Fig. 19.1
Glenoid component loosening with radiolucent lines
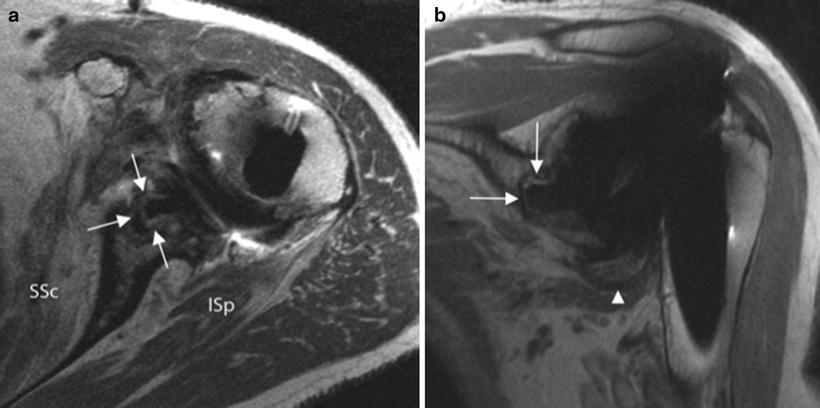
Fig. 19.2
Axial (a) and coronal oblique (b) FSE PD images demonstrate circumferential hyperintense signal with adjacent thin low-signal rim about the glenoid baseplate and keel indicative of loosening (arrows) in two different patients. Wear-induced synovitis is detected on the coronal oblique image at the axillary recess (arrowhead)
Patient then underwent arthroscopic removal of a loose glenoid component (Fig. 19.3a–c). The component was removed through the rotator interval. At the time of arthroscopy, biopsies were taken for culture and were held for 14 days in order to rule out an indolent infection with P. acnes. These were negative. The patient went on to pain-free range of motion and elected not to undergo another procedure for glenoid reimplantation.
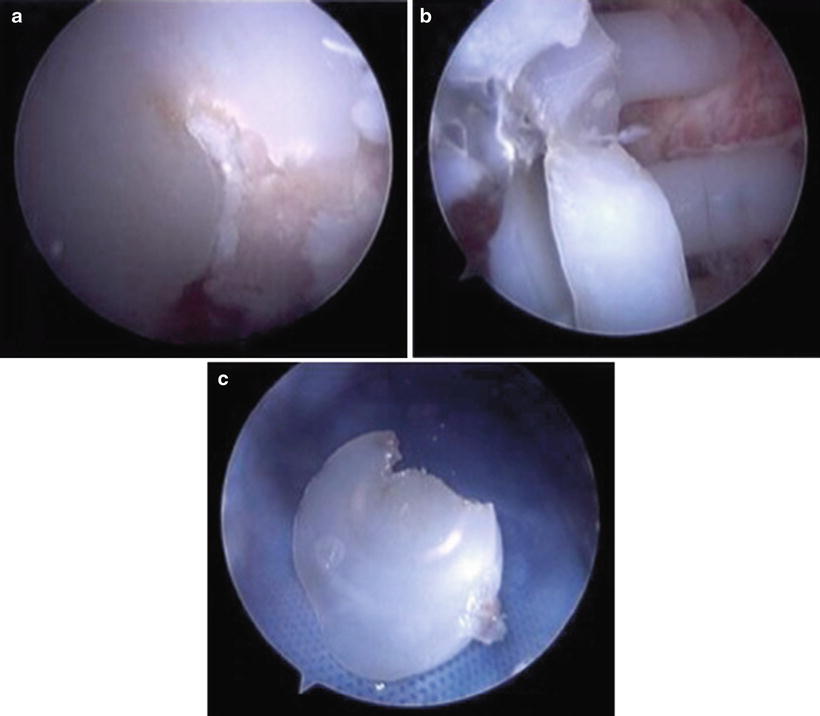
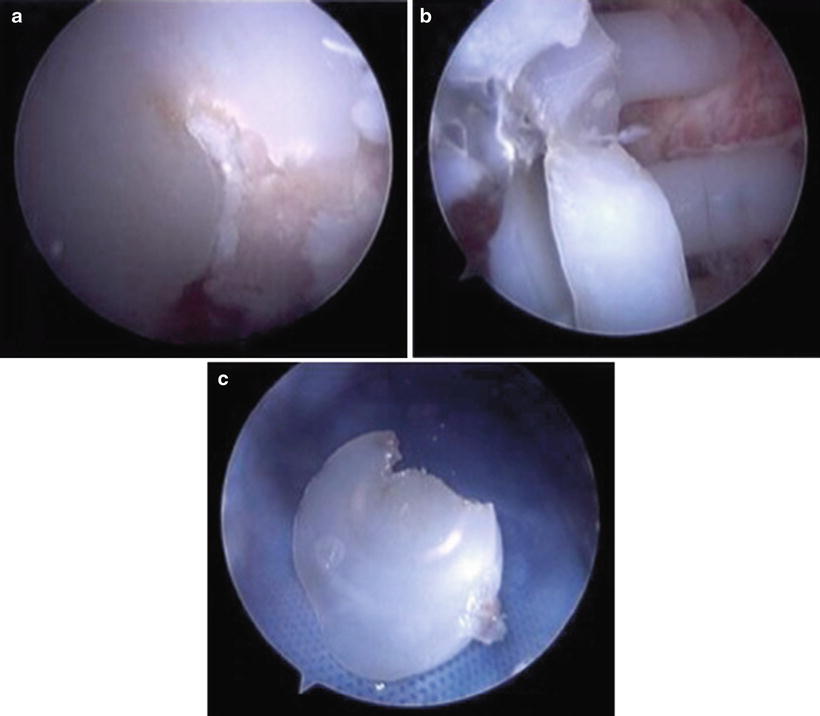
Fig. 19.3
(a) Arthroscopic images while viewing from a posterior portal of a cracked and loose glenoid. (b) Glenoid was easily removed arthroscopically through an incision made in the rotator interval. (c) View of the glenoid on the back table after removal
In the analysis by Bohsali et al., loosening of the glenoid and humeral components occurred frequently, accounting for 39 % of complications [8, 18–20]. Moreover, 83 % of the cases of loosening involved failure of the glenoid component fixation. Loosening of an arthroplasty component is recognized on radiographs as the appearance of a radiolucent line at the implant/cement/bone interface. Line thickness is measured starting with 0.5 mm. The sites of appearance have been divided into eight zones for the humeral component and six zones for the glenoid component [21–24]. Franklin et al. [25] devised criteria to classify radiolucency around the glenoid component for keeled