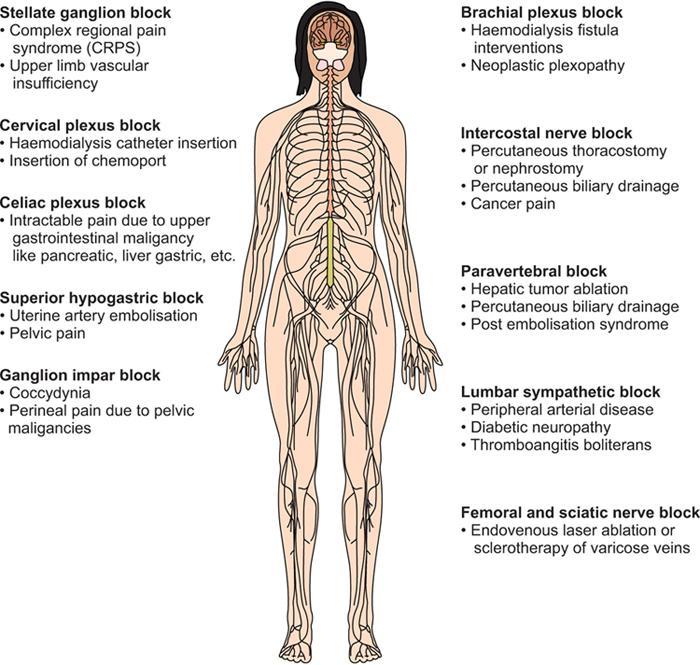
Neeraj Mehta The interventional radiology procedures have increased in leaps and bounds in present times and have become more lengthy and complex. These procedures are usually conducted under local anaesthesia with the patient awake and using minimal sedation. The application of sedatives and analgesics to relieve patient anxiety and pain will go long way in allaying side effects of the procedure per se, thereby making the experience more pleasant and satisfactory for the patient. Good sedation techniques, along with adequate analgesia and supportive patient management all play integral roles in minimizing interventional side effects, thus enhancing the patient’s experience and optimizing patient outcome. Regional anaesthesia leads to numbing of a particular body part thereby relieving pain and allowing surgery to be undertaken. It has various types: Subarachnoid block (aka Spinal), epidural anaesthesia (including caudal) and peripheral nerve blocks. In this chapter, we will discuss nerve blocks, which can help the interventional radiologist to do interventional procedures more painlessly and also helps in building practice in pain management (Fig. 2.18.1). There has been an increase in the application of nerve blocks given peripherally owing to minimization of peri-procedural complications due to opioid usage (e.g., respiratory depression, nausea, pruritis), general anaesthetic agents overdose, metabolic and electrolyte imbalances. It also alleviates the need for general anaesthesia, which is hazardous in high-risk patients and concomitantly raises patient tolerability during IR procedures along with post-procedure comfort. Nowadays, Interventional Radiologist play a prominent role in a multidisciplinary team for management of malignancy, from the initial diagnosis to minimally invasive treatment of malignancy and its complication, which can further be extended to pain management in the form of nerve block or ablative therapies. aExplained in this chapter. The most frequently used local anaesthetics include lidocaine, bupivacaine and ropivacaine. These agents are highly stable and rarely cause allergic reactions, and such reactions are usually caused by either their metabolite p-aminobenzoic acid or methylparaben (a preservative found in some preparations). LAs are often used in combination with other Las (short and long-acting) or additives to maximize their desired effect or to reduce their toxicity. Typical doses of commonly used local anaesthetics are – Lidocaine 4.5 and 7 mg/kg without and with epinephrine respectively having duration of action of about 1 to 3 hrs, Bupivacaine 2.5 and 3 mg/kg without and with epinephrine respectively having duration of action of about 4 to 16 hrs and Ropivacaine 3.5 mg/kg with duration of action about 5 to 8 hrs. These are potent anti-inflammatory and pain modulating drugs. Corticosteroids can be injected with the goals of short-term and medium-term pain relief, reduction of inflammation and improved mobility. Steroid injections usually take 48–72 h to be effective and, hence, are combined with local anaesthetics for a rapid onset of action. Commonly used corticosteroids are Methylprednisolone, Triamcinolone and Betamethasone. Neurolytic agents are used to causing permanent damage to nerves or a nerve plexus with the aim of providing relief from pain by interrupting the transmission of pain signals in the nerves. The most commonly used agents are alcohol (50%–100%) and Phenol (4%–15%). These cause nerve destruction by inducing protein precipitation, however, alcohol is more efficient in destructing nerve cell bodies and hence has regeneration is less as compared to phenol. Radiofrequency ablation is the procedure where an electrical current is applied to induce thermocoagulation and neural destruction. It has been widely used to ablate or modulate pain pathways in the trigeminal ganglion, spinal cord, dorsal root ganglion, sympathetic chain, facet joints and peripheral nerves. Radiofrequency ablation is of two types: Conventional and Pulsed. In Conventional radiofrequency ablation (CRF), the temperature may go up to 85°C but in pulsed radiofrequency ablation (PRF), the temperature is not raised beyond 42°C. Pulsed radiofrequency differs from CRF in that pulsed radiofrequency does not lead to a neurodestructive process. Pain relief from the destruction of nerves following exposure to extreme cold is called cryoanalgesia. The procedure has no systemic side effects and the major advantage of this procedure is the absence of neuritis or neuroma formation and it has a reversible effect as compared to chemical neurolysis or radiofrequency ablation. It can also be performed as an outpatient procedure. Brachial Plexus (BP) is formed by ventral rami of C5 through C8 and T1; some people may have input from C4 or T2. There are four approaches for brachial plexus block, namely interscalene, supraclavicular, infraclavicular and axillary.
2.18: Image guided nerve blocks and sympathectomies
Introduction
Overview
Peripheral nerve blocks which could be useful for IRS
aBrachial Plexus Block
Sympathetic Block or Sympatheticolysis
Intercostal nerve block
aStellate ganglion block
Paravertebral block
aSuperficial cervical plexus block
Transverse Abdominis plane block
aSuperior hypogastric block
Saphenous nerve block
aGanglion impar block
aFemoral and sciatic nerve block
Lumbar sympathetic block
Medications used in nerve block
Local anaesthetics
Corticosteroids
Typical Dosages of Commonly used Steroid
Steroid
Common Concentration (in mg/mL)
Duration of Action (in days)
Methylprednisolone acetate (Depomedrol)
40 or 80
8
Triamcinolone acetonide (Kenalog)
10 or 40
14
Betamethasone
4 or 6
14
Neurolytic agents
Neurolytic agent
Strength
Benefits
Drawbacks
Systemic toxicity
Alcohol
50%–100%
Hypobaric, fast onset
Painful on injection, risk of neuritis (peripheral nerves)
Disulfiram like reaction
Phenol
4%–15%
Hyperbaric, painless, slow onset
Short-lived, affinity for vasculature
Convulsions, Cardiovascular collapse
Ablative therapies
Radiofrequency ablation or lesioning
Cryoablation
Brachial plexus block
Indications
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree








