div class=”ChapterContextInformation”>
12. Current Imaging Approaches and Challenges in the Assessment of Coronary Artery Disease
Keywords
Coronary wallPlaque vulnerabilityHigh-risk plaqueIntravascular ultrasoundOptical coherence tomographyMagnetic resonance imagingCoronary computed tomography angiographyIntroduction
For many decades, coronary angiography was the gold standard for the study of coronary artery diseases. Angiography allows a two-dimensional assessment of the coronary lumen, a vessel silhouette. Important components of the atherosclerotic process in the coronary vessel wall are not evaluated by angiography, such as positive remodeling, plaque composition, plaque extension, or diffuse atherosclerosis. Currently, evaluating the cardiovascular risk based on diagnosing coronary stenosis by angiography is not enough for both the diagnosis and the therapeutic definition in coronary artery disease (CAD). The new paradigm is evaluating the coronary artery wall. We know that acute coronary events are caused mainly by plaques with small degrees of stenosis, but with vulnerability characteristics that are hardly diagnosed by angiography.
Several diagnostic methods have been used to evaluate the characteristics of arterial walls in order to identify early stages of CAD and features that are able to predict plaque vulnerability. Many characteristics are evaluated in coronary artery wall. Some of the most clinically valuable characteristics are plaque burden, plaque volume, plaque extension, plaque high-risk features and contents, and signs of inflammation. Currently, there is no diagnostic method capable to accurately evaluate all these characteristics at the same time. Therefore, the combination of methods to achieve a complete diagnosis is necessary. Based on the clinical history, a reasonable approach is to choose a method that provides the best answer to the clinical decision-making. In this chapter, we will cover clinically available techniques for evaluating the coronary artery wall, its related diseases, and limitations of each technique.
Invasive Diagnostic Methods to Assess Coronary Wall
In order to better evaluate the coronary atherosclerosis, new diagnostic techniques such as intravascular ultrasound (IVUS) and optical coherence tomography (OCT) arose to complement the angiography exams. Both techniques corroborate and enrich coronary lumen assessment providing additional and valuable information regarding the coronary wall.
Intravascular Ultrasound
The first reports about the use of IVUS appeared in the end of the 1980s. Since then, its use has become increasingly commonplace and technological advances made it increasingly clinically useful. Initially, IVUS exams used gray-scale technique to assess the coronary wall characteristics. This technique had several limitations which compromised its diagnostic accuracy. Current acquisition and processing technologies such as the backscattered ultrasound waves using radio frequency allow accurate analysis of coronary wall. IVUS enables plaque composition discrimination (necrotic core, fibrous tissue, fibrofatty tissue, and dense calcium) as well as determining characteristics of high-risk plaques [1–3]. These diagnostic abilities allow us to use IVUS in monitoring the evolution of atherosclerosis over time and therapeutic response manifested by regression in plaque volume [4, 5].
An important clinical use of IVUS is diagnosing vulnerable plaques. Some plaque vulnerability characteristics assessed by IVUS are the thin-cap fibroatheroma (TCFA), positive remodeling, large plaque burden, and small luminal area. The PROSPECT study showed that in patients with acute coronary syndrome (ACS) plaques with vulnerability signs had increased risk of major acute coronary events (MACE) even in non-culprit lesions [6].
Another quite common clinical use of IVUS is during percutaneous coronary intervention (PCI). IVUS findings help before, during, and after procedure completion. IVUS can be used to choose the most appropriate technique and materials to be used during the PCI. It helps to confirm angiography findings and accurately reports the degree of coronary stenosis, plaque extension, plaque components, coronary ostium involvement, and vessel size. After the procedure, IVUS evaluates minimal lumen area, stent malapposition, stent edge, dissection, and tissue prolapse that may be determinant of future complications such as restenosis and stent thrombosis [2]. Metanalyses focused on comparing IVUS-guided PCI with procedures guided exclusively by angiography showed better immediate and late angiographic results (greater post-minimal lumen diameter, lower restenosis, and revascularization requirement) as well as reduction in MACE [7, 8]. Currently, there is an increasing use of IVUS during PCI, especially when implanting drug eluting stents, where the risks of thrombosis and restenosis are significantly higher if there is stent malapposition. The IVUS-guided PCI is recommended for cases with increased complexity (complex lesions, chronic occlusion, bifurcations with ostium involvement, extensive plaques, or left main artery involvement) or to assess stent failure [9].
Limitations
Despite its excellent diagnostic capacity, IVUS usage to cardiovascular evaluation in general population is restricted for its invasive nature. IVUS exams must be performed in a hemodynamic laboratory, with a trained team and executed by a highly experienced hemodynamicist. All exams use iodinated contrast and need ionizing radiation to precisely locate the target vessel or lesion to be studied. Additionally, longer examination time and extra materials increase the costs, limiting its use in the cardiologic diagnostic practice.
Concerning image quality, IVUS has some limitations evaluating plaques with a great amount of calcification, impairing the visualization behind calcium. Additionally, some plaque structures may exhibit very similar echogenicity characteristics making it impossible to differentiate them, for example, thrombi and lipid component [2]. Finally, IVUS resolution is insufficient to measure the thickness of the fibrous cap; consequently TCFA is defined based on the identification of the necrotic core compressing the lumen.
Optical Coherence Tomography
Usually OCT is considered an alternative or complement to IVUS. Its great advantage comparing to IVUS is its spatial resolution (10–15 mc vs 100–150 mcm). The excellent resolution allows OCT to evaluate the atheroma layer in detail, being the only method capable of measuring in vivo the thickness of the layer and objectively defining TCFA (<65 mcm). Additionally, OCT allows the evaluation of the integrity of the cap, classifying culprit lesions as disrupted fibrous cap (with lipid predominance or calcified nodule) and intact fibrous cap [10]. In patients with ACS, those whose culprit lesion has uninterrupted fibrous cap instead of disrupted have a better prognosis over time, with a lower incidence of death, heart attack, and hospitalization [11].
There are several plaque vulnerability features besides TCFA which can be evaluated accurately by OCT such as plaque composition, macrophages wall infiltrate, microcalcifications, neovascularization, and thrombus. All those features are usual findings in patients with ACS [12–14].
Like IVUS, OCT has been used in planning, guiding, and following PCI. As well as IVUS-guided procedures, using OCT showed to reduce the risk of cardiac death or acute myocardial infarction compared to the angiography-guided procedures [15]. Its excellent spatial resolution allows an excellent plaque characterization, identifying stent malapposition, stent edge, dissection, tissue prolapse, and thrombus [15, 16]. However, the assessment of lumen size after the procedure (minimal lumen area) measured by OCT is significantly lower than that measured by IVUS. This may result in a suboptimal stent expansion in OCT-guided procedures, increasing the chances of late complications such as stent thrombosis or restenosis [16]. The indications for OCT-guided PCI still need stronger randomized controlled trials to support them and should be restricted to cases with greater complexity or with stent failure suspicion [9].
Limitations
OCT imaging requires the use of contrast media to displace blood from the vessel lumen on the segment to be examined. This significantly increase the amount of contrast usually used in angiography. Another limitation imposed by red blood cells is the inability of OCT to visualize red thrombus.
The main disadvantage of OCT comparing to IVUS is the reduced image deep penetration (1–2 mm), making it impossible to fully evaluate plaque composition and the voluminous plaque necrotic core [13]. Reduced deep analysis limits the ability of assessing positive remodeling by OCT, an important plaque vulnerable feature perfectly evaluated by IVUS [13]. Recently, the advent of catheters with the two intracoronary imaging modalities IVUS and OCT promises to associate the high resolution of the OCT to evaluate the cap thickness with the best IVUS image depth for assessing the necrotic core and plaque burden. The combination of both would fully evaluate coronary plaque without dispensing the invasive approach, contrast media usage, and ionizing radiation exposure.
Noninvasive Diagnostic Methods to Assess Coronary Wall
Magnetic Resonance
The first high-resolution magnetic resonance imaging study (MRI) of human arteries was published by Martin et al. in 1995 [17]. Martin studied segments of the carotid, femoral, and aortic arteries and compared MRI findings with histological exams [17]. This study contributed significantly to developing arterial wall imaging techniques to reproduce such images in vivo and stimulated researchers to pursue studying coronary artery walls by MRI. The use of MRI for the evaluation of coronary arteries became clinically feasible after the advent of the latest-generation scanners, allowing faster acquisition sequences and better image quality. Coronary wall evaluation by MRI is safe and noninvasive, does not expose the patient to ionizing radiation, and often does not need any form of contrast medium. These features make coronary wall MRI a promising diagnostic tool for the large-scale evaluation of suspected or known CAD individuals as well as evaluating coronary involvement of inflammatory pathologies.
After a long period of technological advances with emerging new-generation scanners and improvements of MRI sequences, in 2000 Fayad et al. [18] and Botnar et al. [19] published their studies on the use of MRI for the evaluation of coronary artery wall in vivo. They used T2-weighted sequences to assess the coronary artery wall characteristics without the use of contrast media. Coronary segments with atherosclerotic plaques by angiography showed greater vessel area and wall thickness on MRI compared to normal segments in the same patients [18, 19]. These findings boosted the use of MRI to assess coronary wall features in different clinical scenarios.
Coronary MRI demonstrated to be able to identify atherosclerosis in early stages, before significant luminal reduction is established (<50% stenosis). Segments with atherosclerosis presented increased wall thickness and increased wall area compared to healthy coronary segments on angiography [20]. MRI outer vessel area and plaque burden showed good correlation with IVUS [21]. However, coronary wall thickness assessed by MRI demonstrated low correlation with IVUS [22]. Besides identifying atherosclerotic plaques, an important role of MRI is identifying high-risk plaques and their vulnerable features. These plaques are characterized by a large lipid core, positive remodeling, a thin fibrous cap, and a high-inflammatory component being prone to rupture.
In order to assess high-risk plaques, different MRI techniques are available. The measurement of vessel wall signal intensity using T1-weighted three-dimensional black-blood gradient sequences without contrast-medium injection was validated in carotid arteries. High-intensity signal (HIS) in the carotid wall was associated with a high-risk plaque, intraplate thrombus, or hemorrhage assessed by histological exams [23–25]. This approach was used in patients with significant coronary stenosis (>70%), and HIS plaques had a high frequency of ultrasound attenuation, low CT density, and a high incidence of transient slow flow phenomena [26, 27]. Furthermore, the location of HIS in the coronary lumen or intrawall was also related to important features of plaque vulnerability [27]. Masumoto et al. [28] compared OCT findings in patients with angina pectoris and showed that thrombus and intimal vasculature were associated with intraluminal HIS. In contrast, intrawall HIS was associated with macrophage infiltration and absence of calcification [28].
Another non-contrast MRI ability is to identify methemoglobin in coronary wall using T1-weighted black-blood sequences. Methemoglobin is visualized in acute thrombus and intraplaque hemorrhages [26, 29], an important plaque vulnerability feature present in patients ongoing acute coronary syndrome [30, 31].
These combined techniques allow non-enhanced MRI to assess coronary wall thickness, vascular remodeling, plaque burden, and intraplaque hemorrhage or thrombus. These characteristics are known as vulnerable plaque features with significant clinical impact. Patients with HIS plaques have higher probability of MACE [32].
Beyond these non-contrast techniques, MRI can also evaluate coronary artery wall through images acquired after contrast injection (gadolinium). The technique shares the same principles of late gadolinium enhancement for evaluation of myocardial fibrosis. The pathophysiological pathway is based on the theory that there is a rupture of the cell membrane and the expansion of extracellular space by collagen in the fibrosis process. Providing gadolinium is an extracellular contrast, enlarged extracellular space will increase the contrast amount in those areas and extend the contrast wash out time. Late images acquired after gadolinium injection will enhance in fibrotic regions. Histological study of carotid plaques demonstrated that contrast enhancement was associated with neovascularization of the fibrous cap, increased endothelial permeability, and infiltration of inflammatory cells [33].
Early reports using T1-weighted images demonstrated that coronary wall contrast enhancement is strongly associated with vascular remodeling and atherosclerosis severity [29, 34]. Coronary wall enhanced areas by MRI correspond predominantly to mixed plaques by computed tomography angiography (CTA) [34]. In the setting of chronic coronary artery disease, contrast uptake in the coronary wall might be associated with neovascularization, endothelial permeability, and infiltration of inflammatory cells [29, 34].
Patients with ACS had significantly greater contrast uptake in the coronary wall of culprit lesions [35, 36]. However, long-term follow-up of these patients showed that the enhancement decreased 3 months after reperfusion [35]. This finding suggests that edema and the inflammatory process present in ACS have a significant role in this phenomenon and that enhancement of the coronary wall may be a surrogate biomarker of plaque activity and/or vulnerability [35, 36].
Delayed enhancement MRI can be useful for the evaluation of coronary wall involvement in several inflammatory diseases. Puntmann et al. [37] showed that patients with systemic lupus erythematosus at clinical remission have a higher signal intensity measured by contrast noise ratio on the coronary wall compared to control subjects [37]. In another study of the same group, they demonstrated that patients with systemic lupus erythematosus presented contrast enhancement in a diffuse pattern while patients with CAD had a regional distribution, but both had contrast noise ratio values higher than control patients [38]. In Takayasu’s arteritis, the delay enhancement of the coronary wall seems to have the same distribution as segments with CAD [39].
Limitations
The image acquisition of coronary arteries is a challenge for any noninvasive imaging method, especially MRI. Some of the reasons for that lie in the fact that coronary arteries have reduced caliber and tortuous trajectory and are subjected to heart and respiratory movements. New-generation scanners with optimized sequences allow faster exams, minimizing cardiac cycle and respiratory movement artifacts while maintaining adequate image quality. Another variable that compromises coronary MRI quality is the distance between MRI coil, positioned on the thoracic wall, and the coronary arteries. The greater the distance, the lower the noise signal ratio and worse image quality. Finally, the maximum spatial resolution obtained by the MRI (0.65 × 0.65 mm) is insufficient compared to those available by the IVUS (<0.1 mm) or even CTA (0.35 × 0.35 × 0.35 mm). MRI resolution allows a satisfactory analysis only for segments with greater caliber and restricting its evaluation to the proximal or middle coronary segments [40].
Computed Tomography Angiography
Computed tomography angiography has raised as an emerging diagnostic tool in the evaluation of coronary arteries in the past years. Coronary CTA allows the evaluation of several cardiac structures in a single acquisition such as the coronary arteries lumen, coronary wall, coronary adjacent structures (pericoronary fat and pericardium), myocardial perfusion, and functional and anatomical heart structures. These evaluations are possible using a single contrast-medium injection. The overall assessment of heart structure and function became possible by the evolution of scanners and the reconstruction algorithms. New equipment with a larger number of detectors (up to 320 detectors) and dual source energy scanners significantly improved spatial and temporal resolution, as well as reducing radiation exposure and the need of larger volumes of iodinated contrast [41].
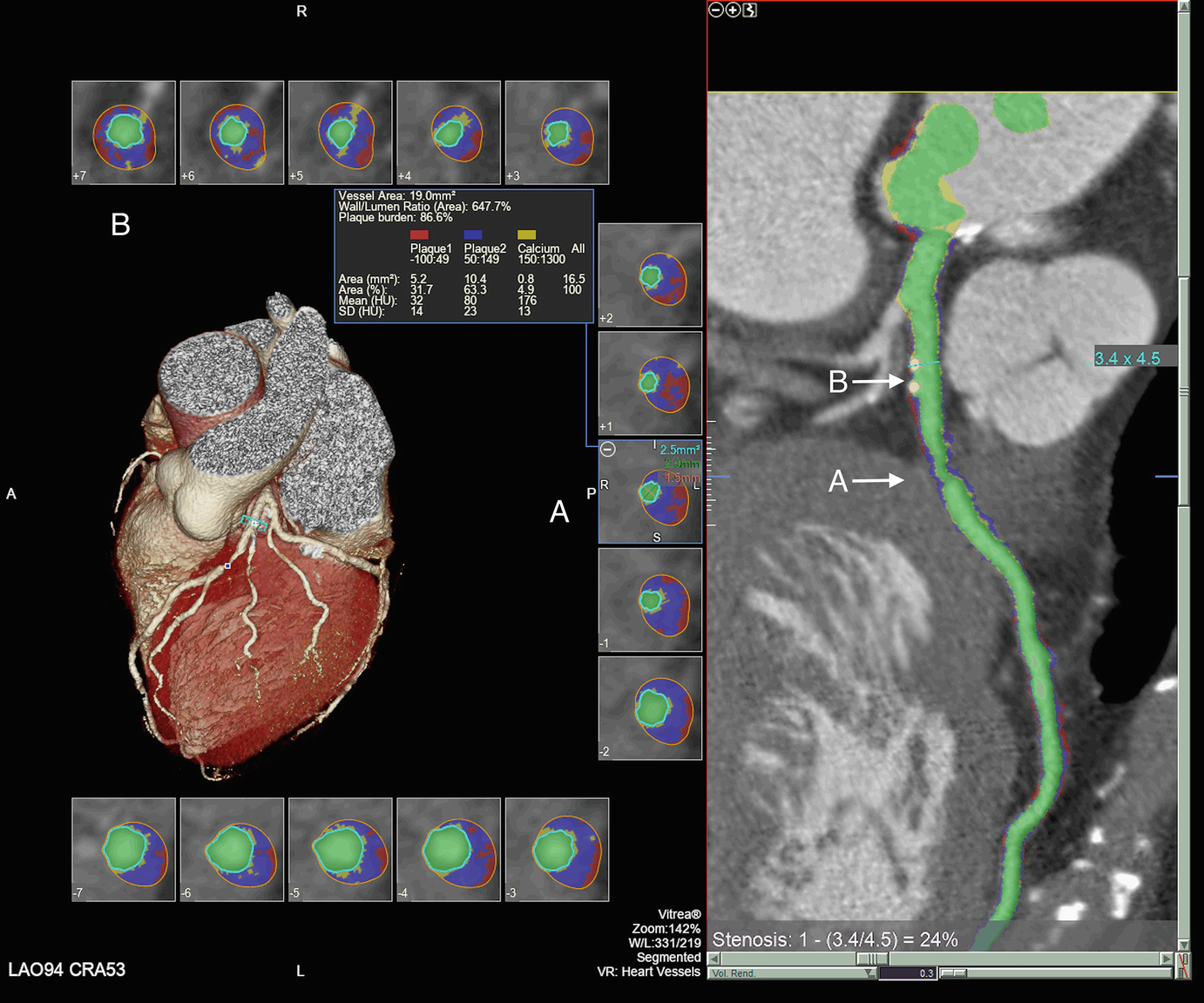
Coronary computed tomography angiography with simultaneous visualization of the three-dimensional anatomy of the heart and coronary arteries, visualization of the coronary artery lumen in curved multiplanar reconstruction, and transverse images of the coronary artery with lumen and artery wall visualization. Cross-sectional analysis of the artery allows the evaluation of the characteristics of each slice and identification of segments with lumen stenosis (A) as well as segments apparently normal to angiography (B) but with atherosclerotic involvement identified by tomography

Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree








