Central venous catheters (CVCs) are commonly used in patients in a variety of clinical settings, including the intensive care unit, general ward, and outpatient settings. After placement, the radiologist is frequently requested to evaluate the location of CVCs and deem them suitable for use. An understanding of the ideal location of catheter tips as well as the approach to identifying malpositioned catheter tips is essential to prevent improper use, recognize and/or prevent further injury, and direct potential lifesaving care. An approach to CVC placement based on tip location can be helpful in localization and guiding management.
Key points
- •
The radiologist is frequently requested to evaluate the location of central venous catheter (CVC) tips and deem them suitable for use. An approach to CVC placement based on tip location (right of midline, left of midline, or midline) can be helpful in localization and guiding management.
- •
The ideal anatomic location for a CVC tip is in the lower superior vena cava or upper right atrium, also known as the superior right cavoatrial junction.
- •
When encountered with a catheter tip located to the left of the midline, the following locations should be considered: left-sided superior vena cava, left superior intercostal vein, left pericardiophrenic vein, left superior anomalous pulmonary vein, and left internal mammary vein.
- •
CVCs with the tips located to the right of the midline have several potential locations in addition to the desired location of the superior vena cava, including the right internal mammary, right pericardiophrenic, azygous vein, and, rarely, an anomalous right superior pulmonary vein.
- •
In the setting of arterial placement of a CVC, CT can be used to illustrate the site of arterial access and in turn direct further management.
Introduction
Central venous catheters (CVCs) are commonly used in patients in a variety of clinical settings, including the intensive care unit (ICU), general ward, and outpatient settings. CVC, also known as a central line or central venous line, is defined as a catheter placed into a large vein, with the tip typically terminating within the superior vena cava (SVC) or inferior vena cava (IVC). CVCs enable continuous access to the venous system and are a mainstay for treatment in the ICU setting. CVCs are typically placed for administration of fluids, medication delivery, repeated blood draws, hemodynamic monitoring, total parenteral nutrition, and dialysis access.
The type of CVC placed is typically dependent on the expected duration of the catheter use. Short-term CVCs are deployed with the expectation to remain in place for use for days to weeks. As a result, they are not tunneled under the skin. The tunneling may decrease the risk of infection but adds to the complexity of the procedure. Long-term CVCs are tunneled lines typically placed for intravenous (IV) therapy or multiple repeated intermittent treatments, with the expectation of use lasting longer than 4 weeks. Regardless of the expected duration of use, CVCs are available in a variety of lengths, gauges, and lumens. Multiple lumen catheters allow for simultaneous functions, such as drug infusions, blood draws, and hemodynamic monitoring. The multiple lumens may have different lengths, with a staggered termination of the tips, or all tips may terminate at the same length.
Short-term catheters can be inserted, exchanged, and removed at the bedside and frequently are used in the ICU setting. Reported rates of CVC usage range from 13% to 91% in the ICU setting. In the authors’ experience, it is rare for an ICU patient to have no central catheter. CVC placement may result in a multitude of complications, including infection, hemorrhage, and thrombosis. Not infrequently, complications may result from catheter insertion or malpositioning. Multiple studies have demonstrated that a malpositioned CVC occurs approximately 10% of the time. Frequent sites of misplaced catheters include the internal jugular vein, azygous vein, superior intercostal vein, contralateral subclavian vein, and axillary vein. A majority of the complications are minor with vessel wall perforation the most common severe complication. Vessel wall perforation may result in pneumothorax, hemothorax, mediastinal/soft tissue hematoma, and cardiac perforation. Pneumothorax is the result of wall perforation, occurring in approximately 2% of cases Complications are more common with subclavian vein placement compared with jugular placement.
The American College of Radiology Appropriateness Criteria on the radiological management of central venous access recommends a chest radiograph after insertion of a CVC and/or Swan-Ganz catheter to demonstrate proper placement and possible complications. Rarely, computed tomography (CT) may be used as a problem-solving technique when the radiograph is ambiguous. After initial insertion, follow-up chest radiographs demonstrate little benefit in revealing complications and are suggested only when there is a clinical suspicion of a catheter-related complication. The radiologist, then, has the potential to play a key role after CVC placement in the recognition of correct positioning of the CVC as well as catheter-related complications in order to prevent adverse outcomes and prompt potentially life-saving intervention in cases of a rare life-threatening complication.
Normal catheter placement
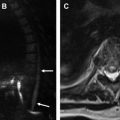
The tip of the CVC should be distal to the last venous valve, which is located at the confluence of the internal jugular and subclavian veins. On the chest radiograph, this location typically is seen at the first intercostal space. The ideal anatomic location for a CVC tip is in the lower SVC or upper right atrium, also known as the superior right cavoatrial junction. The location of the CVC tip typically is verified by obtaining a portable chest radiograph after CVC placement, prior to the first use of the catheter. Although other methods, such as ultrasound, electrocardiography, and impedence technology, have been explored for catheter verification, the chest radiograph remains the standard of care at most institutions. A portable chest radiograph is easily obtained and imparts a very low effective radiation dose; approximately 0.02 mSv, or the equivalent of 3 days of background radiation at sea level. The lower SVC is located below the right mainstem bronchus, above the superior cavoatrial junction ( Fig. 1 A ). The superior cavoatrial junction is approximately 2 vertebral bodies below the carina (see Fig. 1 A). In certain scenarios it may be difficult to accurately localize the tip of the catheter secondary to overlying structures or patient body habitus. An additional lateral or oblique view can be obtained to demonstrate proper location of the catheter ( Fig. 1 B). In the current era of digital radiography, adjusting contrast and brightness with narrow window widths can be utilized to help locate catheter tips in suboptimal exposures.

Malpositioned catheters
The authors propose a simplified approach to evaluation of malpositioned catheters, with an emphasis placed on the location of the catheter relative to the midline. Close attention should be paid to possible intra-arterial course of the catheter. Furthermore, the chest radiograph should be used to evaluate for secondary complications of catheter placement, including pneumothorax and vascular perforation. When there is concern for malposition of a CVC, orthogonal images and injection of contrast material can be used to verify the precise location. Increasingly, CT is used as a problem-solving technique.
Right-sided venous catheters
CVCs with the tips located to the right of the midline have several potential locations in addition to the desired location of the SVC. These potential venous locations include normal structures, most commonly, the right internal mammary, right pericardiophrenic, and azygous vein. Rarely, a CVC may find its way into an anomalous right superior pulmonary vein.
The right anterior aspect of the chest is drained by the right internal mammary vein, also referred to as the right internal thoracic vein. The right internal mammary vein drains the anterior intercostal veins and anastomoses with abdominal wall vessels. The right internal mammary vein courses superiorly and drains cranially into the innominate vein. The orifice of the right internal mammary vein is located close to the origin of the SVC and can be entered during catheter placement from both right-sided and left-sided approaches. CVCs located within the right internal mammary vein may be slightly lateral to the SVC, just to the right of the sternal boarder, on the frontal view with a distinct anterior course seen on the lateral view. The frontal radiograph often demonstrates a distinctive curve or notching of the catheter as it enters the internal mammary vein ( Fig. 2 ).

The right pericardiophrenic vein is a small vein responsible for drainage of the pericardium, pleura, and diaphragm. The vein courses lateral to the right heart boarder traveling adjacent to the phrenic nerve. The right pericardiophrenic vein drains directly into the right internal mammary vein. In patients with venous obstruction, it may serve as a collateral pathway for venous drainage. It often anastomoses with the inferior phrenic vein. Although not frequently entered during CVC placement, given its diminutive size, placement may result in thrombosis or perforation.
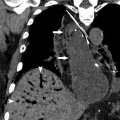
The azygous vein is located to the right of the vertebral bodies and enters the thorax through the aortic hiatus and courses superiorly within the thorax carrying deoxygenated blood from the posterior chest and abdominal walls. Although the term, azygous , translates to without a pair , the azygous vein often communicates with the left-sided equivalent—the hemiazygous vein. The azygous vein forms around the level of T12-L2 from the confluence of ascending lumbar veins and right subcostal veins. Differing from other right-sided venous structures, the azygous vein courses through the posterior or middle mediastinum before arching over the right mainstem bronchus, at which point it joins the SVC ( Fig. 3 ). This course posterior to the trachea is best appreciated on the lateral projection.

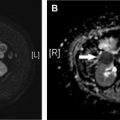
A right superior anomalous pulmonary vein is equally as common as a left superior anomalous pulmonary vein. It represents a congenital malformation in which the blood supply from the right upper lobe drains directly to the systemic venous system or right atrium. The most common site of drainage is the SVC, although drainage into the right atrium, right brachiocephalic vein, coronary sinus, and azygous system have all been reported. Even more rarely, the anomalous vein may drain into the portal vein, ductus venosus, or inferior vena cava. This lesion results in a left to right shunt. Typically, these patients have an associated sinus venosus type atrial septal defect. A catheter within an anomalous right upper lobe pulmonary vein has the tip located to the right of the expected location of the SVC extending toward the right upper lobe. It often appears as if the tip is freely floating in the lung itself. The lateral view shows a midline location ( Fig. 4 ). A catheter in a pulmonary vein can be confusing if an arterial blood gas is used to confirm venous placement because the blood is richly oxygenated.

Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree