SECTION I BREAST IMAGING
Essentials 1
Questions
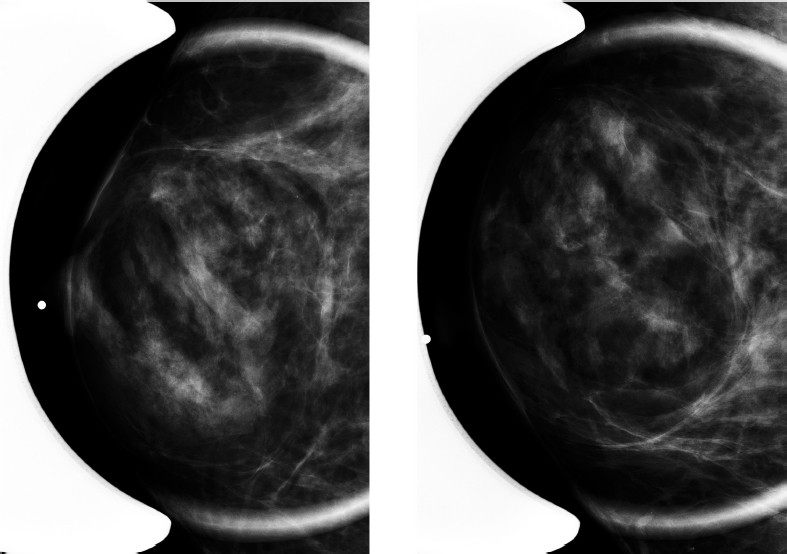
1. Which of the following is the appropriate overall Breast Imaging Reporting and Data System (BI-RADS) category for this screening mammogram?
A. BI-RADS category 0
B. BI-RADS category 1
C. BI-RADS category 2
D. BI-RADS category 3
E. BI-RADS category 4
2. Regarding screening guidelines, which of the following are the current recommendations for screening mammography for the average-risk woman, according to the American Cancer Society in 2015?
A. Annual screening mammography for women aged 45 to 54 years with the option of beginning annual screening between ages 40 to 44. Biennial mammography screening starting at age 55 with the option to continue annual screening.
B. Annual screening mammogram starting at age 40.
C. Annual screening mammogram and whole breast ultrasound starting at age 40.
D. Biennial screening mammography for women aged 50 to 74 years with an individual decision to start screening prior to 50 years old.
E. Alternating biennial screening mammography and breast magnetic resonance imaging starting at age 45.
3. Regarding breast cancer risk factors and high-risk patients, which ONE of the following is correct?
A. Women who are characterized as “high-risk” have a > 30% lifetime risk of developing breast cancer.
B. Women who have had previous chest irradiation between the ages of 10 and 30 years old should begin screening mammography at age 30.
C. Women who have a first-degree relative with breast cancer should begin screening mammography at an age 10 years earlier than the age of the affected relative at time of diagnosis, or between 25 and 30 years old, whichever is later.
D. In women with “dense breasts” as their sole breast cancer risk factor, supplemental screening breast ultrasound and breast magnetic resonance imaging are indicated.
E. In women who have had a previous diagnosis of atypical ductal hyperplasia on excisional biopsy with no other known risk factors, breast magnetic resonance imaging is indicated.
Answers and Explanations
Question 1
A. Correct! BI-RADS category 0. Each BI-RADS category is paired with an assessment and recommendation. There is a mass present in the upper inner quadrant of the right breast, and additional imaging is needed to evaluate this mass. Therefore, this is BI-RADS category 0—additional imaging is needed.
Other choices and discussion
B. BI-RADS category 1 assessment means that there are no abnormalities on the mammogram. It is “negative,” with a management recommendation of routine mammography screening.
C. BI-RADS category 2 assessment means that there is a benign finding (history of excisional biopsy, lumpectomy, bilateral benign masses, etc.), and there are no suspicious abnormalities. The management recommendation is the same as a BI-RADS category 1 assessment.
D. BI-RADS category 3 assessment means that the finding is probably benign (>0% but ≤ 2% likelihood of malignancy). The only BI-RADS categories permitted after a screening exam are 0, 1, and 2. A diagnostic workup needs to be completed before a BI-RADS category 3 can be given.
E. BI-RADS category 4 assessment represents a suspicious abnormality. This category can be rendered after diagnostic workup and should not be used as an assessment on screening mammogram.
Question 2
A. Correct! Annual screening mammography for women aged 45 to 54 years with the option of beginning annual screening between ages 40 and 44. Biennial screening mammography starting at age 55 with the option to continue annual screening. These are the most recent 2015 American Cancer Society recommendations. Women should continue screening as long as they have good overall health and a life expectancy of ≥ 10 years.
Other choices and discussion
B. Annual screening mammogram starting at age 40 is the American College of Radiology and Society of Breast Imaging’s recommendation.
C. There are no guidelines that currently recommend both mammography and whole breast screening ultrasound for the average-risk woman.
D. Biennial screening mammography for women aged 50 to 74 years with an individual decision to start screening prior to 50 years old is the 2016 recommendation from the United States Preventative Services Task Force. The task force also concludes that there is insufficient evidence to assess the balance of benefits and harm for women > 75 years old.
E. Screening breast magnetic resonance imaging is not recommended in women of average risk for breast cancer.
Question 3
C. Correct! Women who have a first-degree relative with breast cancer should begin screening mammography at an age 10 years earlier than the age of the affected relative at time of diagnosis, or between 25 and 30 years old, whichever is later. This is according to the American College of Radiology’s appropriateness criteria.
Other choices and discussion
A. High-risk women include women with a > 20% lifetime risk, BRCA gene mutation carrier, women who has a first-degree relative with a BRCA gene mutation but themselves are untested, history of chest irradiation between ages 10 and 30, and other genetic mutations that lead to an increased incidence of breast cancer such as Li-Fraumeni syndrome.
B. According to the American College of Radiology’s appropriateness criteria, women who have had chest irradiation between the ages of 10 and 30 should begin screening mammography 8 years after radiation therapy, starting the earliest at age 25.
D. Woman with “dense breasts” do have a small increased risk of developing breast cancer compared to those who do not. However, there is currently insufficient evidence for adjunctive screening with other modalities.
E. A diagnosis of atypia (atypical ductal hyperplasia, atypical lobular hyperplasia) by itself does not put a woman at high enough risk to warrant supplemental screening with a breast magnetic resonance imaging.
Suggested Readings
D’Orsi CJ SE, Mendelson EB, Morris EA, et al. ACR BI-RADS® Atlas, Breast Imaging Reporting and Data System. 5th ed. Reston, VA: American College of Radiology Nainiero MB, Lourenco A, Mahoney MC, et al. ACR Appropriateness Criteria® Breast Cancer Screening. Available at https://acsearch.acr.org/docs/70910/Narrative/. American College of Radiology. Accessed February 18, 2016 Oeffinger KC, Fontham EH, Etzioni R, et al. Breast cancer screening for women at average risk: 2015 guideline update from the american cancer society. JAMA 2015;314:1599–1614 Siu AL. Screening for Breast Cancer: U.S. Preventive Services Task Force Recommendation Statement Screening for Breast Cancer. Ann Intern Med 2016;164:279–296Top Tips
On screening mammography, only a BI-RADS category of 0, 1, or 2 can be given.
The current recommendations on when to initiate screening mammography differ between different organizations. In general, all organizations agree that initiation of screening mammography at age 40 saves the most lives; however, there needs to be a balance between the benefits and harms of screening.
According to the American College of Radiology, supplemental screening with bilateral breast MRI is indicated in women with a > 20% lifetime risk of developing breast cancer, BRCA gene mutation carrier and untested first-degree relative, history of chest irradiation between ages 10 and 30, and other genetic mutations that lead to an increased incidence of breast cancer such as Li-Fraumeni syndrome.
Essentials 2
Case
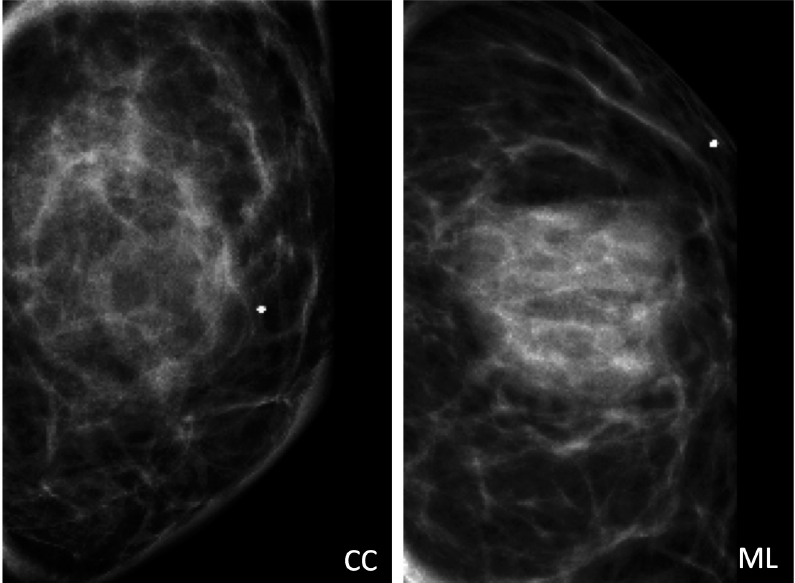
A 52-year-old woman presents with a right breast, subareolar, palpable abnormality. Craniocaudal and mediolateral oblique spot magnification views are shown.
Questions
1. Regarding the imaging findings, which ONE of the following is the best answer?
A. Oval mass with circumscribed margins and complex internal architecture. Recommend targeted ultrasound.
B. A targeted ultrasound would show a complex solid and cystic mass.
C. Biopsy of this lesion will reveal “benign, normal glandular tissue.” This is radiologic-pathologic concordant.
D. On a baseline screening mammogram, this mass would be categorized as BI-RADS category 0—additional imaging is needed.
E. Fat-containing mass. Benign. There is absolutely no risk of cancer development within this lesion.
2. Regarding a fat-containing mass, which ONE of the following is the best answer?
A. Most oval, circumscribed, fat-containing masses on routine screening mammography are benign and require no additional workup.
B. A slowly growing, painful, fat-containing mass is benign, and no additional workup is needed.
C. Two-dimensional mammography is the most sensitive modality to evaluate for fat within a breast lesion.
D. Evaluation of questionable fat content within a lesion seen on ultrasound is an appropriate indication for breast magnetic resonance imaging.
E. On ultrasound, lipomas are hypoechoic to the surrounding fat.
3. Which of the following can be included in the differential diagnosis for a malignant fat-containing lesion of the breast? (Select ALL that apply.)
A. Liposarcoma
B. Phyllodes tumor
C. Invasive ductal carcinoma
D. Invasive lobular carcinoma
E. Radial scar
Answers and Explanations
Question 1
C. Correct! Biopsy of this lesion will reveal “benign, normal glandular tissue.” This is radiologic-pathologic concordant. This is a hamartoma. On pathology, a hamartoma cannot be differentiated from normal breast tissue, since they are the same glandular elements. Therefore, core biopsy may not be helpful for making the definitive diagnosis of a hamartoma.
Other choices and discussion
A. There is an oval, fat-containing mass with circumscribed margins at the site of the palpable abnormality. Findings are characteristic for a hamartoma, and no additional imaging (including ultrasound) is needed. Hamartomas are masses within the breast composed of both glandular tissue and fat and are described as having a “breast within a breast” appearance.
B. On ultrasound, hamartomas can appear as oval, circumscribed masses with heterogeneous internal echotexture similar to normal breast tissue.
D. If the typical appearance of a hamartoma is present on a screening mammogram, no additional imaging is needed.
E. As hamartomas contain normal glandular elements, cancer can arise within a hamartoma. Thus, any suspicious finding (calcifications, suspicious mass, etc.) within a hamartoma should be worked up and biopsied to evaluate for malignancy.
Question 2
A. Correct! Most oval, circumscribed, fat-containing masses on routine screening mammography are benign and require no additional workup. Differential diagnosis of these benign entities includes lipoma, hamartoma, fat necrosis, galactocele, and lymph node.
Other choices and discussion
B. A painful, enlarging, fat-containing mass may need surgical excision, as this would be atypical for the presentation of a benign lipoma or hamartoma.
C. With the advanced technology of digital breast tomosynthesis, the ability to detect fat within masses has improved, and it is possible to visualize fat within a breast cancer. The cancer can engulf fat as it grows.
D. Mammography is currently the standard modality for the evaluation of fat within a mass originally seen on ultrasound. A bilateral breast magnetic resonance imaging is generally not used for problem solving mammographic- or ultrasounddetected lesions.
E. On ultrasound, lipomas are typically oval, circumscribed masses that range from slightly hypoechoic to hyperechoic relative to the surrounding fat. They are usually found superficially, but can appear within the deeper breast tissue.
Question 3
A–D. All of these choices are correct! Although rare, there are malignant, fat-containing lesions. These include primary liposarcoma of the breast, phyllodes tumors, and invasive cancers such as invasive ductal carcinoma and invasive lobular carcinoma. The belief is that tumors can incorporate fat within the breast as they grow.
Other choice and discussion
E. Radial scars are benign sclerosing lesions with a central fibroelastic core and radiating spiculations. In general, radial scars cause architectural distortion that is seen on mammography. Occasionally, they may centrally contain fat. A radial scar is viewed as a “high-risk lesion,” and surgical excision is recommended for core needle biopsy revealing this pathology.
Suggested Readings
Ayyappan AP, Crystal P, Torabi A, Foley BJ, Fornage BD. Imaging of fat-containing lesions of the breast: A pictorial essay. J Clin Ultrasound 2013;41:424–433 Freer PE, Wang JL, Rafferty EA. Digital breast tomosynthesis in the analysis of fat-containing lesions. Radiographics 2014;34:343–358 Yang Wei Tse. Fibroadenolipoma (Hamartoma). Statdx. http://www.statdx.com. Accessed December 29, 2015Top Tips
Fat-containing, oval, circumscribed masses without suspicious findings are benign and do not need further workup.
Differential diagnosis of benign fat-containing masses includes lipoma, hamartoma, fat necrosis, galactocele, and lymph node.
Hamartomas have the classic appearance of a “breast within a breast” on screening mammography and do not need further diagnostic workup.
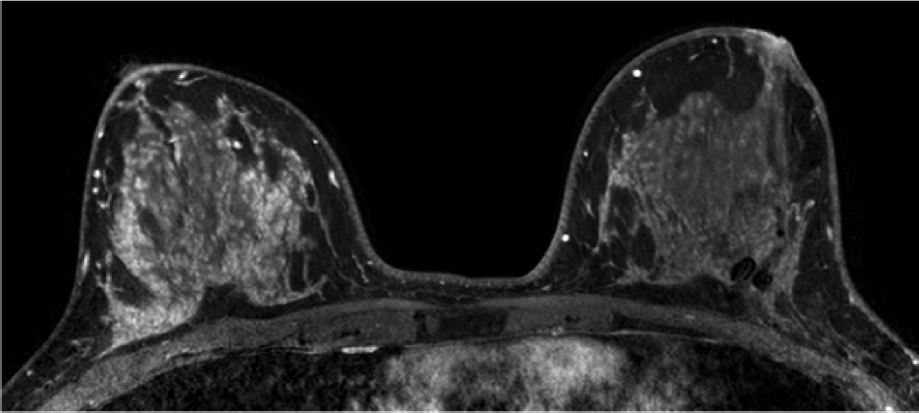
Essentials 3
Questions
1. Which of the following is the least likely reason for the imaging findings?
A. Inflammatory breast cancer
B. Renal failure on dialysis
C. Venous obstruction due to superior vena cava thrombosis
D. Congestive heart failure
2. A 35-year-old woman presents with unilateral breast enlargement, erythema, and edema for 2 days. Which ONE of the following is the best answer?
A. If there is unilateral focal skin and trabecular thickening on mammography, then her clinical and imaging findings are pathognomonic for inflammatory breast cancer, and a referral to tumor board should be made.
B. If her mammogram and ultrasound are both negative, magnetic resonance imaging should be performed.
C. If her mammogram and ultrasound show skin thickening without underlying suspicious abnormality, a trial of antibiotics and clinical follow up is recommended.
D. If a targeted ultrasound shows a fluid collection with surrounding hyperemia, a biopsy should be performed, with all samples submitted in formalin.
3. Regarding inflammatory breast cancer, which ONE of the following is the best answer?
A. The clinical presentation usually involves a slow progression of redness and skin thickening over a period of months to years.
B. A skin punch biopsy can differentiate inflammatory breast cancer from locally advanced breast cancer.
C. In a patient with newly diagnosed inflammatory breast cancer, positron emission tomography/ computed tomography is indicated.
D. Inflammatory breast cancer has a good prognosis, with a 5-year survival rate of 80 to 90%.
E. Treatment of inflammatory breast cancer usually includes mastectomy followed by radiation therapy. Chemotherapy has not demonstrated survival benefit.
Answers and Explanations
Question 1
A. Correct! There is diffuse bilateral trabecular and skin thickening on the mammogram. Inflammatory breast cancer usually presents as unilateral breast enlargement with increased density, trabecular thickening, and skin thickening on imaging. In rare cases, the findings may be bilateral secondary to severe locally advanced disease. Axillary adenopathy is present in about 50% of cases of inflammatory breast cancer.
Other choices and discussion
B. The differential for bilateral trabecular and skin thickening include systemic causes of volume overload, such as congestive heart failure, hepatic failure, and renal failure. Of note, edema resulting from these etiologies may be asymmetric due to the patient preference of positioning when in the supine position.
C. Central venous obstruction (as in superior vena cava thrombosis) can cause bilateral edema, manifested by trabecular and skin thickening. Vascular causes of unilateral breast edema include subclavian or axillary vein thrombosis.
D. In this specific case, the woman had a history of corrected tetralogy of Fallot and current severe heart and liver failure.
Question 2
C. Correct! The differential with this clinical presentation is mastitis versus inflammatory breast cancer. The clinical history, mammography, and ultrasound are collectively useful in differentiating underlying malignancy from abscess. A trial of antibiotics should first be attempted, and if findings do not completely improve after adequate antibiotic therapy, a skin punch biopsy would be advised.
Other choices and discussion
A. Inflammatory breast cancer is a clinical diagnosis. However, there must be a pathologic diagnosis of cancer coupled with an appropriate clinical presentation to make the diagnosis.
B. Magnetic resonance imaging is not indicated prior to a trial of antibiotics or before a definitive diagnosis of inflammatory breast cancer is made.
D. If the clinical history and imaging findings are concerning for abscess, an abscess drainage should be performed, with fluid sent to microbiology for culture. If no fluid can be aspirated, or if there is concern for a malignant mass, a subsequent biopsy could be performed with samples sent in formalin.
Question 3
C. Correct! Positron emission tomography/computed tomography is beneficial in newly diagnosed inflammatory breast cancer to evaluate for distant metastasis. Bone is the most common site of distant metastasis.
Other choices and discussion
A. The clinical presentation of inflammatory breast cancer is usually that of rapidly progressive breast erythema, edema, and tenderness, developing over a period of weeks to a few months. There is a lack of response to a trial of antibiotics. A commonly seen clinical finding is peau d’orange, meaning “skin of an orange” in French, caused by dermal lymphatic obstruction from tumor emboli.
B. Locally advanced breast cancer is cancer that progresses and directly invades the skin. The timeline of symptoms is the key feature that differentiates inflammatory breast cancer from locally advanced breast cancer (the latter with a slower progression and longer onset of symptoms, without the erythema or edema).
D. Inflammatory breast cancer has a highly aggressive course, with a 5-year survival rate of 25 to 50%. It accounts for approximately 2 to 5% of all breast cancers. About 20 to 40% of patients present with distant metastasis at the time of diagnosis.
E. Neoadjuvant chemotherapy followed by mastectomy and radiation therapy is the standard of care for inflammatory breast cancer. Neoadjuvant chemotherapy can shrink the existing tumor burden, helping with both locoregional control and systemic disease.
Suggested Readings
Berg, Wendie A. Trabecular Thickening, Edema (Mammography). Statdx. Accessed December 28, 2015 Yeh ED, Jacene HA, Bellon JR, et al. What radiologists need to know about diagnosis and treatment of inflammatory breast cancer: a multidisciplinary approach. RadioGraphics 2013;33:2003–2017Top Tips
For bilateral trabecular and skin thickening, think systemic causes such as fluid overload.
The main differential for an erythematous, edematous breast is mastitis versus inflammatory breast cancer. The first step in the management is an initial trial of antibiotics and, if symptoms do not resolve, a skin punch biopsy.
Imaging is integral in the evaluation of inflammatory breast cancer, directing biopsy, staging, and pretherapy planning.
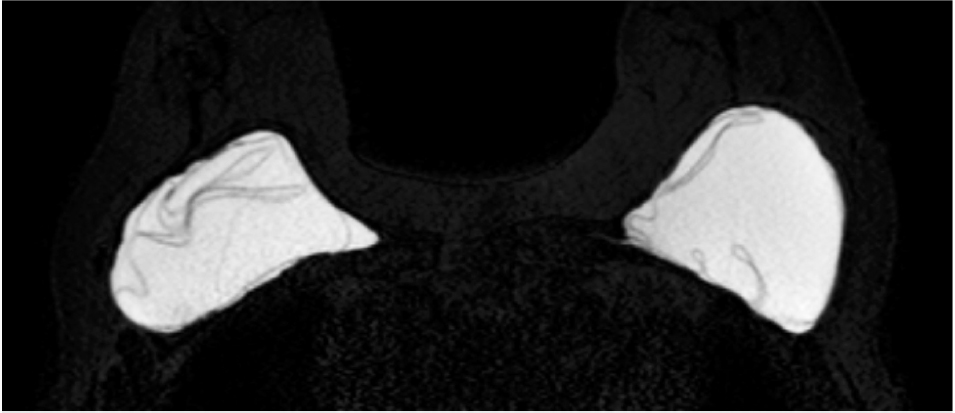
Essentials 4
Case
A 29-year-old lactating woman presents with a palpable abnormality in the left breast. A targeted ultrasound was initially performed. Subsequently, a diagnostic mammogram was performed. Spot magnification views are shown.
Questions
1. Regarding the imaging finding above, which ONE of the following is the best answer?
A. A mammogram should have been performed first to avoid a targeted ultrasound.
B. This is a suspicious abnormality, and an ultrasound-guided biopsy should be performed.
C. This is compatible with the most common benign breast mass in a lactating woman.
D. Aspiration of this finding would result in foul-smelling, serosanguinous fluid.
E. During informed consent for biopsy, no special or unusual procedural complication discussion is needed.
2. Regarding imaging of the pregnant or lactating patient, which ONE of the following is the best answer?
A. Mammography is contraindicated for the pregnant patient due to potential radiation-induced carcinogenic and teratogenic effects.
B. Bilateral breast magnetic resonance imaging is a safe imaging modality for the fetus during pregnancy and for the infant during lactation.
C. Lactating patients should pump or nurse prior to having a mammogram performed.
D. Pregnancy-associated breast cancer most commonly presents as a painful lump.
E. The prognosis of women with pregnancy-associated breast cancer is worse than those with age- and stage-matched controls.
3. Which of the following should be included in the differential diagnosis of a breast mass in a pregnant or lactating patient? (Select ALL that apply.)
A. Pregnancy-associated breast cancer
B. Fibroadenoma
C. Lactating adenoma
D. Galactocele
E. Breast abscess
Answers and Explanations
Question 1
C. Correct! This is compatible with a galactocele, which is the most common benign breast mass in a lactating woman. These form as a result of duct dilation and inflammation. A fat-fluid level is considered pathognomonic for a galactocele; however, this may also be seen in fat necrosis.
Other choices and discussion
A. The initial imaging workup for a woman < 30 years old with a palpable abnormality should be a targeted ultrasound. Ultrasound is also the first-line imaging modality in the workup of a palpable breast mass for a pregnant or lactating patient. This is because of ultrasound’s lack of ionizing radiation and its high sensitivity for detecting cancer in this patient population. In cases where sonographic findings are equivocal for a galactocele, a mammogram can aid in the diagnosis. The mammographic images shown in this case are consistent with a galactocele. Therefore, no ultrasound is needed.
B. This is not a suspicious abnormality, and biopsy is not indicated. Mammogram reveals an oval mass with obscured margins and a fat-fluid level on the mediolateral view. These findings, in addition to the clinical context of lactation, are consistent with a galactocele.
D. Galactoceles are cysts that contain milk and often contain necrotic or inflammatory debris. Aspiration would result in milkycolored fluid (not foul-smelling, serosanguinous fluid).
E. Additional potential complications following breast biopsy of a lactating woman include a milk-duct fistula (which is extremely rare) and blood within the breast milk. These risks should be discussed prior to the procedure.
Question 2
C. Correct! The milk may increase breast density and obscure important findings. Thus, prior to mammography, lactating patients are asked to pump or nurse to decrease the volume of milk.
Other choices and discussion
A. The low levels of scatter radiation do not support delaying mammography during pregnancy, when clinically indicated.
B. Bilateral breast magnetic resonance imaging requires intravenous gadolinium-based contrast. These contrast agents are NOT recommended during pregnancy because of the possible harmful effects to the developing fetus. However, there is a negligible excretion of this contrast in breast milk (a rate of 0.0004% of the maternal dose), and breast MRI can be safely performed in the lactating patient.
D. Pregnancy-associated breast cancer most commonly presents as a painless lump. It may also present as a unilateral enlarging breast with skin thickening, focal pain, and suspicious nipple discharge.
E. Traditionally, it was thought that women with pregnancy-associated breast cancer had a worse prognosis than those who did not. This may be explained by a delay in diagnosis (with larger tumor size at presentation). However, compared to age- and stage-matched controls, there are actually similar survival rates between woman with pregnancy and non-pregnancy-related breast cancers.
Question 3
All are correct!
A. Pregnancy-associated breast cancer represents approximately 10% of all newly diagnosed breast cancer cases in women < 40 years old. The mean age at diagnosis is between 32 and 34 years. The most common histology is high-grade, estrogen and progesterone receptor negative, invasive ductal carcinoma.
B. Growth of fibroadenomas can occur during pregnancy, as these are hormone-sensitive masses.
C. Lactating adenomas are benign lesions thought to be a fibroadenoma variant, tubular adenoma, or lobular hyperplasia due to the physiologic changes of pregnancy. In general, these may regress after pregnancy.
D. Galactoceles are the most common benign lesions in lactating woman. They are cysts that contain milk and inflammatory debris.
E. Disruption of the nipple-areolar complex and milk stasis places lactating women at risk for infection. If abscess is suspected, a clinical exam and ultrasound are recommended as the best initial workup.
Suggested Readings
American College of Radiology. ACR manual on contrast media v10.1. From: http://www.acr.org/quality-safety/resources/contrastmanual. Published 2015. Accessed February 12, 2015 Barnes DM, Newman LA. Pregnancy-associated breast cancer: a literature review. Surg Clin North Am 2007;87:417–430, x Chetlen AL, Brown KL, King SH, et al. JOURNAL CLUB: scatter radiation dose from digital screening mammography measured in a representative patient population. Am J Roentgenol 2016;206:359–365 Sabate JM, Clotet M, Torrubia S, et al. Radiologic evaluation of breast disorders related to pregnancy and lactation. Radio-Graphics 2007;27:S101–S124 Vashi R, Hooley R, Butler R, Geisel J, Philpotts L. Breast imaging of the pregnant and lactating patient: imaging modalities and pregnancy-associated breast cancer. Am J Roentgenol 2013;200:321–328Top Tips
Although mammography is safe to the fetus during pregnancy, ultrasound is the BEST initial imaging modality when evaluating a palpable abnormality in the pregnant or lactating patient.
A fat-fluid level seen within a mass on mammography in a lactating patient is consistent with a galactocele.
Pregnancy-associated breast cancer accounts for approximately 10% of breast cancers in woman < 40 years old.
Essentials 5
Questions
1. Which of the following is the best possible reason for this finding on magnetic resonance imaging?
A. A history of radiation therapy on the left
B. Inflammatory breast cancer on the right
C. Exogenous hormones
D. The patient was imaged on day 23 of her menstrual cycle
E. Injection of gadolinium on the right
2. Which of the following are generally accepted indications for bilateral breast magnetic resonance imaging? (Select ALL that apply.)
A. Screening for a patient with > 10% lifetime risk and no additional risk factors
B. Evaluation of a woman with newly diagnosed breast cancer
C. Evaluation of a patient with metastatic axillary adenocarcinoma and an unknown primary
D. Evaluation of saline implant integrity
E. Evaluation of breast cancer response to neoadjuvant chemotherapy
3. Regarding dynamic kinetic enhancement characteristics of magnetic resonance imaging findings, which ONE of the following is the best answer?
A. The first postcontrast phase of the exam should be acquired within the first 2 minutes postinjection.
B. There are three main phases of the time-intensity curve: initial, peak, and delayed.
C. A lesion with rapid initial phase enhancement and washout on delayed phase enhancement is suspicious and should be biopsied.
D. A lesion with medium initial phase enhancement and persistent delayed phase enhancement is benign.
E. A lesion that does not meet the 50% enhancement threshold kinetics is benign.
Question 1
A. Correct! A history of radiation therapy on the left. Susceptibility artifact from surgical clips is present in the posterolateral left breast in this patient with a history of left lumpectomy and radiation therapy. The enhancement on the right corresponds to normal background parenchymal enhancement (BPE). Radiation therapy is known to decrease the amount of BPE.
Other choices and discussion
B. Although inflammatory breast cancer can present as asymmetric trabecular thickening and enhancement, there is no evidence of breast enlargement or skin enhancement in this patient.
C. BPE is dependent on several factors, one of which is hormones. Although the presence of exogenous hormones can increase the BPE, this typically results in bilateral and symmetric variation.
D. Similar to the influence of exogenous hormones, timing of the menstrual cycle can affect the amount of BPE. However, this fluctuation would typically be symmetric. The ideal imaging time with the least amount of BPE is during the follicular phase of the cycle (days 7 to 15).
E. There are no studies to show that laterality of contrast injection affects the amount of enhancement in the breast.
Question 2
B. Correct! Current National Comprehensive Cancer Network practice guidelines recommend that a breast magnetic resonance imaging (MRI) can be considered to evaluate the extent of disease in a patient with newly diagnosed breast cancer.
C. Correct! In patients with mammographically occult breast cancer and biopsy-proven axillary metastatic adenocarcinoma, a bilateral breast MRI can discover the primary lesion in approximately 60 to 70% of cases.
E. Correct! Results from the American College of Radiology Imaging Network (ACRIN 6657) study showed that MRI findings are a stronger predictor of pathologic response from neoadjuvant chemotherapy and residual cancer burden than is the clinical assessment.
Other choices and discussion
A. The American Cancer Society currently recommends the use of screening breast MRI for patients with a > 20% lifetime risk of breast cancer. In a high-risk patient population, combined MRI and mammography have a higher sensitivity (92.7%) than combined ultrasound and mammography (52%).
D. Bilateral breast MRI can evaluate for silicone implant integrity. Saline implant complications are usually apparent on clinical exam, and the saline is reabsorbed within the body.
Question 3
A. Correct! The first postcontrast phase of the exam should be acquired within the first 2 minutes postinjection. Imaging after this time will result in missing the peak enhancement of the lesion.
Other choices and discussion
B. The time intensity curves are divided into two phases: the “initial phase,” with images acquired within the first 2 minutes after injection, and the “delayed phase,” with images acquired after the first 2 minutes or peak enhancement. In general, peak enhancement usually occurs after 2 to 3 minutes of injection.
C. Although the most suspicious type of kinetic enhancement is initial rapid enhancement with washout on delayed images, there are benign findings (e.g., lymph nodes) that have the same enhancement characteristics. Thus, morphologic characteristics should be examined before a biopsy recommendation is made.
D. Kinetics are useful in the evaluation of any lesion (focus, mass, non-mass enhancement). However, a benign kinetic enhancement profile should not dissuade further workup for a morphologically suspicious mass or non-mass enhancement.
E. The enhancement threshold for computer-aided analysis tools can be selected by the interpreting radiologist and is usually set between a 50 and 100% increase in signal intensity from baseline to the first postcontrast study. Absence of a morphologically suspicious finding to meet threshold kinetic features does not prove benignity.
Suggested Readings
Berg WA. Tailored supplemental screening for breast cancer: what now and what next? Am J Roentgenol 2009;192:390–399 Brenner RJ. Evaluation of breast silicone implants. Magn Reson Imaging Clin N Am 2013;21:547–560 de Bresser J, de Vos B, van der Ent F, Hulsewé K. Breast MRI in clinically and mammographically occult breast cancer presenting with an axillary metastasis: a systematic review. Eur J Surg Oncol 2010;36:114–119 Hylton NM, Blume JD, Bernreuter WK, et al. Locally advanced breast cancer: MR imaging for prediction of response to neoadjuvant chemotherapy—results from ACRIN 6657/I-SPY TRIAL. Radiology 2012;263:663–672Top Tips
The American Cancer Society currently recommends the use of screening breast MRI for patients with a > 20% lifetime risk of breast cancer.
The amount of BPE is influenced by hormonal factors and can fluctuate depending upon menstrual cycle and exogenous estrogens.
A benign kinetic enhancement curve is reassuring. However, these features do not override suspicious morphologic features when evaluating a lesion.
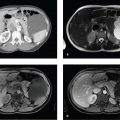
Essentials 6
Questions
1. Regarding the bilateral breast magnetic resonance imaging performed for silicone implant evaluation, which ONE of the following is shown?
A. Normal intact implants with bilateral complex radial folds
B. Intracapsular rupture on the left and extracapsular rupture on the right
C. Bilateral intracapsular rupture
D. Bilateral extracapsular rupture without intracapsular rupture
E. Bilateral intracapsular and extracapsular rupture
2. Regarding silicone breast implants, which ONE of the following is the best answer?
A. Silicone implants are harmful and increase the risk of developing breast cancer.
B. Mammography is useful in the evaluation of intracapsular silicone implant rupture.
C. Breast magnetic resonance imaging is the secondline imaging modality to evaluate for a silicone implant complication.
D. The presence of breast implants decreases mammographic sensitivity for detecting breast cancer.
E. A standard T2-weighted sequence should be used to evaluate for silicone implant complication.
3. Regarding silicone implant complications, which ONE of the following is the best answer?
A. A breast magnetic resonance imaging should be performed annually to evaluate for silicone implant complication in asymptomatic patients.
B. Extracapsular rupture can only occur when the implant capsule is fully collapsed.
C. Implant herniation implies underlying intracapsular rupture.
D. Radial folds can generally be traced back to the implant capsule, whereas folds from a collapsed rupture are separated from the capsule.
E. Silicone granulomas have the same T2 signal intensity on water-suppressed images as the silicone gel within the implants.
Answers and Explanations
Question 1
C. Correct! There is bilateral intracapsular rupture. There is a “linguine” sign on the right, which indicates complete collapse of the silicone implant shell, and both a “linguine” (medially) and “keyhole” or “teardrop” (posteriorly) sign on the left. The keyhole sign indicates silicone gel outside of the implant shell but still contained within the fibrous capsule.
Other choices and discussion
A. Radial folds are normal infoldings of the implant shell, and they may mimic intracapsular rupture when complex. However, in this case, there is discontinuity of the implant capsule bilaterally (with partial collapse of the right implant).
B. There is no evidence of extracapsular rupture (silicone within the surrounding breast tissue) or silicone within lymph nodes on this image.
C. There must be intracapsular rupture (defect in the silicone implant shell) for extracapsular rupture to be present (rent in the fibrous capsule surrounding the implant).
D. There is no evidence of extracapsular rupture.
Question 2
D. Correct! In a study evaluating the effect of breast augmentation on the accuracy of mammography and cancer characteristics, the sensitivity of screening mammography was lower in women who had breast augmentation than in those who did not. However, the prognostic factors (tumor stage, nodal status, and estrogen-receptor status) were similar.
Other choices and discussion
A. There is no evidence that shows a cause or effect relationship between silicone breast implants and the development of breast cancer.
B. With intracapsular rupture, the implant shell (or envelope) is defective. However, the fibrous capsule that the body creates and surrounds the implant with is still intact. Thus, if there is an intracapsular silicone implant rupture, magnetic resonance imaging is superior to mammography for detection.
C. Manufacturer recommendations approved by the U.S. Food and Drug Administration support magnetic resonance imaging as the first-line imaging modality in the evaluation of a silicone implant complication.
E. Silicone gel has a T2-signal intensity that is higher than fat but lower than water. Thus, to truly evaluate for silicone extravasation either surrounding the implant shell or into the breast, it is best to use a T2-weighted sequence that suppresses both fat and water.
Question 3
D. Correct! Radial folds can generally be traced back to the implant capsule, whereas folds from a collapsed rupture are separated from the capsule. Tracing the origin of radial folds to the inner surface of the implant capsule is the key to distinguishing complex radial folds from intracapsular rupture.
Other choices and discussion
A. Asymptomatic women with implants are advised to have an MRI to check for implant rupture 3 years after placement and every 2 years thereafter, although some authors believe this may be too frequent and suggest every 10 years for patients without a breast cancer history.
B. Intracapsular rupture can be staged based upon the extent of deflation, ranging from not collapsed to fully collapsed. Extracapsular rupture can occur during any of these stages.
C. The term herniation is used when the implant shell is extruded through the fibrous capsule that surrounds the implant. Implants with herniation may not necessarily have a rupture, but herniation does imply a focal weakening/defect in that area.
E. Both silicone granulomas and silicone within lymph nodes have lower signal intensity on T2 water-suppressed sequences than does pure silicone gel. This is due to tissue ingrowth and the ratio of lymph node to silicone within nodes, respectively.
Suggested Readings
Middleton MS. MR evaluation of breast implants. Radiol Clin North Am 2014;52:591–608 Miglioretti DL, Rutter CM, Geller BM, et al. Effect of breast augmentation on the accuracy of mammography and cancer characteristics. JAMA 2004;291:442–450 Wiedenhoefer JF, Shahid H, Dornbluth C, Otto P, Kist K. MR imaging of breast implants: useful information for the interpreting radiologist. Appl Radiol 2015;44(10):18–24Top Tips
Saline implant rupture is a clinical diagnosis.
There are two major types of silicone implant rupture: intracapsular, which describes a break in the silicone implant shell, and extracapsular, which occurs when there is both a break in the implant shell and in the fibrous capsule.
Complex radial folds can mimic intracapsular rupture. Tracing the folds back to the implant capsule helps to differentiate the two.
Essentials 7
Questions
1. Regarding the imaging findings, which ONE of the following is the BEST answer?
A. BI-RADS 6. The imaging findings are consistent with multicentric breast cancer.
B. BI-RADS 0. Recommend spot compression views and ultrasound for confirmation.
C. BI-RADS 4. Recommend biopsy of the most suspicious appearing mass.
D. BI-RADS 3. Probably benign masses. Recommend short interval follow up.
E. BI-RADS 2. The imaging findings are benign. Recommend normal interval follow up.
2. Regarding bilateral benign-appearing masses, which ONE of the following is correct?
A. Diagnosis requires at least two masses, with one located in each breast.
B. A round or oval mass with indistinct margins meets diagnostic criteria.
C. Imaging findings are still considered benign even in the setting of a palpable lump.
D. A mass appearing distinctly different from the others warrants diagnostic workup.
E. There is an associated increased risk of breast cancer.
3. A baseline screening mammogram demonstrates bilateral calcifications. Regarding calcifications, which ONE of the following is correct?
A. Tram-track calcifications are suspicious.
B. Large rod-like calcifications radiating toward the nipple are suspicious.
C. Similar appearing groups of bilateral coarse heterogeneous calcifications are considered suspicious.
D. Diffuse punctate and round calcifications are benign.
E. Rim calcifications are suspicious.
Answers and Explanations
Question 1
E. Correct! BI-RADS 2. The mammographic findings are classic for bilateral benign-appearing masses. Normal interval follow up is recommended.
Other choices and discussion
The imaging findings are most consistent with bilateral benign-appearing masses. There is no mammographic evidence of malignancy. No further imaging is required, short-term follow up imaging is not needed, and biopsy is not indicated.
Question 2
D. Correct! Overall, the bilateral benign-appearing masses should appear similar. A mass appearing distinctly different from the others warrants diagnostic workup.
Other choices and discussion
A. Diagnosis requires at least three masses, with at least one located in each breast.
B. A round or oval mass with circumscribed margins meets diagnostic criteria. A mass with indistinct margins warrants diagnostic workup.
C. A palpable lump requires dedicated diagnostic workup, even if there are bilateral benign-appearing masses.
E. There is no increased risk of malignancy.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree