (Fig. 8.2.5).
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree