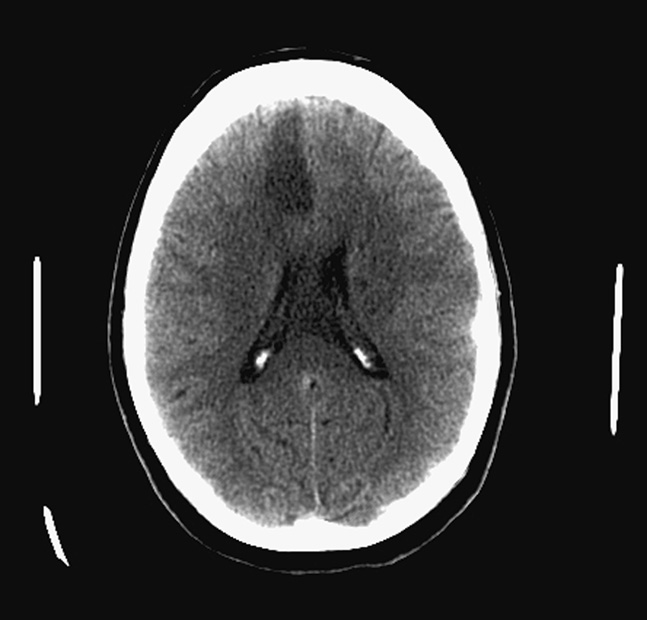
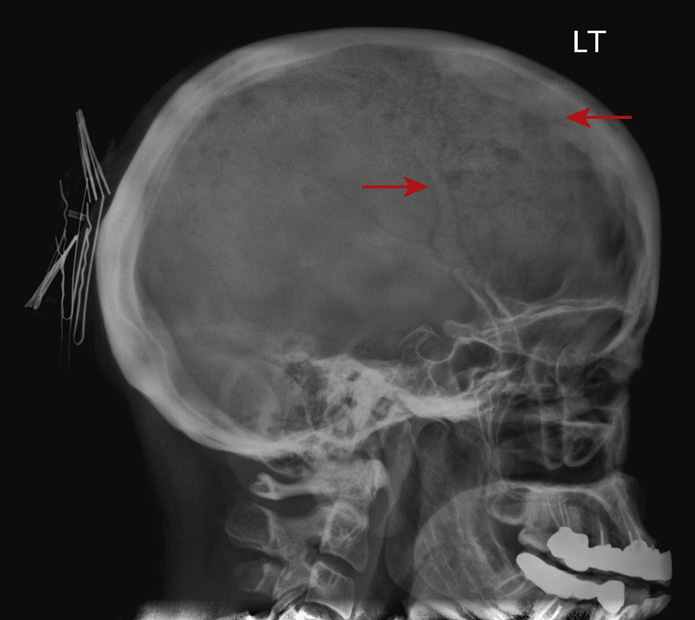
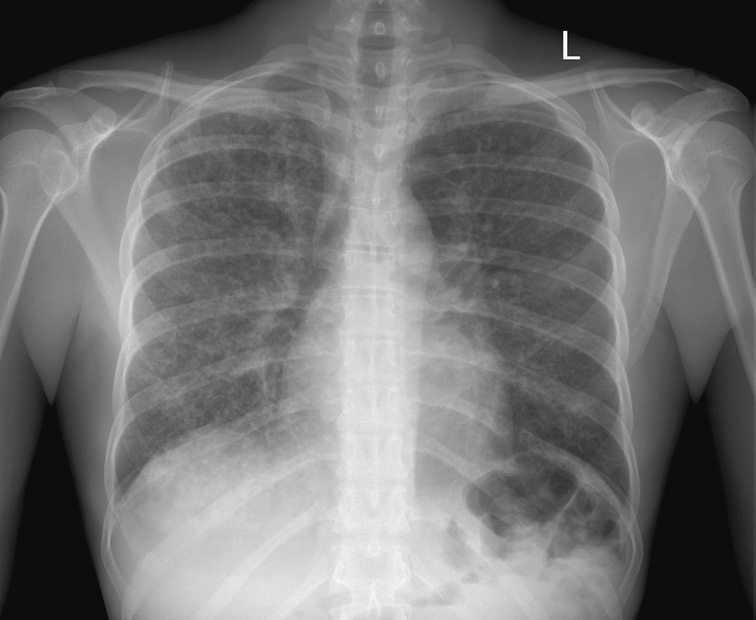
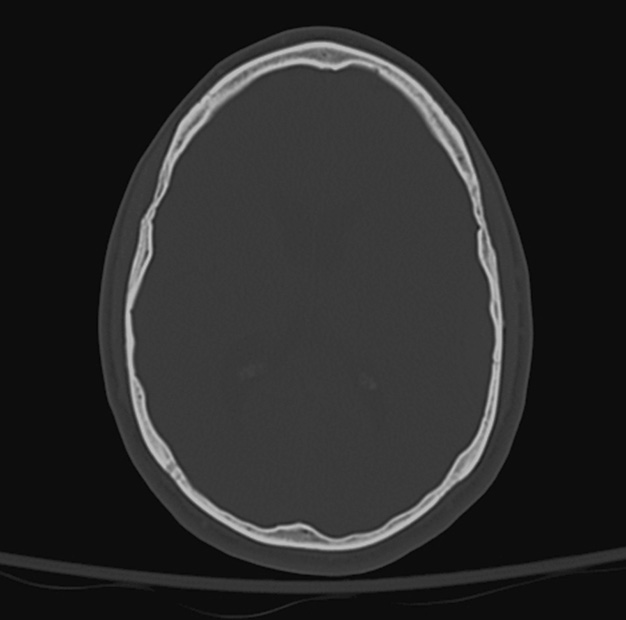
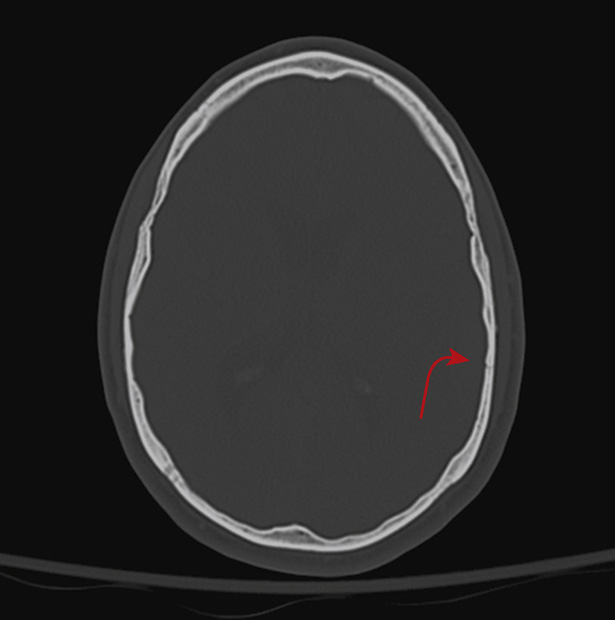
1. A 69-year-old woman with a history of poorly controlled hypertension and type 2 diabetes mellitus presented with a history of left-sided weakness and sensory deficit predominantly involving the lower limb, with hypobulia. The computed tomography (CT) scan is above. The most likely cause of the above finding is:
A. Hypertensive intracranial hemorrhage
B. Atherosclerotic occlusion of the right middle cerebral artery (MCA)
C. Atherosclerotic occlusion of the right anterior cerebral artery (ACA)
D. Ischemic infarction secondary to hypoperfusion
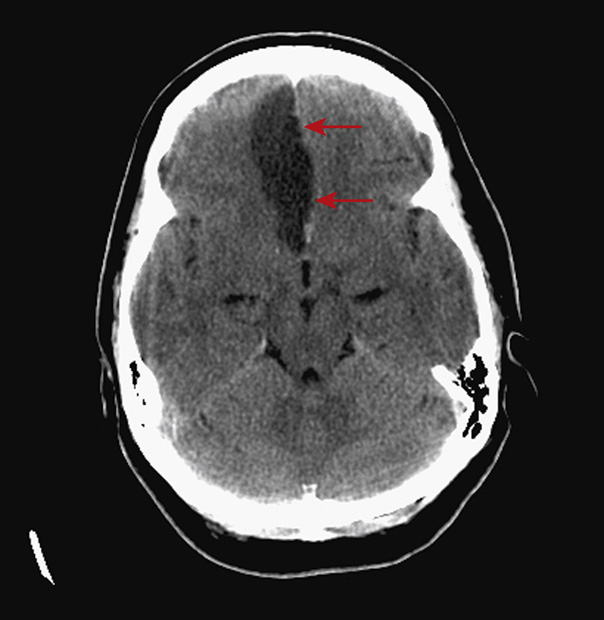
1. The answer is C: Atherosclerotic occlusion of the anterior cerebral artery (ACA). There is hypodensity (arrows) with mild mass effect involving the paramedian right frontal lobe. This is consistent with an ACA territory acute ischemic infarct. The most common cause of an ischemic ACA territory infarct is atherosclerotic occlusion, typically at the A2 origin. The patient’s history of hypertension and type 2 diabetes predispose her to atherosclerotic disease.
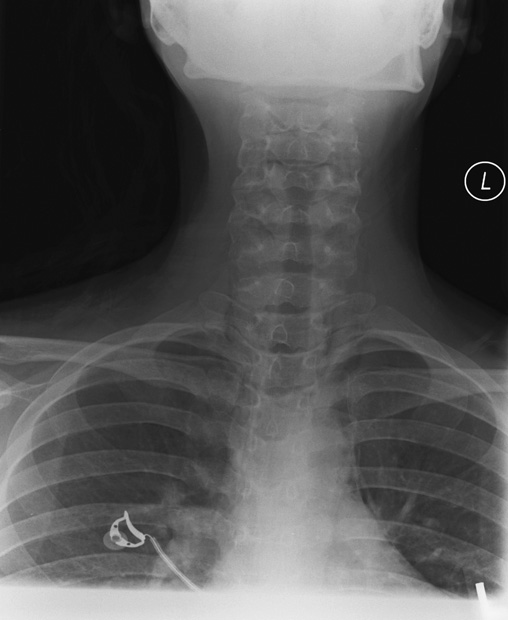
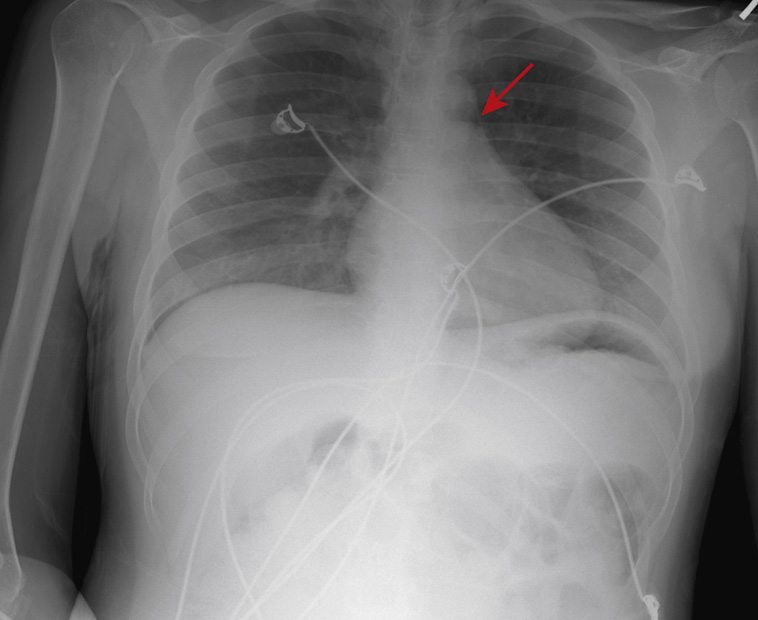
2. A 20-year-old woman with a history of asthma presents to the emergency department complaining of chest and neck discomfort. Her chest x-ray (top) and neck x-ray (bottom) are shown above.
Which of the following is the correct diagnosis?
D. Hyperinflation without extra pulmonary air
E. Pneumothorax and pneumomediastinum
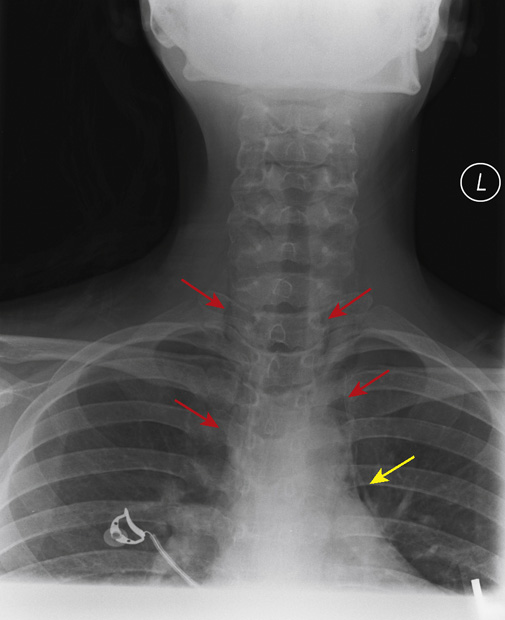
2. The answer is A: Pneumomediastinum. Spontaneous pneumomediastinum may occur in any patient with coughing or straining, but it is more common among asthmatics. The cause is believed to be spontaneous rupture of a small bleb along the medial pleural surface, close to the mediastinum. This patient’s symptoms of sudden onset of chest discomfort with chest and neck tightness is a typical clinical manifestation of spontaneous pneumomediastinum, which requires no treatment in this situation. A chest x-ray is done to be certain there is no pneumothorax, which may require treatment with a chest tube.
The chest x-ray shows faint lucent streaks of air along the borders of the superior mediastinum (yellow arrows). The neck x-ray shows more obvious lucent streaks extending from the superior mediastinum into the soft tissue planes of the neck (red arrows). In this case, a chest CT (third figure) was also performed, confirming mediastinal air dissecting into the neck, although CT evaluation is not mandatory in this benign clinical situation. Had the patient been vomiting or had she swallowed something sharp, there would be reason to suspect an esophageal tear, and a Gastrografin swallow and chest CT would be required.
B, E. No pneumothorax is visible on the chest x-ray. The lung apices are also well visualized on the neck x-ray, with no evidence of pneumothorax.
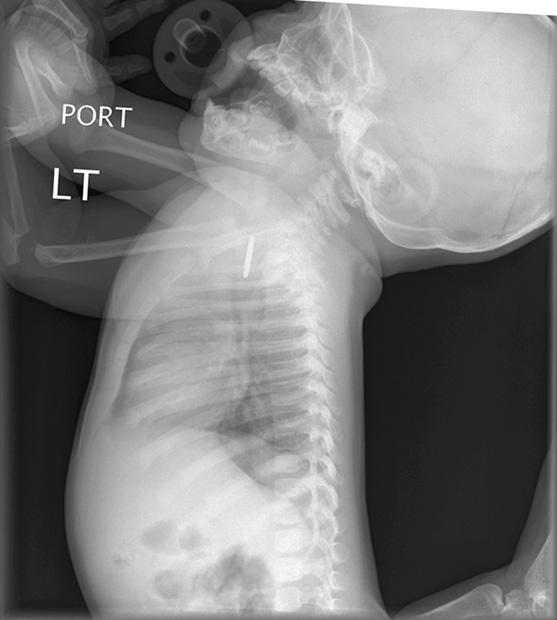
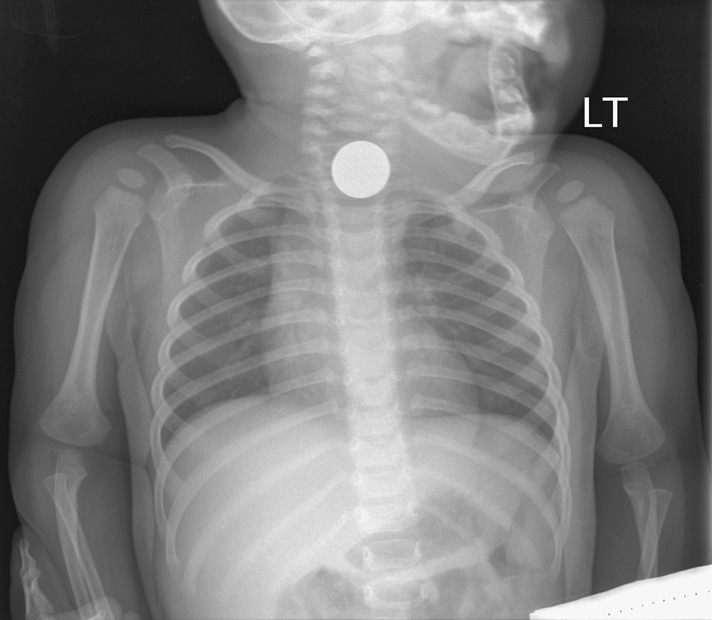
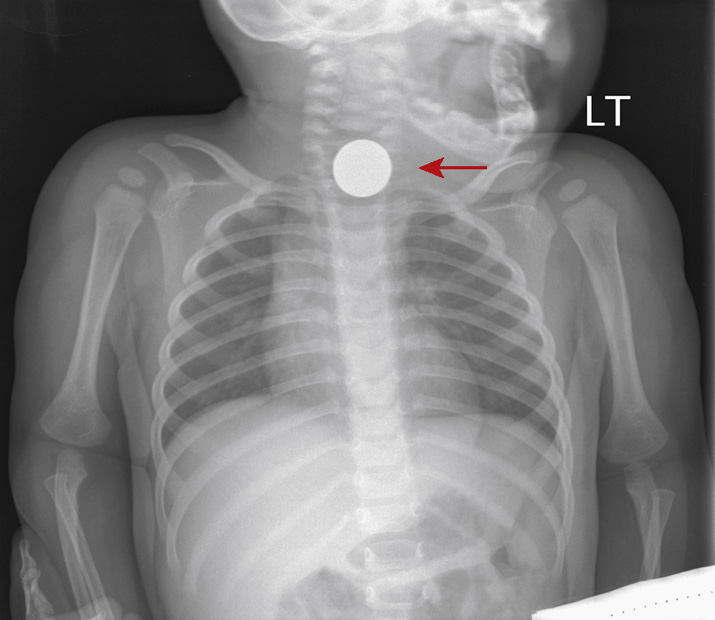
3. A mother reports to the pediatrician with her 9-month-old son with a chief complaint of refusal to feed today and increased drooling. The infant is inconsolably crying, making auscultation of the lungs difficult, but appears dyspneic, and between cries the physician hears stridor. The child is transferred to the nearest emergency department and anteroposterior (AP) and lateral chest radiographs are obtained. Which of the following statements is true?
A. Based on the radiographic findings, a bronchoscopy should be performed immediately.
B. The right lung is hyperinflated relative to the left.
D. Dyspnea and stridor can occur in children when a foreign body is within the esophagus.
Foreign Body in Esophagus (Coin)
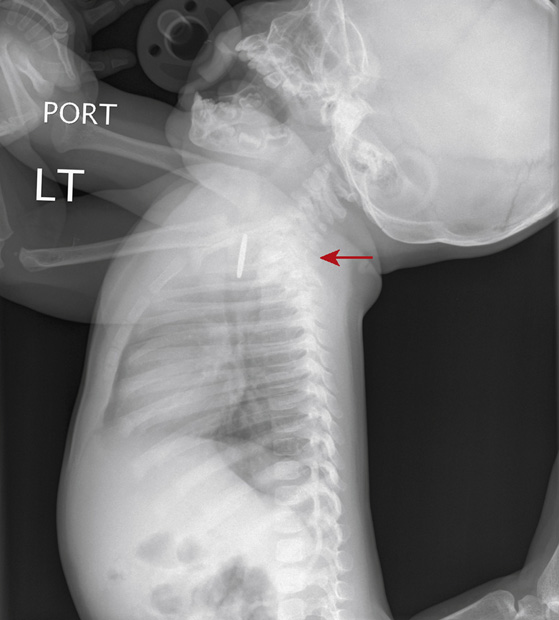
3. The answer is D: Dyspnea and stridor can occur in children when a foreign body is within the esophagus. This infant presents with fairly typical signs and symptoms of foreign body ingestion/aspiration. The radiographs confirm the presence of a circular metallic foreign body at the level of the thoracic inlet, posterior to the trachea on the lateral view, and in a coronal orientation (arrows); thus, impacted within the esophagus. A clue that the presumed coin is in the esophagus on the AP radiograph is its coronal orientation (en face), because a coin-shaped object would favor a sagittal orientation (en profil) within the trachea (due to the incomplete posterior cartilaginous rings of the trachea). Foreign bodies within the esophagus can have mass effect on the posterior trachea and induce dyspnea and stridor, especially at the thoracic inlet, often confounding the clinical presentation.
Foreign body aspiration/ingestion is a common cause of respiratory and gastrointestinal (GI) malady in the pediatric population. Potential complications of esophageal foreign bodies include impaction, laceration, and perforation. Aspirated or ingested foreign bodies can manifest with both acute and chronic symptoms and signs. The preferred method of extraction of impacted esophageal foreign bodies is through endoscopy, with overall a minimal complication rate.

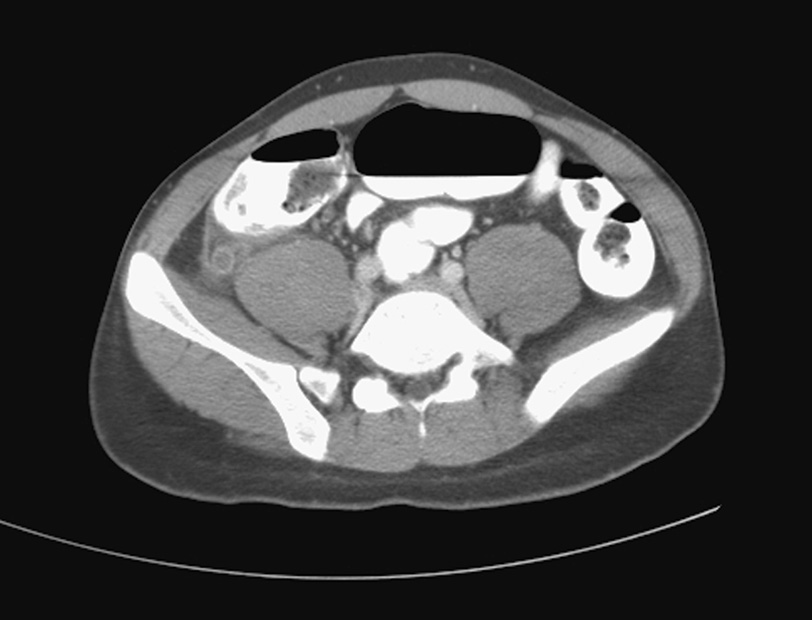
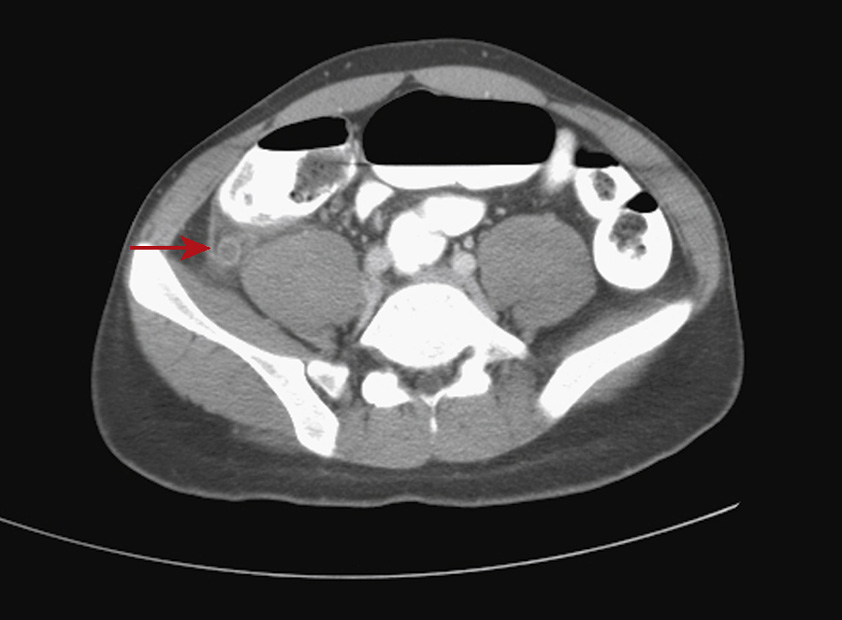
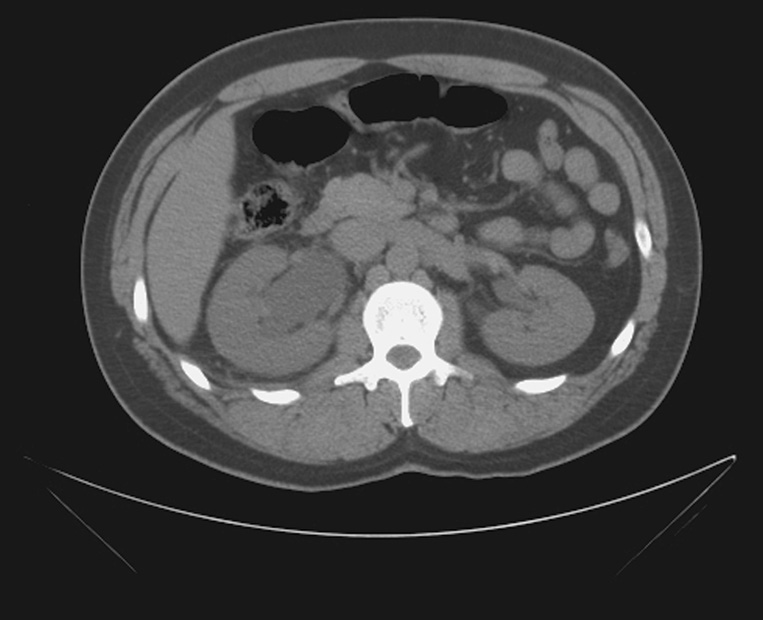
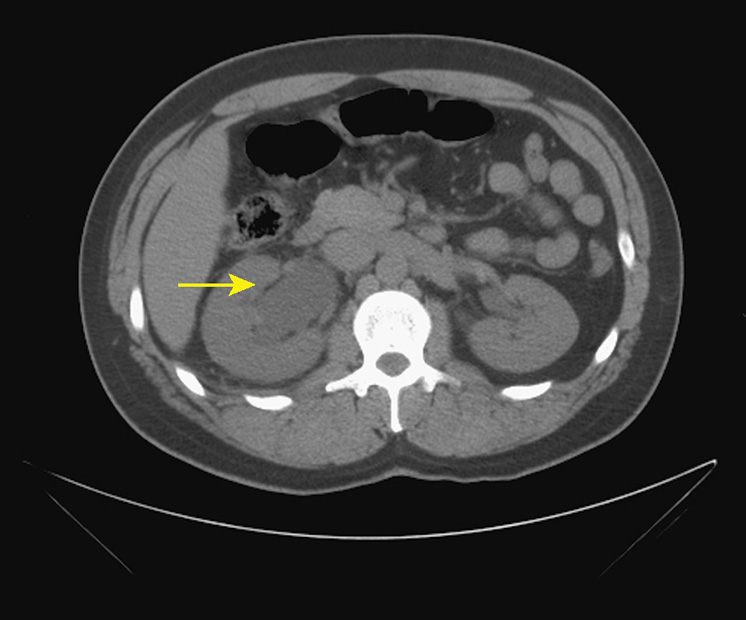
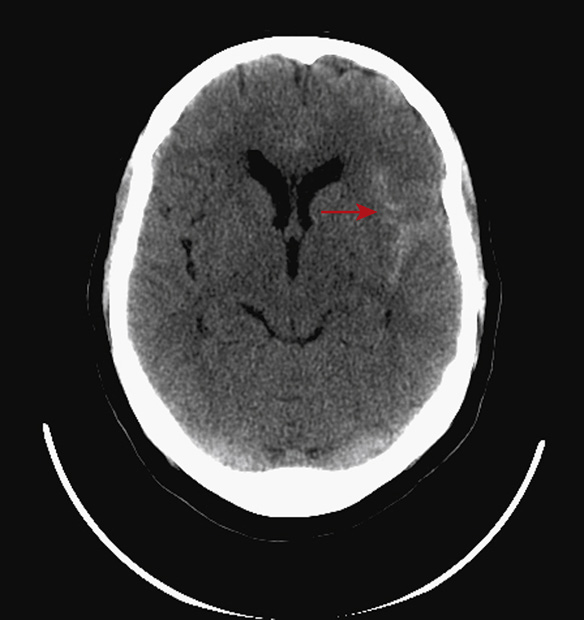
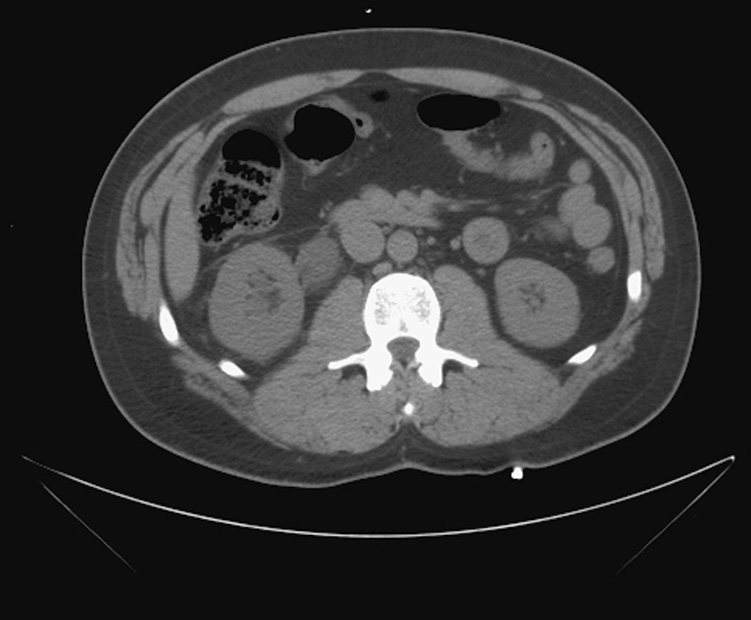
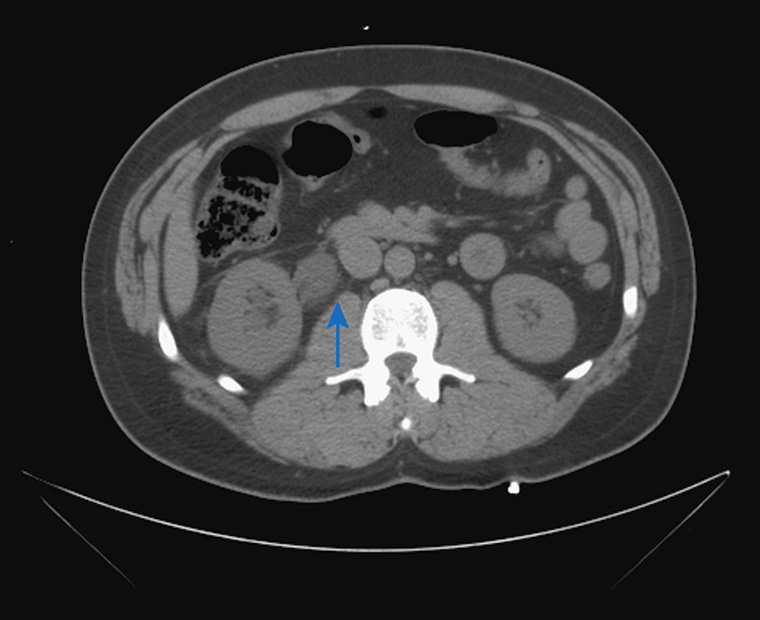
4. A 23-year-old man presents to the emergency department with fever, nausea, and vomiting and is found to have diffuse abdominal tenderness and a leukocytosis. A CT of the abdomen is performed. Which of the statements regarding the CT findings is correct?
A. The pericecal fat is normal in density.
B. The appendix is abnormally dilated, and its wall is abnormally enhancing.
C. This appendix is likely to be compressible on ultrasound.
E. There is strong evidence of appendiceal perforation.
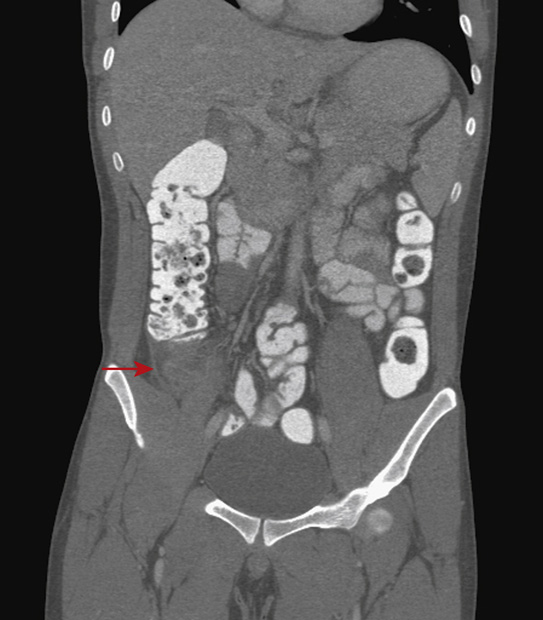
4. The answer is B: The appendix is abnormally dilated and its wall is abnormally enhancing. This is a fairly typical presentation for appendicitis. On the images above, there is a dilated, retrocecal appendix (red arrows) with avid wall enhancement and marked periappendiceal fat infiltration, all findings supporting a diagnosis of acute appendicitis. On CT the appendix should be less than 7 mm in diameter. A fluid-filled appendix without intraluminal air or contrast (if administered), and cecal inflammation can add to the suspicion.
Acute appendicitis is due to luminal obstruction, usually at the ostia (by an appendicolith or hypertrophied Peyer patches) and a superimposed infection. Associated complications include perforation with pneumoperitoneum and periappendiceal abscess formation. Treatment is surgical resection, if the lesion is not perforated or is minimally perforated, and percutaneous drainage if a well-formed abscess develops in the setting of perforation. In certain patient populations, such as pregnant and pediatric patients, ultrasound is a preferred initial imaging modality in suspected appendicitis to avoid irradiation.
A. As above, the pericecal fat is abnormal in density.
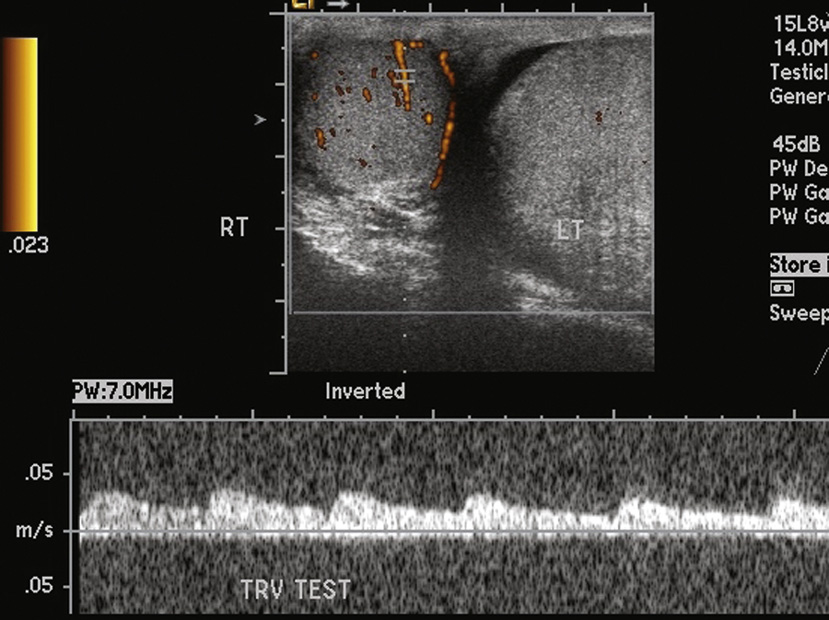
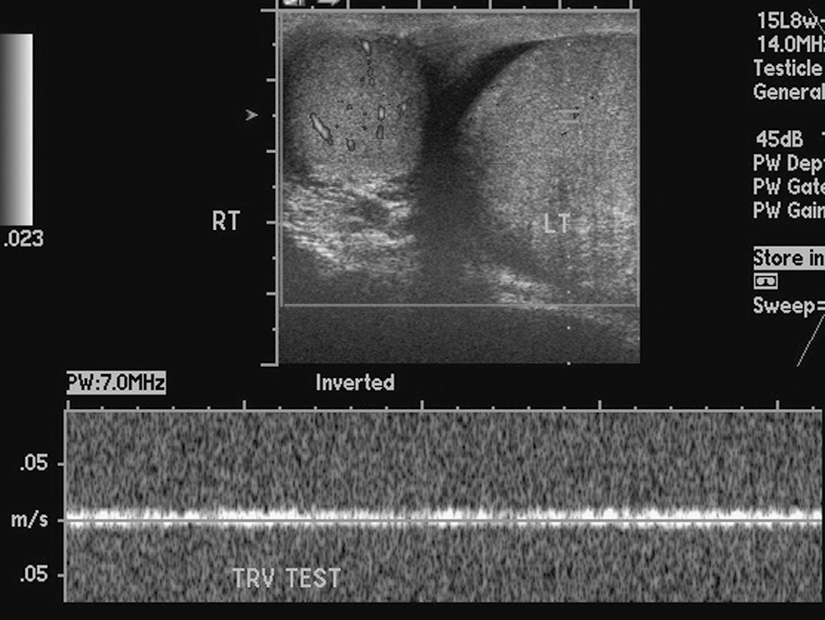
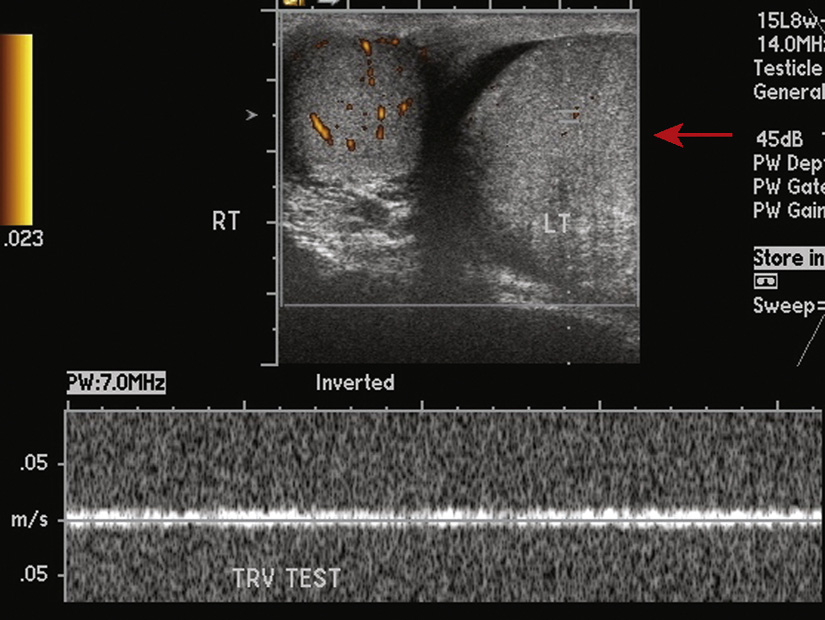
5. A 14-year-old boy presents to the emergency department with severe left scrotal pain. While he had been experiencing pain off and on for about a week, the pain is now much worse and has been constant for about 3 hours. An ultrasound is ordered. Which of the following statements is true?
A. Both testes are symmetric in size.
C. The sonographic findings are suggestive of neoplasm.
E. No further imaging is necessary.
5. The answer is E: No further imaging is necessary. The sonographic images are diagnostic of left testicular torsion, and no further imaging should delay prompt intervention. The left testicle is markedly larger than the right, and there is no blood flow demonstrated on both power and spectral Doppler analysis (arrows).
Testicular torsion occurs when the testis and spermatic cord twist, either spontaneously or secondary to trauma, causing the vascular pedicle to twist as well and resulting in vascular compromise. Viability of the testis depends on the degree of torsion and the time of onset of pain to intervention, with an 80% chance of salvage within 6 hours and a 0% chance after 12 hours. There is a bimodal peak age of incidence in infants and adolescents. Up to 50% of patients report a history of similar symptoms resolving spontaneously.
A. The left testicle is markedly larger than the right.
B. There is no blood flow demonstrated on both power and spectral Doppler analysis.
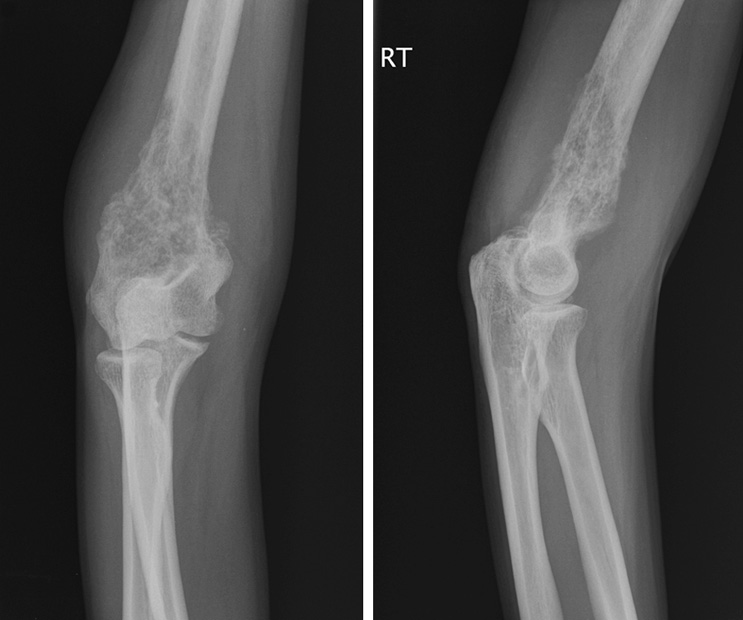
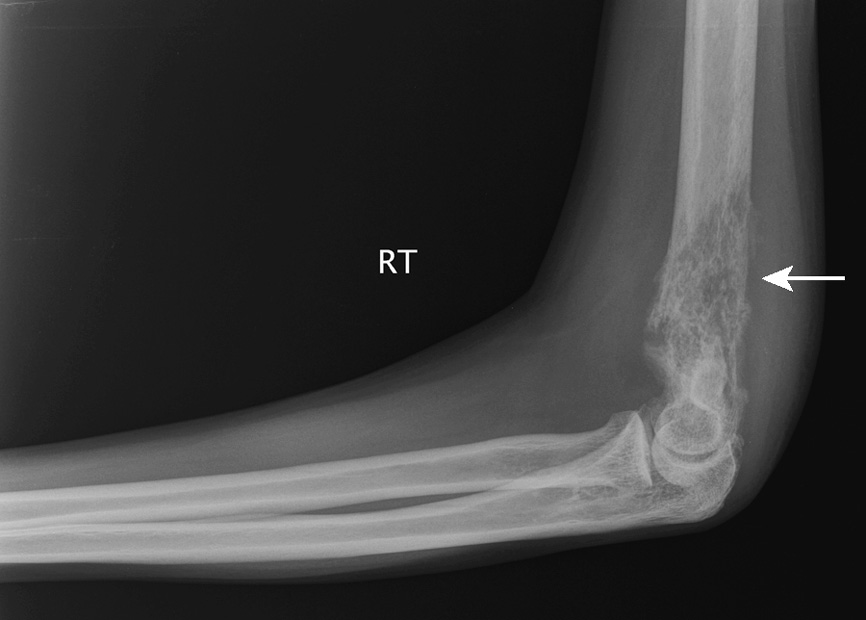
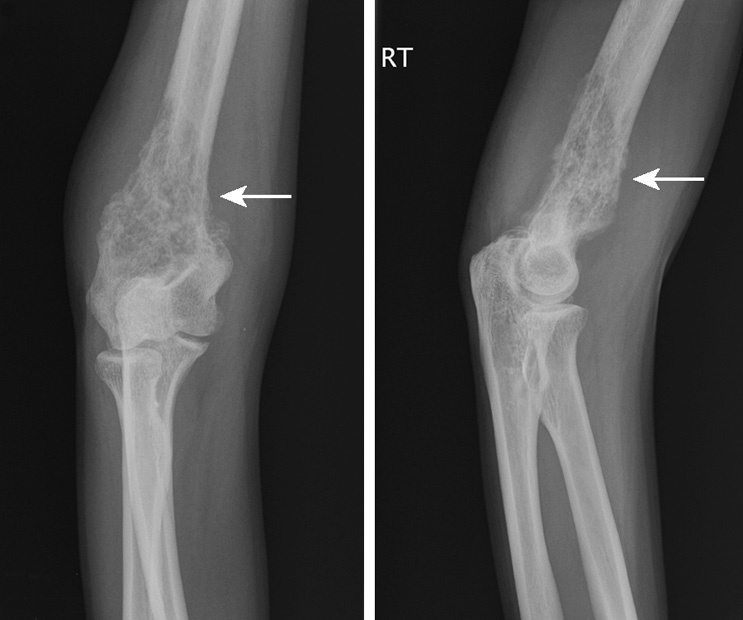
C. There is no neoplasm by sonographic findings.
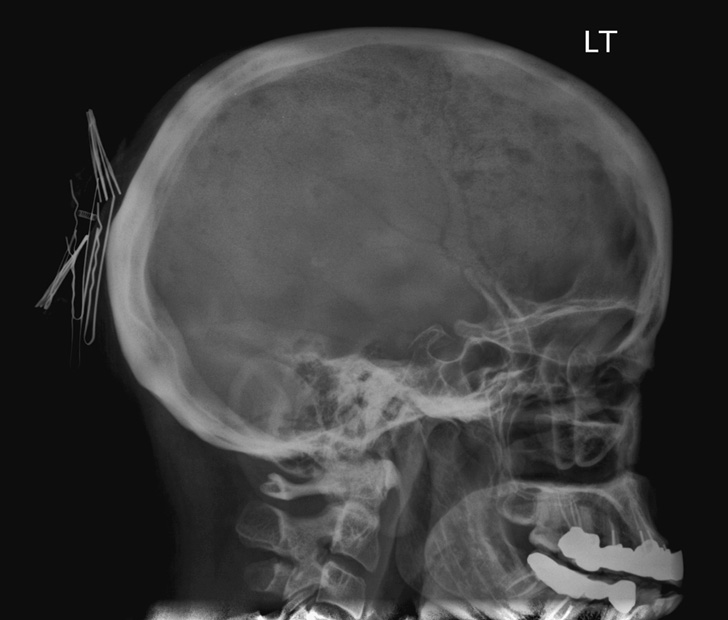
6. A 60-year-old woman presents to her primary care physician with complaints of intermittent mild bone pain, especially in the back. She has lost weight since her last visit. She is found to be mildly anemic and to have mild renal insufficiency on laboratory tests. Further testing of the patient’s urine reveals the presence of Bence Jones proteins. She is sent for magnetic resonance imaging (MRI) of the spine. She informs the MRI technologist that she long ago had a piece of metal stuck in her eye after a car accident. A lateral radiograph of the skull is performed to evaluate for metallic foreign body in the orbits prior to the MRI. Which of the following statements is true?
A. The patient likely has elevated serum calcium.
B. There is intraorbital metal, an absolute contraindication to an MRI.
E. The patient’s prognosis is favorable.
Myeloma Involving the Calvarium
6. The answer is A: The patient likely has elevated serum calcium. The lateral radiograph of the skull shows multiple, well-defined, lytic lesions throughout the calvarium (red arrows), with a “punched-out” appearance, which, especially with the clinical information provided, are highly likely due to myeloma. There are multiple lesions; therefore the stage of the disease is more likely to be advanced, and the patient likely has elevated serum calcium due to the osseous destruction. Myeloma is a monoclonal plasma cell malignancy arising from the bone marrow. Myeloma is the most common primary bone neoplasm. Common sites of involvement of myeloma include the spine, ribs, pelvis, skull, femur, and humerus. Myeloma is primarily treated with chemotherapy.
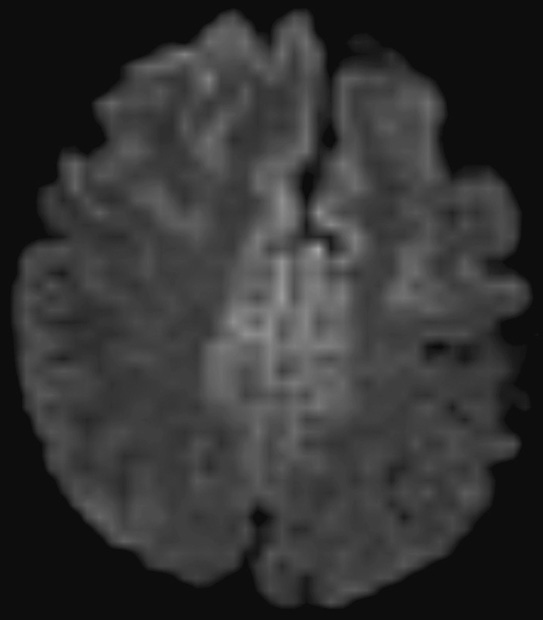
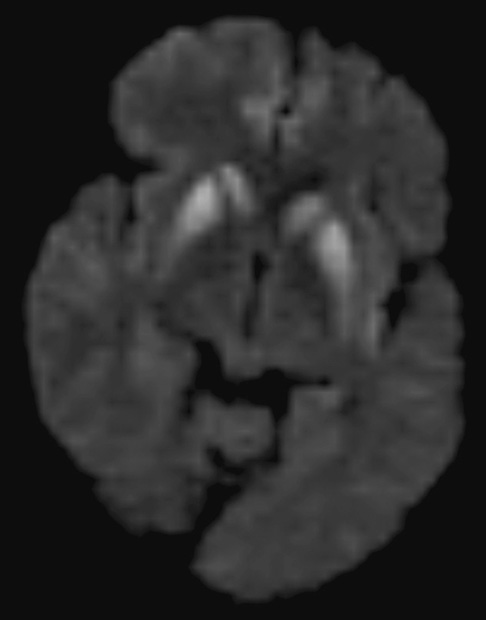
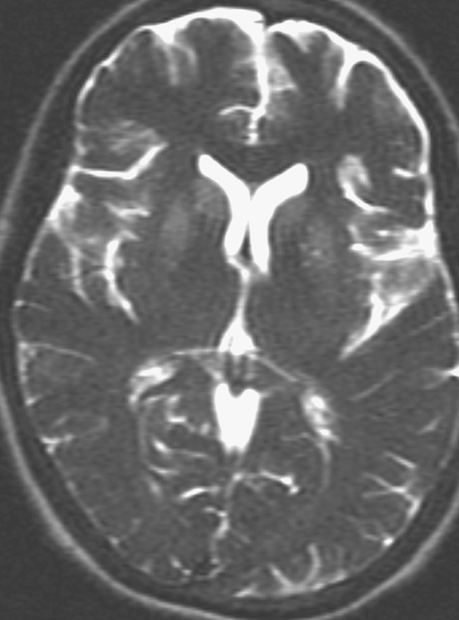
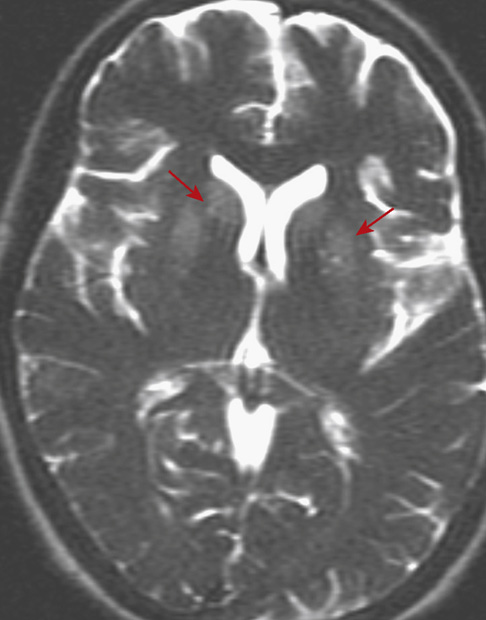
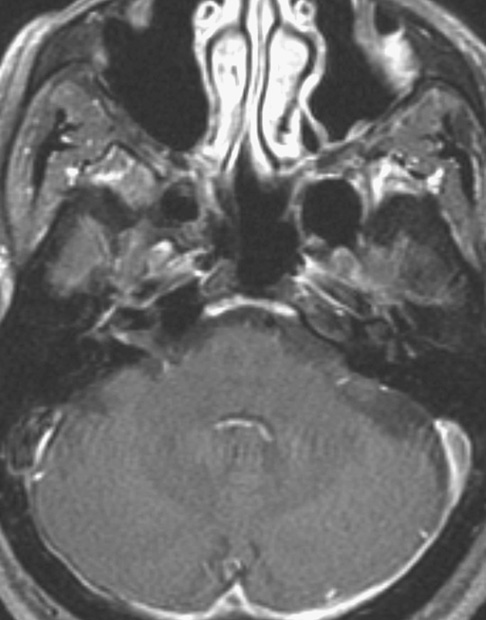
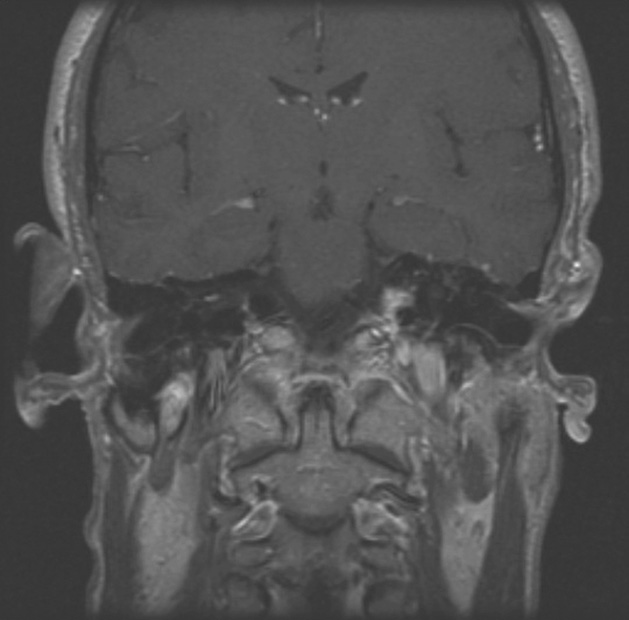
7. A 48-year-old man presented to his primary care physician with a 6-month history of gradually increased awareness of sudden random muscular jerking. His wife reports that his thinking seems to be more clouded and there are personality changes. The MRI demonstrated symmetric signal abnormality within the cerebral cortex, caudate heads, and putamen on the T2 and diffusion-weighted images.The most likely diagnosis is:
C. Creutzfeldt-Jakob disease (CJD)
Creutzfeldt-Jakob Disease (CJD)
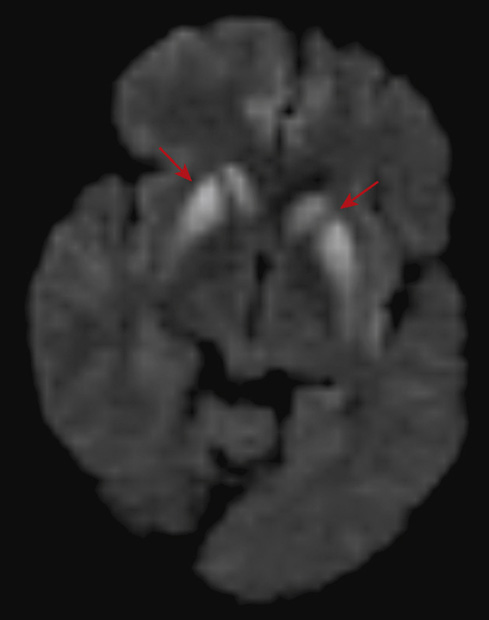
7. The answer is C: Creutzfeldt-Jakob disease (CJD). The pattern of hyperintense signal on T2 (first figure) and diffusion-weighted imaging (second and third figures) within the bilateral putamen and caudate head (straight arrows) as well as the bilateral paramedian gyri (curved arrows) is classic for CJD. The three major categories of CJD are sporadic, hereditary, and acquired. The sporadic form is the most common, accounting for at least 85% of cases. The hereditary form will have a family history of the disease and test positive for a genetic mutation. The acquired form demonstrates several variant subtypes, with variable symptoms and course of the disease. The sporadic and variant types of CJD are more likely to demonstrate signal abnormality within the thalamus, the so-called pulvinar sign.
