Hypersensitivity Pneumonitis, Chronic
Jud W. Gurney, MD, FACR
Key Facts
Terminology
Chronic granulomatous lung disease caused by inhalation of variety of organic and chemical antigens
Imaging Findings
Ground-glass opacities + centrilobular nodules + lobular hyperinflation + signs of fibrosis (traction bronchiectasis, irregular reticular lines, honeycombing)
Mid lung more common, especially in bird breeders and those with continuous exposure
Upper lung zone more common in farmers (intermittent exposure)
Emphysema (20%) more common in farmer’s lung as compared to other agents
Patterns of fibrosis may be either NSIP or IPF
Mild degrees of irregular linear opacities and traction bronchiectasis may be partially or fully reversible
Top Differential Diagnoses
Idiopathic Pulmonary Fibrosis (IPF)
Nonspecific Interstitial Pneumonia (NSIP)
Sarcoidosis
Pathology
Chronic HP thought to result from low-level or recurrent exposure
Clinical Issues
Diagnosis often delayed for years, mean 3 years
Disease may progress despite elimination of antigen exposure
Prognosis depends on degree of fibrosis
TERMINOLOGY
Abbreviations and Synonyms
Extrinsic allergic alveolitis, hypersensitivity pneumonitis (HP), farmer’s lung
Definitions
Chronic granulomatous lung disease caused by inhalation of variety of organic and chemical antigens
Farmer’s lung and bird fancier’s lung are most common forms
IMAGING FINDINGS
General Features
Best diagnostic clue: Ground-glass opacities + centrilobular nodules + lobular hyperinflation + signs of fibrosis (traction bronchiectasis, irregular reticular lines, honeycombing)
Patient position/location
Mid lung more common, especially in bird breeders and those with continuous exposure
Upper lung zone more common in farmers (intermittent exposure)
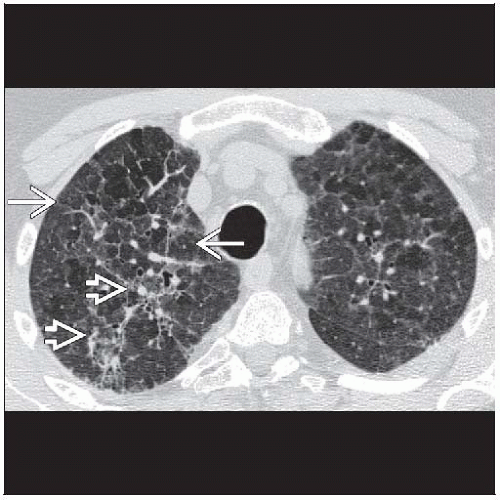
CT Findings
Background of subacute findings: Ground-glass opacities and small ill-defined centrilobular nodules
Ground-glass opacities, often in geographic distribution (100%)
Centrilobular nodules (60%), usually ground-glass density < 5 mm in diameter
Mosaic perfusion pattern (60%)
Lung cysts (30%), nearly always seen in conjunction with ground-glass opacities
Thin-walled 3-25 mm in diameter, usually few in number (mean 4) range from 1-15
Individual signs alone nonspecific, combinations more helpful
Geographic ground-glass attenuation + normal lung + mosaic perfusion + centrilobular nodules
Ground-glass opacities + centrilobular nodules + lobular air-trapping
Chronic HP depends on signs of fibrosis
Irregular linear opacities (40%)
Traction bronchiectasis (20%)
Honeycombing (50%)
Emphysema (20%)
Patients with HP tend not to be smokers
Emphysema more common in farmer’s lung as compared to other etiologies
Patterns of fibrosis may be either NSIP or IPF
In IPF, most inferior lung (posterior costophrenic angles) is usually severely involved (relatively spared in HP)
In NSIP, peribronchovascular ground-glass opacities and basilar distribution similar (centrilobular nodules and lobular hyperinflation uncommon in NSIP)
Distribution of disease
Bird breeders: Mid lung zone predominant
Farmer’s lung: Upper lung zone predominant
Distinction may reflect intermittent exposure (farmers) vs. continuous exposure (bird breeders) to offending antigen
Relative sparing costophrenic angles
Posterior costophrenic angles less involved than other areas in lung, in contrast to IPF in which this lung usually is most severely involved
Associated findings
Mediastinal adenopathy (50%), nodes < 20 mm short axis diameter
Pleural effusions rare
Resolution
Mild degrees of irregular linear opacities and traction bronchiectasis may be partially or fully reversible
Accuracy of diagnosis
If highly confident of diagnosis (up to 60% of cases of chronic HP) you will be correct 90% of the time
Most common mimics: IPF and NSIP
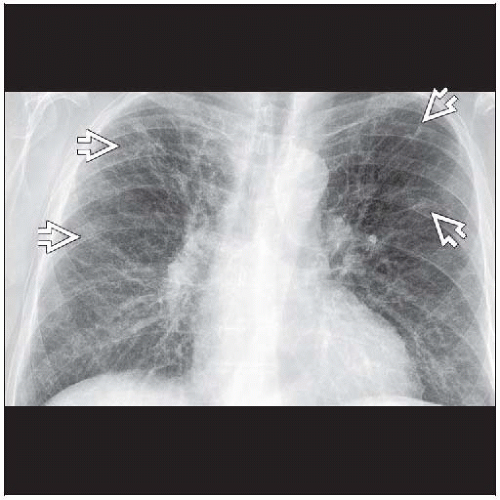
Radiographic Findings
Radiography
Findings of fibrosis
Architectural distortion, volume loss, variable distribution: Upper, mid, or lower zone predominant
Imaging Recommendations
Best imaging tool: HRCT much more specific than chest radiography for fibrosis
DIFFERENTIAL DIAGNOSIS
Idiopathic Pulmonary Fibrosis (IPF)
Striking subpleural distribution, not as common with HP
Honeycombing prominent, ground-glass opacities less common
Inferior costophrenic angles usually most severely abnormal lung (basilar peripheral lung)
May not be spared but not most severely involved lung in HP
Air-trapping not a feature
Nonspecific Interstitial Pneumonia (NSIP)
Ground-glass opacities > reticulation
Traction bronchiectasis usually out of proportion to degree of reticulation
Peripheral &/or peribronchovascular distribution
Centrilobular nodules not a feature
Air-trapping not a feature
Sarcoidosis
Peribronchovascular distribution, subpleural nodules, adenopathy
Subpleural lymphatic deposits rare in HP
Predominantly upper lung zones
Silicosis
Occupational history of dust exposure
Predominantly upper lung zones
May develop progressive massive fibrosis, not seen with chronic HP
Subpleural lymphatic deposits rare in HP
Air-trapping not a feature