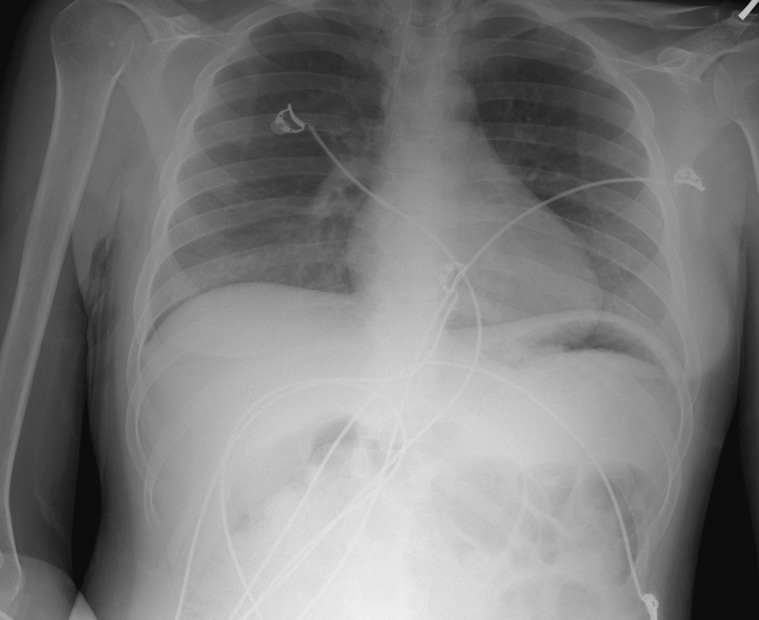
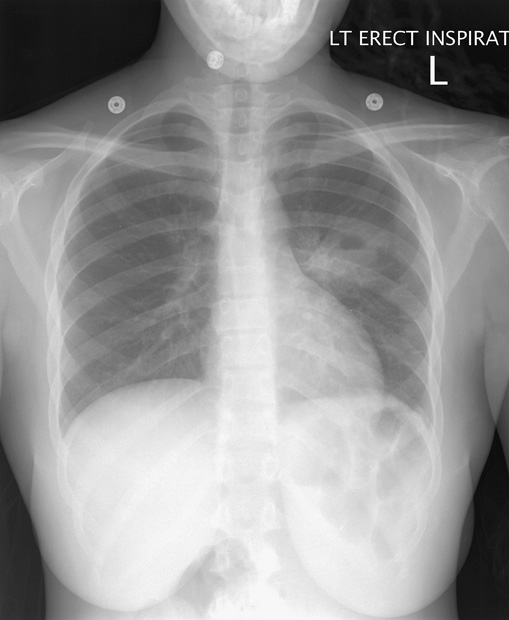
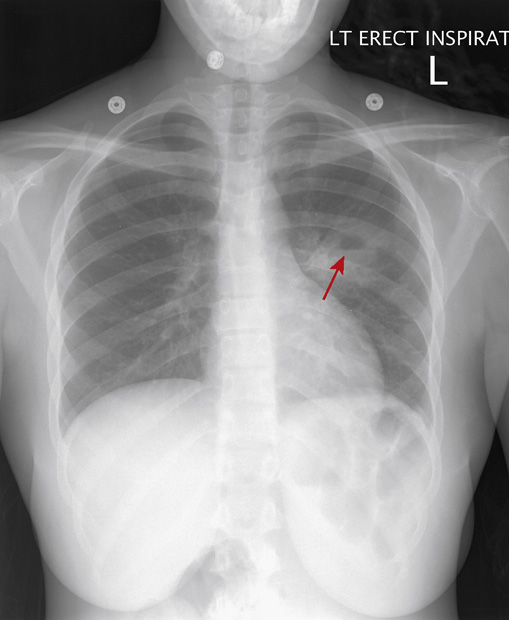
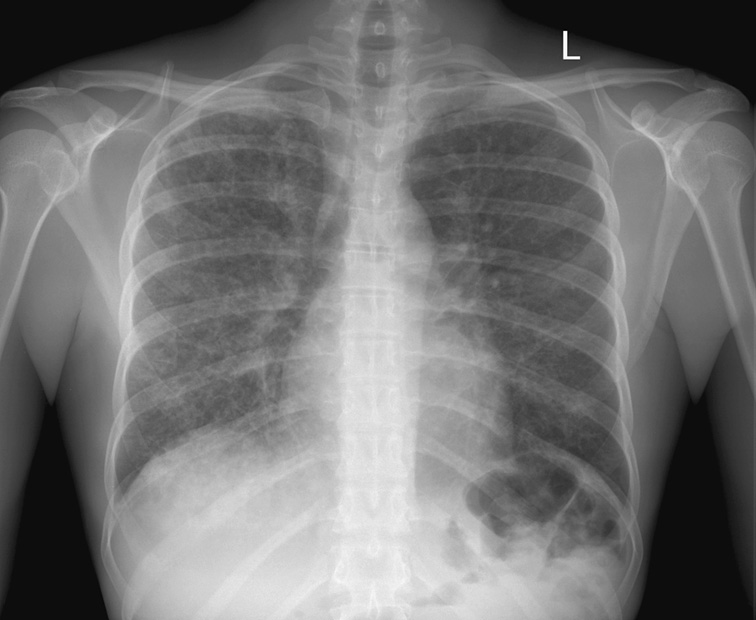
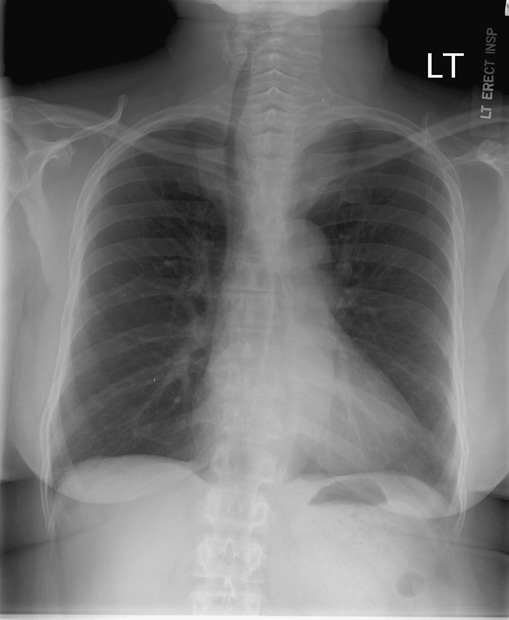
8. An 18-year-old woman presents to the emergency department complaining of chest discomfort. On physical examination, she is mildly tachypneic and tachycardic, with a fever of 101° F. Her past medical history is significant for a seizure disorder. Her chest x-ray is above.
What is the most likely diagnosis?
B. Squamous cell carcinoma of the lung
9. What additional studies are indicated at this time?
B. CT scan of the chest, abdomen, and pelvis
E. Ventilation/perfusion scan of the lungs
8. The answer is C: Lung abscess. The chest x-ray shows a 6-cm masslike structure in the left lung. The mass has typical features of an abscess, including an area of central cavitation with an air-fluid level (arrow). The patient’s underlying seizure disorder puts her at significant risk of aspiration, which was the cause of this infection.
A, B, E. The differential diagnosis of cavitary lung masses also includes fungal infections, squamous cell tumors, and Wegener granulomatosis, among other less likely etiologies. However, the patient’s profile, including her young age and her history of seizure disorder, render these other diagnoses unlikely.
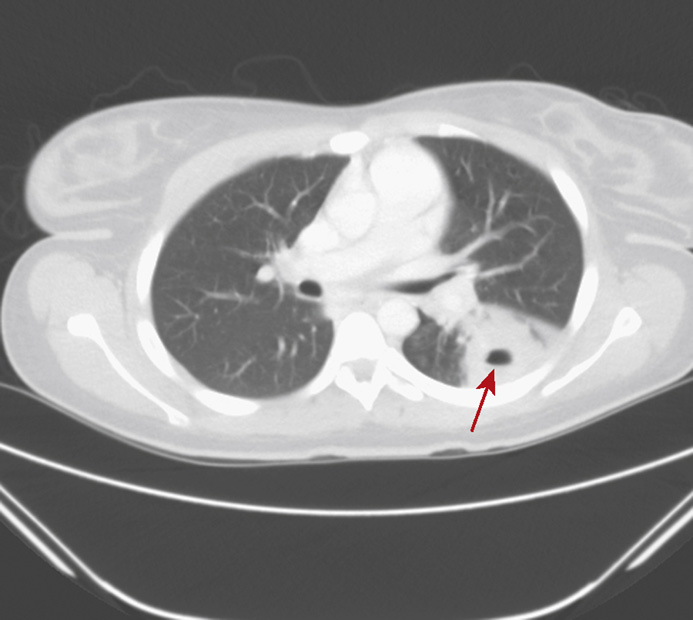
9. The correct answer is A: CT scan of the chest. Chest CT is indicated to confirm the x-ray findings, to evaluate for possible additional abnormalities, and to establish a baseline appearance for follow-up comparison. A representative image from the CT study (above) confirms a large mass with central necrosis and air-fluid level (arrow) in the superior segment of the left lower lung. No additional abscesses are present.
B, D. There is no indication to perform additional imaging of the abdomen, pelvis, or brain at this time.

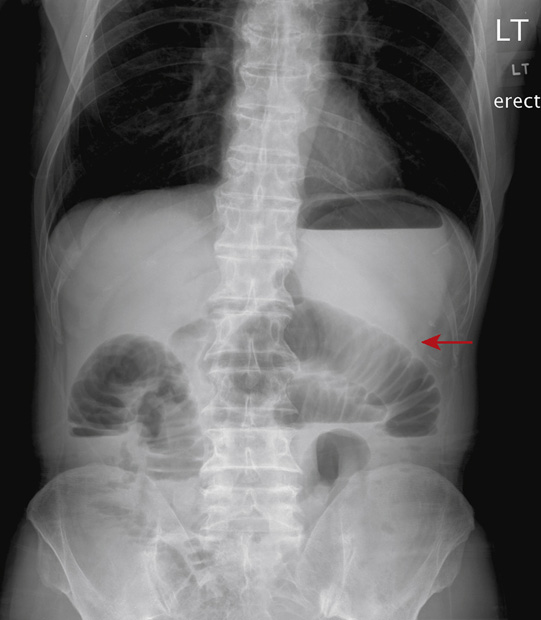
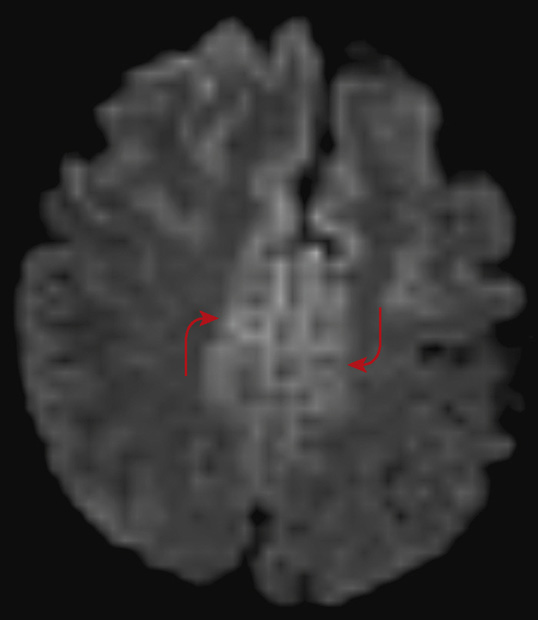
10. A 50-year-old man presents to the emergency department with abdominal bloating, nausea, vomiting, and no bowel movement in 4 days. Past surgical history is significant for appendectomy as a young adult. On physical exam, the abdomen is distended, and there is a paucity of bowel sounds, but there is no rebound tenderness. The patient’s vital signs are stable and laboratory tests are normal. While waiting for a surgical consult, abdominal radiographs are performed. Which of the following statements is correct?
A. There is a large bowel obstruction.
B. There is a small bowel obstruction.
C. There are signs of vascular compromise.
D. CT of the abdomen is unnecessary.
E. Tumor is the most likely etiology.
10. The answer is B: There is a small bowel obstruction. The patient presents with symptoms concerning for bowel obstruction. The radiographs are supportive of a high-grade small bowel obstruction. The colon is not visualized, and the dilated loops are clearly small bowel (arrows), as evidenced by the presence of valvulae conniventes.
Radiographic findings supportive of small bowel obstruction include dilated small bowel loops, presence of valvulae conniventes, multiple air-fluid levels on erect or decubitus views, and a relative absence of air and stool throughout the large bowel. The first course of action should be decompression via placement of a nasogastric tube. Given the fluid-filled stomach, the patient will very much appreciate this procedure. Complications of small bowel obstruction include bowel strangulation, perforation, and sepsis. Prognosis of an uncomplicated obstruction is good. A trial of conservative management with bowel rest, decompression, and hydration may prove helpful in low grade obstructions.
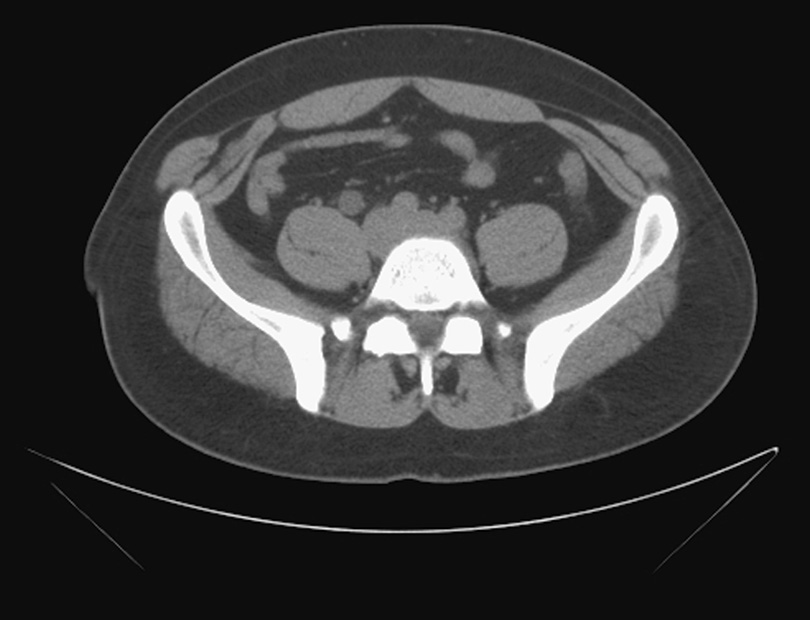

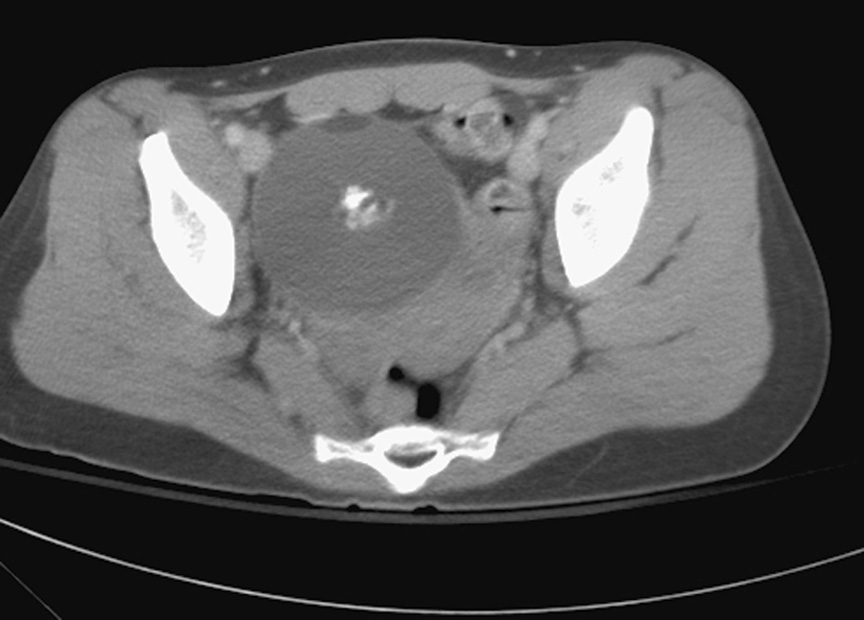
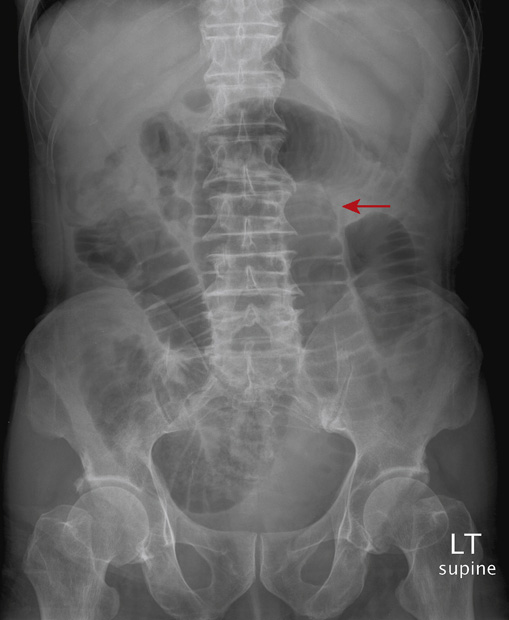
11. A 23-year-old man presents to the emergency department with severe colicky right flank pain, which radiates to the groin. He is afebrile, and his vital signs are stable. A urinalysis reveals hematuria. A CT of the abdomen (above) and pelvis (p. 196) is obtained. Which of the following statements is true?
A. Intravenous (IV) contrast should have been administered.
B. The cause of pain is most likely musculoskeletal in origin.
C. This disease process is more common in women.
D. Radiographs are considered sufficient to make this diagnosis.
E. There is obstructive uropathy on the right.
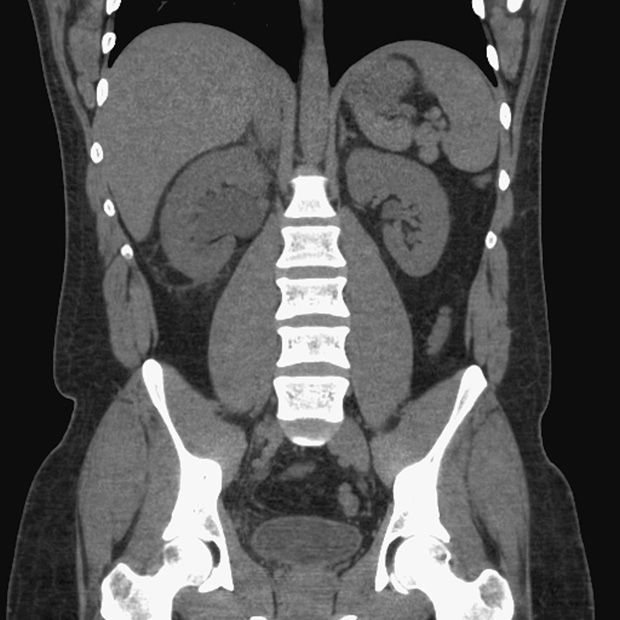

Obstructive Urolithiasis (additional figures on p. 198)
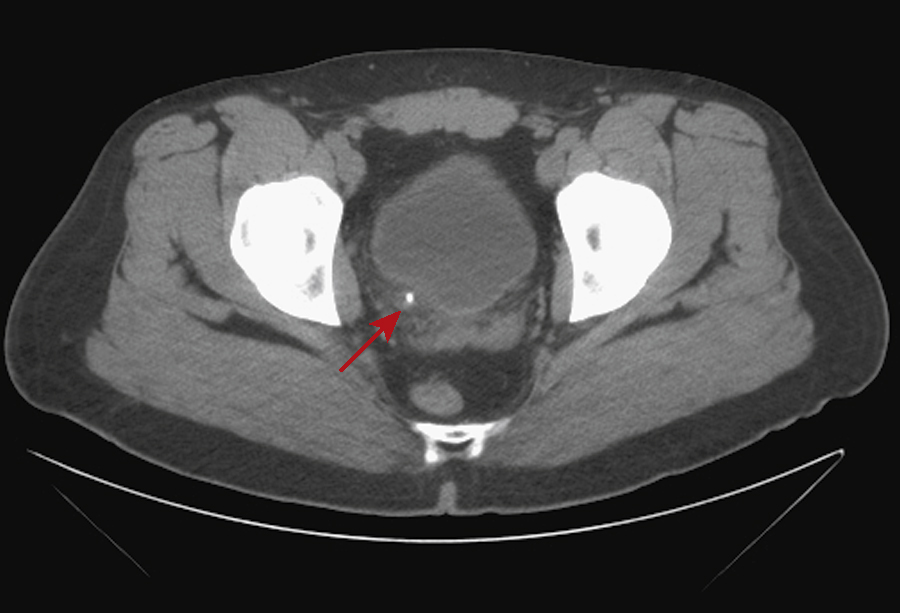
11. The answer is E: There is obstructive uropathy on the right. The CT images provided demonstrate an obstructing calculus in the right ureterovesicular junction (red arrow), under 10 mm in size. There is resulting hydroureter (blue arrow), hydronephrosis (yellow arrow), enlargement of the right kidney, and right perinephric fat standing.
Urolithiasis should be considered very likely in patients who present with acute colicky flank pain that radiates to the groin. Distal ureteral calculi less than 10 mm in size can pass spontaneously. Ultrasound is the preferred initial imaging test in suspected urolithiasis in pregnant patients. In the absence of complications such as renal failure, anuria, or urosepsis, hydration and analgesia with oral pain medications is usually the initial treatment in patients with small stones.
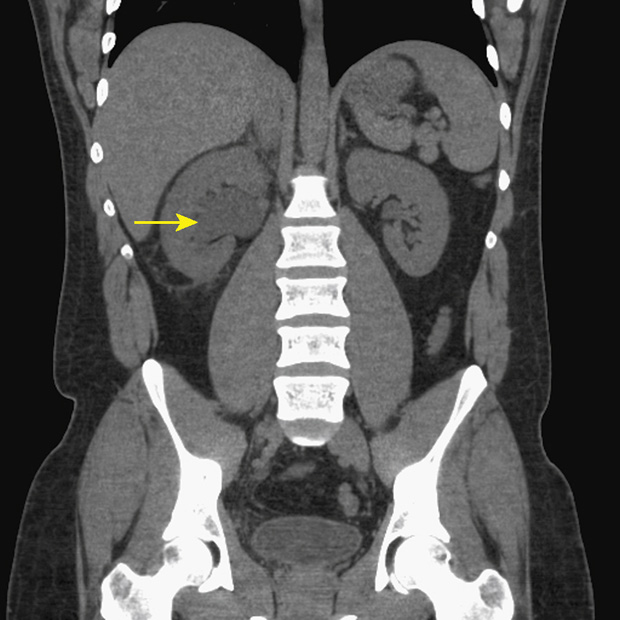
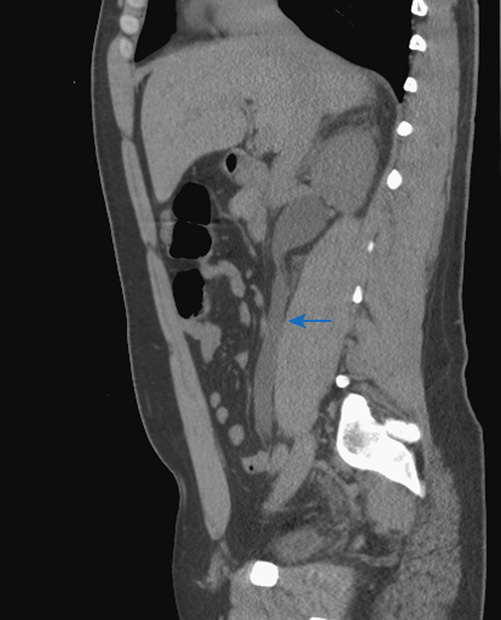
C. Urolithiasis is three times more common in men.
12. A 65-year-old woman presents to her primary care physician after tripping in her driveway and is complaining of left wrist pain and swelling. She is referred to the local imaging center for radiographs of the left wrist, and she returns to her doctor with one radiograph from the study. Which of the following statements is true?
A. No other radiographic views are necessary in this case.
B. This is not the expected location of injury, given the patient’s age.
C. When the patient fell, she likely landed on the palm of her dorsiflexed hand.
D. Most of these injuries require surgery.
E. An underlying advanced inflammatory arthropathy predisposed the patient to this injury.
12. The answer is C: When the patient fell, she likely landed on the palm of her dorsiflexed hand. This patient has suffered a fracture of her left distal radius (red arrow). The single posteroanterior (PA) radiograph shows the comminuted impacted fracture, which has an intraarticular component extending to the radiocarpal joint.
In people approximately 40 years old and older, the most common fracture at the wrist that results from a “fall on an outstretched hand” (FOOSH) when the hand is dorsiflexed is the distal radial fracture. There are many types of distal radial fractures, the majority given eponyms, and the most common being the Colles fracture, in which there is a transverse fracture through the distal radius and apex volar angulation. Colles fractures tend to occur in osteoporotic bone. Distal radial fractures are largely due to axial compression with variable tensile forces, especially in the setting of FOOSH.
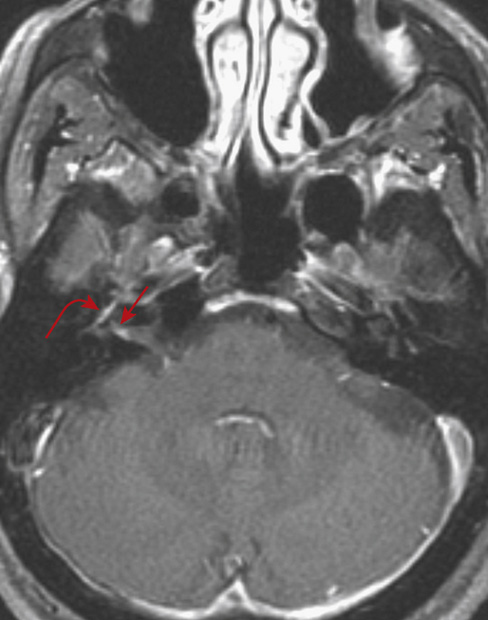
13. A 47-year-old woman presented to her primary care physician’s office with a 2-week history of increasing weakness of her right face and noticed yesterday that she could not fully close her eyelid. Imaging was obtained. The most likely etiology for the patient’s symptoms is:
B. Bell palsy (facial neuritis)
D. Acute erosive otomastoiditis
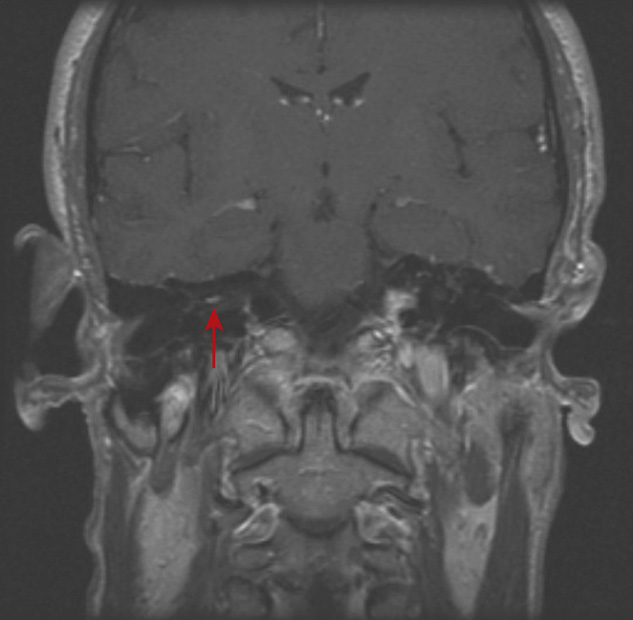
13. The answer is B: Bell palsy (facial neuritis). Postcontrast T1-weighted imaging demonstrated enhancement of the right facial nerve that included the tympanic segment and geniculate ganglion (curved arrow) with extension into the internal auditory canal (IAC) (straight arrows). The facial nerve is broken down into anatomic segments: the meatal segment is from the brain stem to the IAC; the labyrinthine segment is from the fundus of the IAC to facial hiatus; the tympanic segment is from the geniculate ganglion to the pyramidal eminence; the mastoid segment is from the pyramidal process to the stylomastoid foramen; and the extratemporal segment is from the stylomastoid foramen to the pes anserinus.
The facial nerve may demonstrate mild enhancement normally up to and within the geniculate ganglion and tympanic segment, but enhancement should never extend more proximally through to the labyrinthine segment and into the IAC. The appearance of thin wispy enhancement extending into the fundus of the IAC is consistent with Bell palsy.
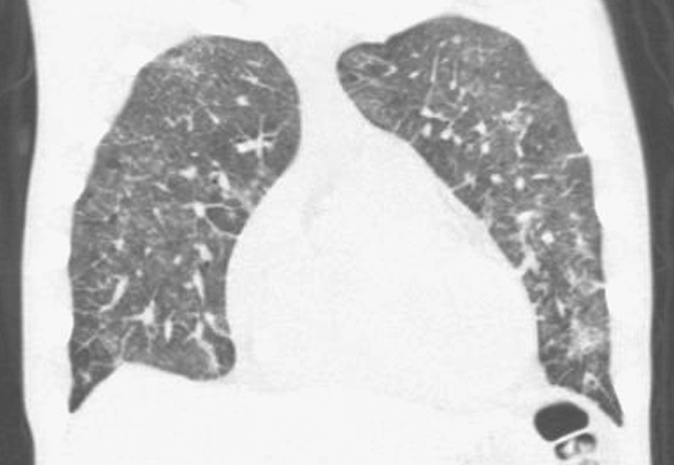
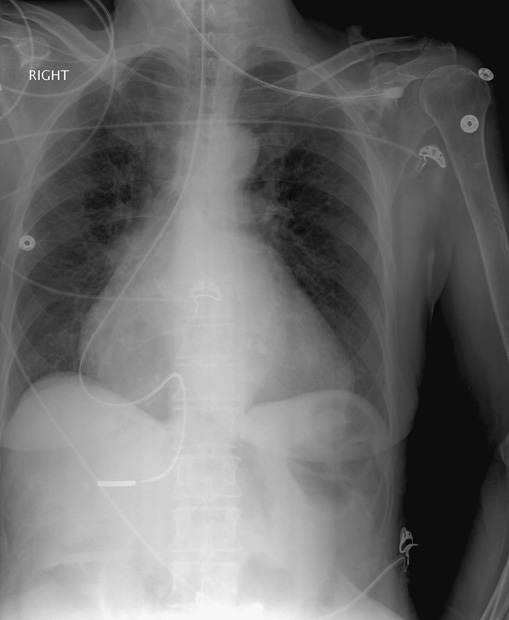
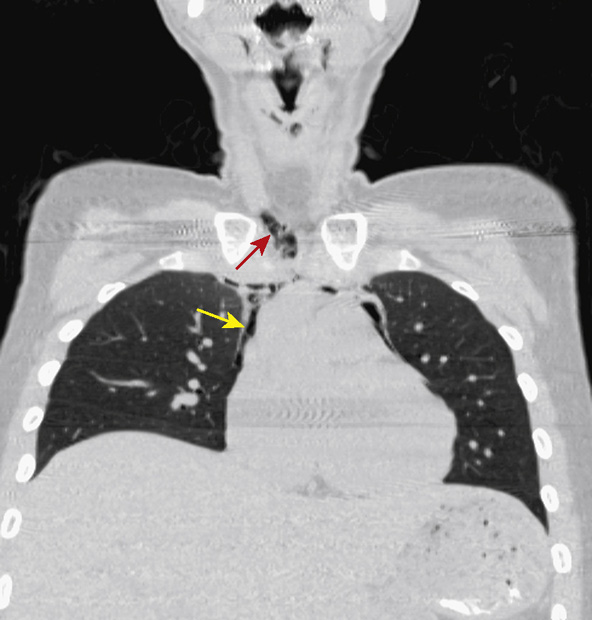
14. A 23-year-old man presents to the emergency department with symptoms of malaise, dry cough, and dyspnea for several weeks. Physical examination reveals tachypnea, tachycardia, and fever, with crackles on auscultation. On further questioning, the patient admits to IV drug abuse. The chest x-ray findings (top) prompt the clinician to order a chest CT study, from which is a representative section in the coronal plane is shown in the bottom figure.
What is the most likely diagnosis?
A. Pneumocystis pneumonia (PCP)
D. Cytomegalovirus (CMV) pneumonia
Human Immunodeficiency Virus Pneumocystis Pneumonia (HIV PCP)
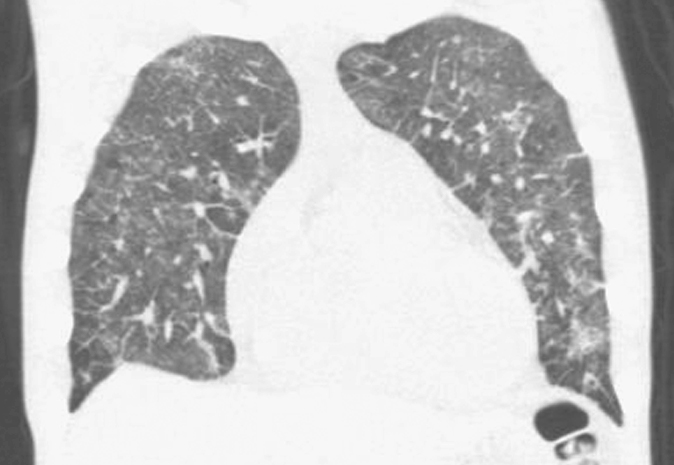
14. The answer is A: Pneumocystis pneumonia (PCP). The chest x-ray and chest CT show a diffuse ground-glass pattern throughout the lungs. The term ground-glass refers to the edge of a microscope slide that can be written on with pencil, and it means that although the area remains transparent, one cannot see detail through it. This pattern is characteristic of pneumocystis pneumonia, commonly known as PCP. The patient tested positive for HIV infection, likely acquired through the sharing of contaminated needles, and he is severely immunosuppressed. Sputum obtained during bronchoalveolar lavage was positive for PCP.
PCP is caused by Pneumocystis jirovecii, an endemic fungus that is harmless to immunocompetent individuals, but it is the most common cause of opportunistic infection in patients with HIV, typically occurring when CD4 counts fall below 200/μL. Although the organism is classified as a fungus, treatment is with antibiotics, trimethoprim-sulfamethoxazole, for 21 days. Despite antibiotic treatment, mortality rates range between 10% and 20%.
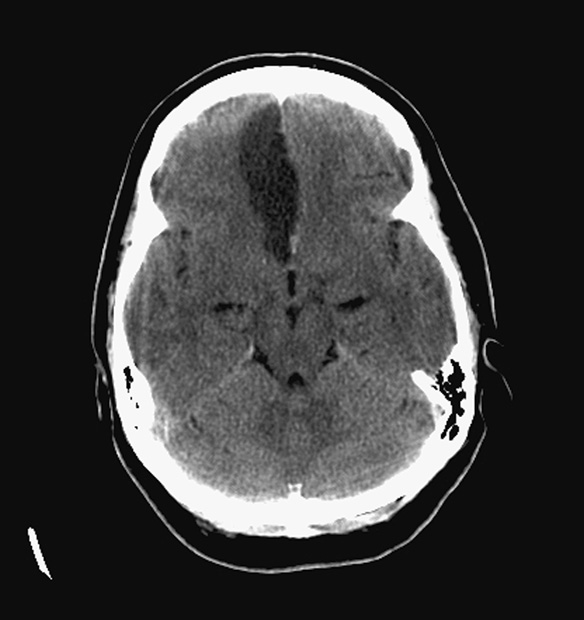
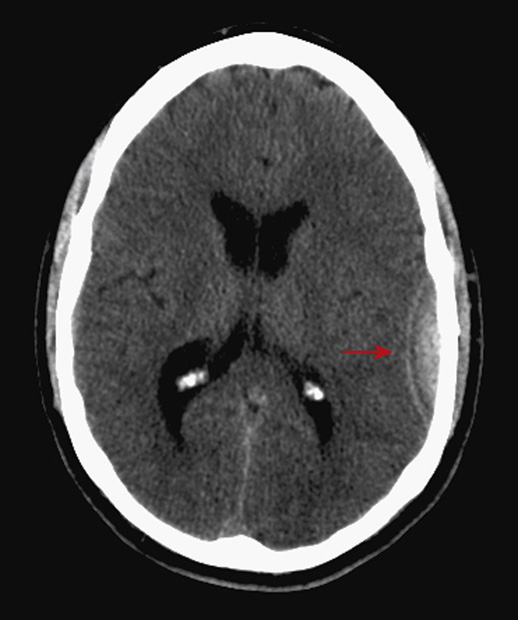
15. A 33-year-old woman presents to the emergency department with altered mental status and severe headache following a minor motor vehicle accident (MVA) in which she was the driver. The patient has no memory of the incident. The CT scan is above. The most likely explanation of the above finding is:
A. Posttraumatic subdural hemorrhage
B. Posttraumatic subarachnoid hemorrhage
C. Incidental calcification within the subarachnoid space
D. Subarachnoid hemorrhage (SAH) secondary to rupture of an aneurysm
15. The answer is D: Subarachnoid hemorrhage (SAH) secondary to rupture of an aneurysm. The appearance is consistent with hemorrhage in the subarachnoid space (arrow). The distribution within the left sylvian fissure points to a ruptured aneurysm involving the left MCA region. CT angiography (CTA) or direct angiography should be performed urgently to identify the location of the aneurysm and treat it with either angiographically directed coiling or placement of a vascular clip.
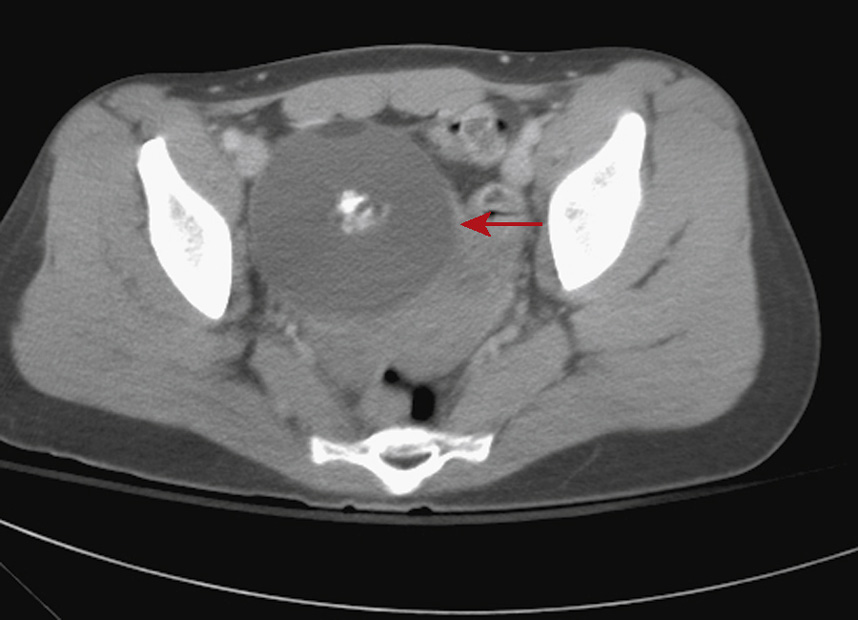
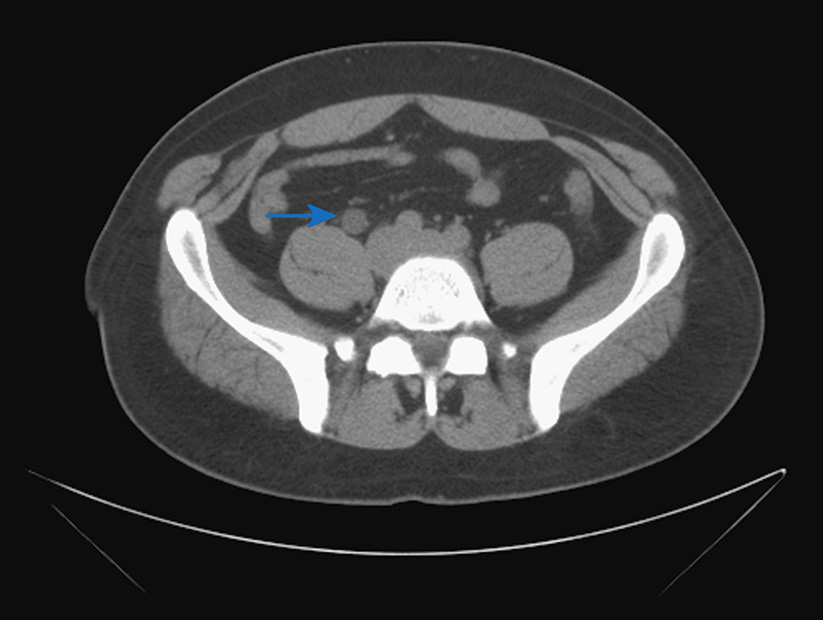
16. A 25-year-old woman is involved in a low-speed MVA and is taken to the emergency department. She is found to be stable, but is complaining of diffuse abdominal pain, and therefore a CT of the abdomen is obtained. Which of the following statements regarding the image provided is true?
A. There is active hemorrhage in the pelvis.
B. If left untreated, the salient abnormality can result in severe complications.
C. There is no malignant potential of the identified abnormality.
D. This abnormality has developed acutely.
E. This abnormality is found only in the pelvis.
16. The answer is B: If left untreated, the significant pelvic abnormality can result in severe complications. The CT image provided demonstrates a round mass in the right hemipelvis, composed of central calcification, surrounding soft tissue, and less dense fat layering anteriorly (arrow). These findings are diagnostic of an ovarian teratoma. Despite being currently asymptomatic, this teratoma could potentially rupture, causing a chemical peritonitis and/or adhesions, act as a lead point in ovarian torsion, cause infertility due to mass effect on the fallopian tube or uterus, or rarely degenerate into a malignant teratoma, necessitating surgical resection with hope to preserve the ovary.
A mature ovarian teratoma is a benign neoplasm developing from at least two of the three primordial germ layers. Teratomas are the most common ovarian neoplasms in women younger than 20 years old. Ovarian teratomas can be bilateral in up to 15% of patients. Ultrasound, CT, and MRI are all potentially useful modalities in distinguishing teratomas from other ovarian neoplasms.
A. There is no evidence of hemorrhage on the image provided.
C. An ovarian teratoma may degenerate into a malignant teratoma, though it is rare.
D. This teratoma was likely present in this patient since birth, albeit smaller at that time.
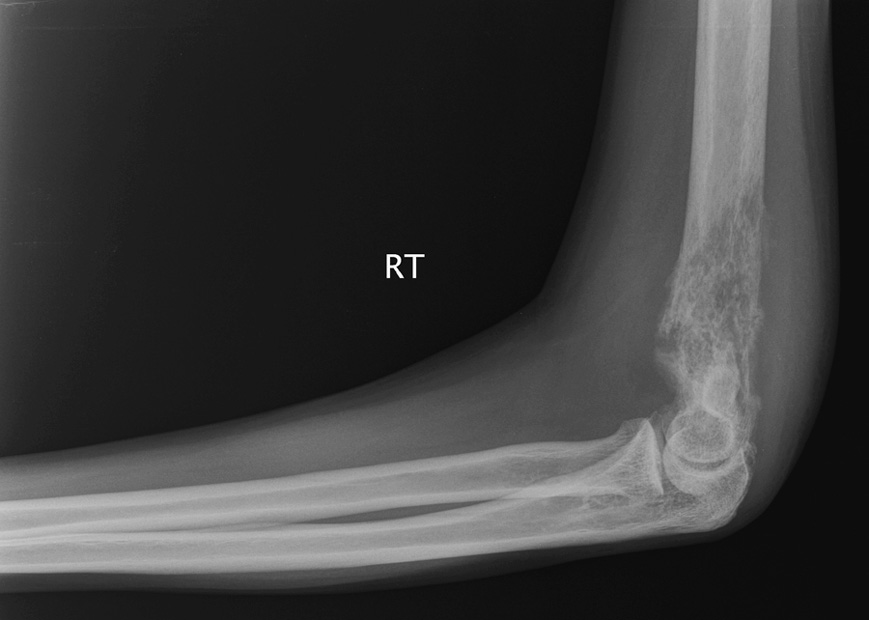
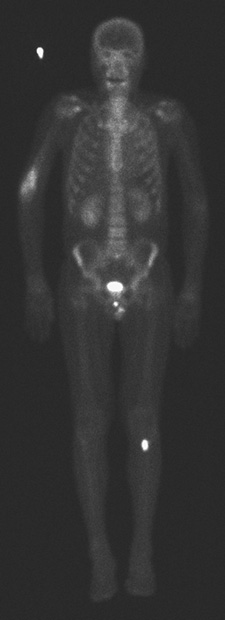
17. A 55-year-old woman with a history of breast cancer is found to have an elevated alkaline phosphatase on recent blood work and is sent for a bone scan. Based on the findings of the bone scan, radiographs are obtained. Based on the images provided, which of the following statements is true?
A. There is a solitary suspicious finding on the bone scan.
B. The radiographs are most compatible with an old healed fracture.
C. Bone scans are a sensitive modality for breast carcinoma metastases.
D. There is abnormal activity in the pelvis on the bone scan.
E. The findings on the bone scan and radiographs are disconcordant.
Lytic Bone Metastasis in Breast Cancer
17. The answer is C: Bone scans are a sensitive modality for breast carcinoma metastases. The image from the bone scan above shows increased radiotracer uptake in the distal right humerus as well as in the proximal left tibia (red arrows). Given the history of breast cancer and an elevated alkaline phosphatase, these foci are very concerning for metastases. Bone scans are very sensitive for osseous metastases, particularly osteoblastic metastases, and are used as screening tools in patients with certain cancers, such as breast, prostate, and lung.
Breast cancer commonly metastasizes to bone, and can be either osteoblastic or osteolytic in nature. The 10-year survival rate of stage IV (metastatic) breast cancer is approximately 10%. In patients with suspicious findings on a bone scan screening for metastases, radiographs and, if necessary, MRI are appropriate imaging studies for further evaluation. Bone scans are very useful in monitoring response to therapy in widespread metastatic disease to the bone.
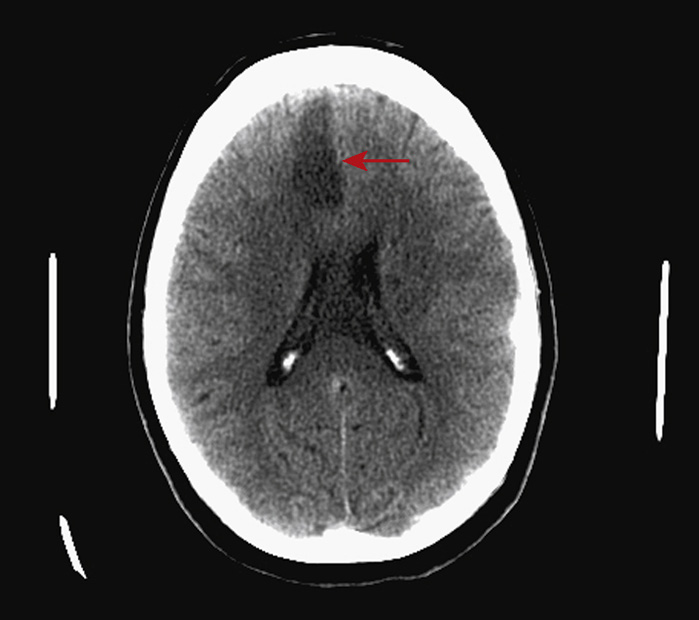
18. A 25-year-old man presents to the emergency department with a history of elbow to the head during a basketball game. He lost consciousness for a few minutes. Upon regaining consciousness, he was alert and oriented, complaining of a headache. By the time he arrived via ambulance, he complained of severe headache and was vomiting. A CT scan of the head was ordered and demonstrated the above findings. There is a hyperdense, biconvex collection in the left parietal region with a subtle, nondisplaced fracture of the left parietal bone.
The appearance above is most consistent with:
B. A subacute to chronic subdural hematoma
18. The answer is C: An acute epidural hematoma. The history of trauma causing loss of consciousness with a lucid interval followed by a rapid deterioration in his clinical course is typical. Epidural hematoma (straight arrow) is usually caused by focal trauma to the temporoparietal region resulting in a fracture and tearing of the middle meningeal artery or one of its dural branches. On CT, the blood is hyperdense, lenticular, or biconvex in shape and does not cross suture lines. There is almost always a fracture associated with it, as in this case (curved arrow). It is a surgical emergency and, if untreated, is associated with a high mortality rate.

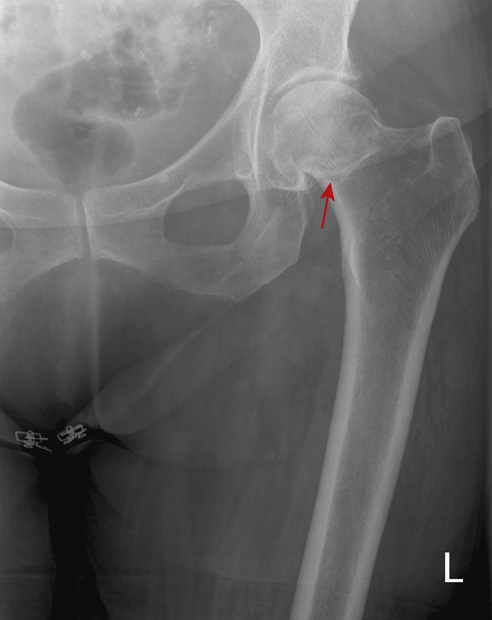
19. A 70-year-old woman suffers a fall at home and is brought to the emergency department by a neighbor. She is unable to walk and complains of pain in her left hip. Radiographs are obtained while she is in the waiting room. Which of the following statements is true?
A. This injury is the least common at this anatomic location.
B. This injury is often related to overuse.
C. There is a pathologic fracture.
D. There is an increased risk of avascular necrosis secondary to this injury.
E. This injury does not require surgery.
Subcapital Femoral Neck Fracture

19. The answer is D: There is an increased risk of avascular necrosis secondary to this injury. This patient has suffered a displaced impacted subcapital fracture of the left femoral neck (red arrows). Femoral neck fractures are intracapsular with an increased risk of avascular necrosis from potential disruption of blood supply to the femoral head.
Femoral neck fractures are commonly sustained by elderly people, often related to seemingly mild falls. The propensity for the hip to flex and internally rotate when the femoral neck is fractured can obscure subtle fracture lines on radiographs. If a fracture is suspected and radiographs are negative, MR is the next most appropriate imaging study to perform. CT is much less sensitive for nondisplaced femoral neck fractures, usually because of the underlying osteoporotic bone. Even with surgical fixation, the prognosis may be poor due to comorbidities such as venous thromboembolic disease and pneumonia.
E. The treatment for this fracture is internal fixation.

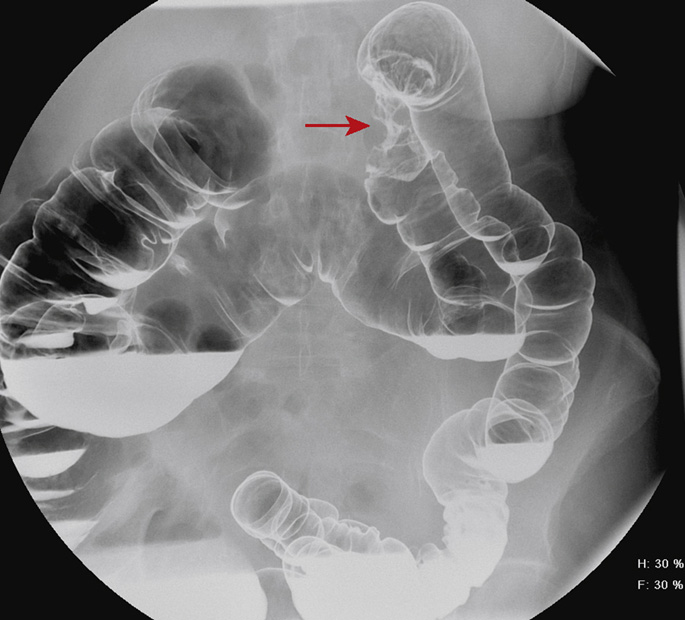
20. A 60-year-old woman presents to her primary care physician with weight loss and iron deficiency anemia. Fecal occult blood tests are positive. A double-contrast barium enema is performed for further evaluation. Which of the following statements is true regarding this disease?
A. Common risk factors include a high-fiber, low-fat, and animal protein diet, inflammatory bowel disease, and a positive family history.
B. This location is the most common site for this entity.
C. The treatment requires surgical resection, possibly with adjuvant chemotherapy.
D. These lesions are not associated with benign polyps.
E. This condition does not usually present with obstruction.
Advanced Colon Carcinoma—Annular Constricting Lesion (i.e., Apple Core Lesion)
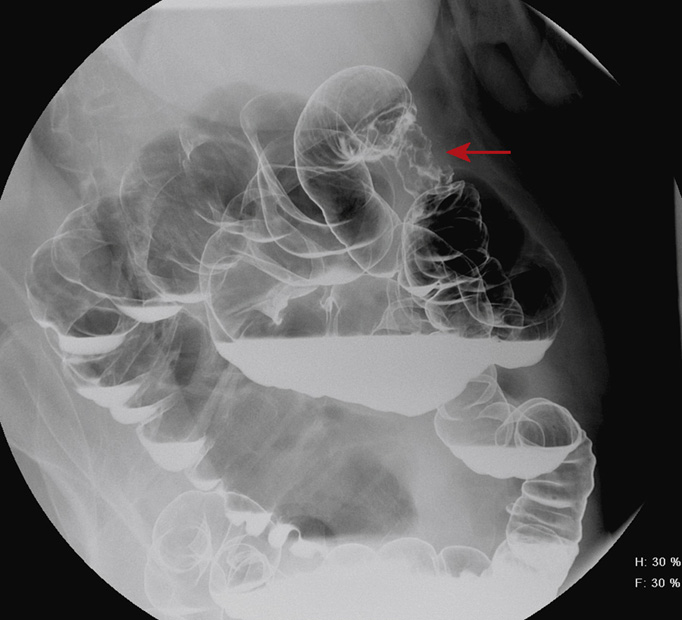
20. The answer is C: The treatment requires surgical resection, possibly with adjuvant chemotherapy. This vignette describes a classic presentation of colon cancer with the peak age at presentation of 50 to 70 years old and the most common presentations including weight loss, change in bowel habits, melena/hematochezia, and iron deficiency anemia. Colon cancer is the most common GI malignancy and the second most common cause of cancer deaths. Colon cancer can be identified on a barium enema as a sessile plaque, a pedunculated lesion, a large polypoid lesion, a semiannular or saddle-like lesion, an annular or apple core lesion, or wall thickening resembling a carpet-like lesion.
The spot radiographs above demonstrate circumferential narrowing in the distal transverse colon, with shelflike borders, resembling an apple core and representing an advanced annular constricting tumor (arrows). The barium enema has a 90%-95% detection rate for colon cancer, which is comparable with that of both colonoscopy and CT colonography. The advantage to the barium enema over colonoscopy in screening is the noninvasiveness. The advantage of colonoscopy in screening is the ability to remove polyps during the procedure. Both CT of the abdomen and pelvis and whole body positron emission tomography (PET) CT are useful modalities in initial staging of colon cancer, particularly in evaluating for lymph node and liver metastases.
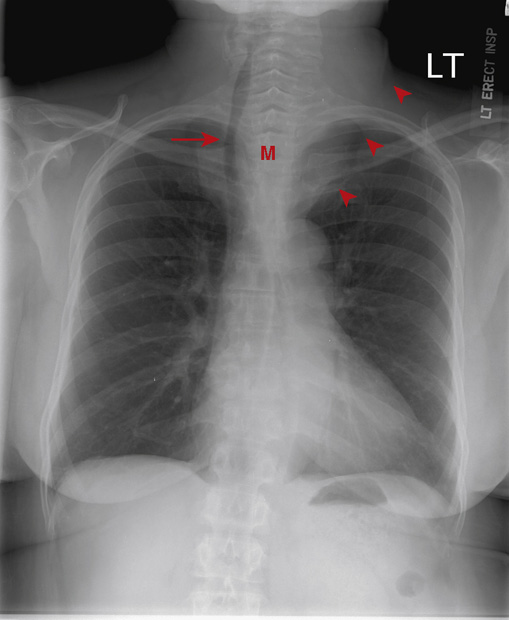
21. An asymptomatic, 50-year-old woman presents for preop testing prior to general anesthesia for knee replacement and has the chest x-ray shown above.
What is the most appropriate next step?
B. CT of the neck and chest with contrast
C. CT of the neck and chest without contrast
E. No additional imaging is needed before knee replacement surgery.
21. The answer is C: CT of the neck and chest without contrast. The next most appropriate step would be CT of the neck and chest without contrast to evaluate a large substernal goiter.
The chest x-ray shows a large mass (M) occupying the superior mediastinum and extending into the neck (arrowheads). The mass displaces the trachea to the right (arrow) and narrows the tracheal lumen along most of its length. The appearance is typical of a large substernal goiter. Further evaluation of the enlarged thyroid and its relationship to the trachea and great vessels is necessary prior to elective surgery under general anesthesia. Ideally the patient should be euthyroid at the time of surgery, so serum thyroid function tests and consultation with an endocrinologist are also indicated.
There are many causes of thyroid goiter, and some of the more common etiologies are detailed below:
▪ The most common cause of goiter worldwide is dietary iodine deficiency. However, the common practice of iodine supplementation in salt makes this a less likely cause in the United States.
▪ Thyroiditis is an inflammatory condition of the thyroid that causes pain and generalized swelling.
▪ Several types of thyroid malignancy occur, but these typically manifest as a solitary, hard nodule rather than as diffuse glandular enlargement. A malignant nodule will appear as a solid nodule on ultrasound that is cold, or nonfunctioning, on I-131 thyroid scanning. CT imaging of malignant lesions may be helpful for evaluation of regional lymph nodes and staging.