implants (Table 19.1). Similarly, Lazarus et al. [26] developed a classification for pegged implants. For glenoid components, the overall prevalence of radiolucent lines is reported to range from 22 to 95 % [2, 7, 27–29]. However, relying solely on plain radiographs to determine security of fixation may be problematic because obtaining reproducible X-rays of the glenoid can be difficult [30]. Nagels et al. [31] performed a study of loosening of the glenoid component using digital roentgen stereophotogrammetric analysis and found that it was more accurate in detecting early loosening. Its use in practice, however, is limited to the lack of experience and familiarity with the technique.
Table 19.1
Classification of radiolucency around keeled glenoid components
Grade 0 | No radiolucency |
Grade 1 | Radiolucency at superior and/or inferior flange |
Grade 2 | Incomplete radiolucency at keel |
Grade 3 | Complete radiolucency (≤2 mm wide) around keel |
Grade 4 | Complete radiolucency (>2 mm wide) around keel |
Grade 5 | Gross loosening |
In reverse total shoulder arthroplasty, scapular notching is another glenoid complication that can lead to implant failure. This term describes a common complication involving the erosion of the inferior scapular neck related to impingement by the medial rim of the humeral cup during adduction [32–38]. A large multicenter trial found an incidence of 68 % at a mean follow-up of 51 months. It was also shown that notching was accompanied by decreases in strength and anterior elevation as well as an increased incidence in humeral and glenoid radiolucent lines [39]. Nyffeler et al. [40] concluded inferior placement of the baseplate on the glenoid plate to prevent the occurrence of notching and also improve range of motion. Glenospheres with a lateral center of rotation have been shown to produce lower rates of scapular notching [41–43].
With regard to the prosthetic humeral head, analyzing its position relative to the greater tuberosity and the shift of the stem in the frontal plane can identify a humeral component at risk or not at risk of loosening [44]. For additional precision in measuring shift of the stem, authors have devised various terminologies. Subsidence (S) describes the change in the vertical distance between the most superior aspects of the humeral component and the greater tuberosity [22]. The tilt is the medial or lateral change in the components’ position measured by calculating the distance of the external surface of the humeral component from the external surface of cortical bone in four areas: superolateral (at the border between radiographic zones 1 and 2), inferolateral (zones 2 and 3), superomedial (zones 6 and 7), and inferomedial (zones 5 and 6) [22, 45]. Clinically relevant threshold amounts for subsidence and tilt in humeral component position are ≥5 mm and ≥10 mm, respectively [44].
Instability
Shoulder arthroplasty can disturb the complex interplay of bony and soft tissue restraints of the glenohumeral joint. Instability following shoulder arthroplasty is a common complication with a reported prevalence of 4 % and accounts for 30 % of all complications across multiple studies [8, 18, 19, 46, 47]. Specifically, anterior and superior instability accounted for 80 % of the cases of instability [8, 18, 19, 46, 47]. Superior instability is associated with a deficient rotator cuff or coracoacromial arch [4, 28, 48, 49]. Attributable causes to anterior stability include humeral component malrotation, anterior glenoid deficiency, anterior deltoid muscle dysfunction, and failure of the subscapularis tendon and anterior aspect of the capsule [5, 46, 50].
Plain radiographs can be used to assess prosthesis instability. The axillary radiograph is the gold standard to assess subluxation of the prosthetic head in the sagittal plane. Furthermore, the degree of subluxation can be classified as either absent, slight, moderate, or severe based on the direction and severity (Table 19.2) [20]. Joint widening on the true AP views may also indicate instability, possibly due to an undersized humeral component, an excessive osteotomy, or a deficient rotator cuff [44].
Table 19.2
Classification of prosthetic head subluxation
Absent | The humeral head is centered in the glenoid cavity |
Slight | <25 % translation of the center of the head component with respect to the glenoid center |
Moderate | 25–50 % translation of the center of the prosthetic head with respect to the glenoid center |
Severe | >50 % translation of the center of the head component with respect to the glenoid center |
Failure of the subscapularis tendon is implicated in many cases of anterior instability following TSA [51–53], but clear visualization is difficult due to metal artifact. Ultrasound can be extremely accurate in the detection of rotator cuff tears in the postoperative shoulder (Fig. 19.4) [54, 55]. In a study documenting the subscapularis healing rate by the use of postoperative ultrasound after TSA in 30 patients, ultrasound identified four torn tendons, whereas there were no radiographic findings definitively associated with the absence of intact subscapularis tendons [56]. A study by Sofka et al. of 11 shoulder arthroplasty revealed six subscapularis tears [57].
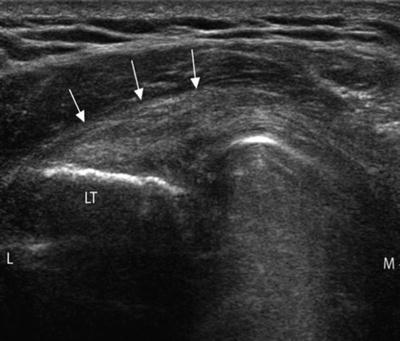
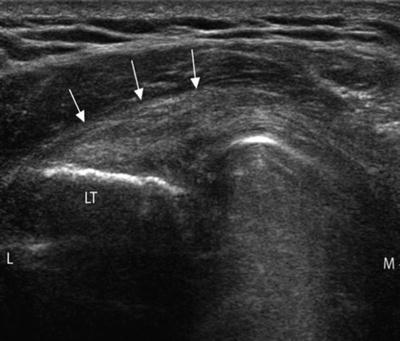
Fig. 19.4
Ultrasound image depicts an intact subscapularis tendon (arrows) in the long axis. LT lesser tuberosity, L lateral, M medial
Posterior instability is normally a result of excessive component retroversion [8, 50, 58, 59]. Consequently, posterior glenoid erosion and soft tissue imbalance lead to instability [8]. Posterior subluxation can be seen on the axillary radiograph (Fig. 19.5). A CT can also be used to determine glenoid version accurately [54].


Fig. 19.5
Axillary radiograph showing posterior subluxation of the humeral head component secondary to eccentric posterior glenoid wear
Periprosthetic Fracture
The reported prevalence of periprosthetic humeral fractures has been estimated to be between 1.5 and 3 % [5, 46, 60]. Initial evaluation of a suspected fracture in a patient should include anteroposterior and axillary radiographs. Cofield and Wright developed a classification system for humeral periprosthetic fractures [61]. Type A fractures occur at the tip of the prosthesis and extend proximally. Type B fractures occur at the tip of the prosthesis without extension. Type C fractures occur at the prosthetic tip and have distal extension [62].
Rotator Cuff Tear
Case 2
A 73 year-old right-hand-dominate male who originally underwent a right total shoulder replacement at an outside hospital approximately 18 months prior to presentation with pain and limited function. Physical exam revealed pseuodoparalysis with attempted elevation and anterosuperior escape. Radiographs show superior and anterior subluxation (Fig. 19.6a, b), and MRI showed subscapularis dehiscence with retraction to the coracoid (Fig. 19.7) and fatty infiltration of the muscle belly.
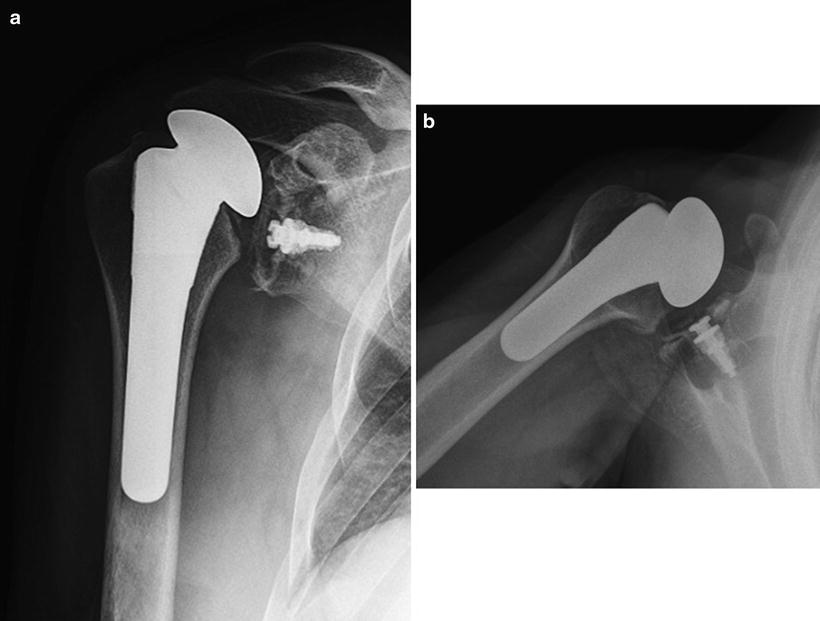
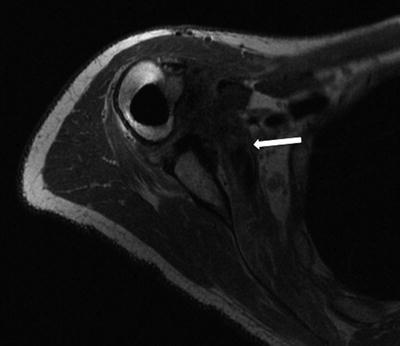
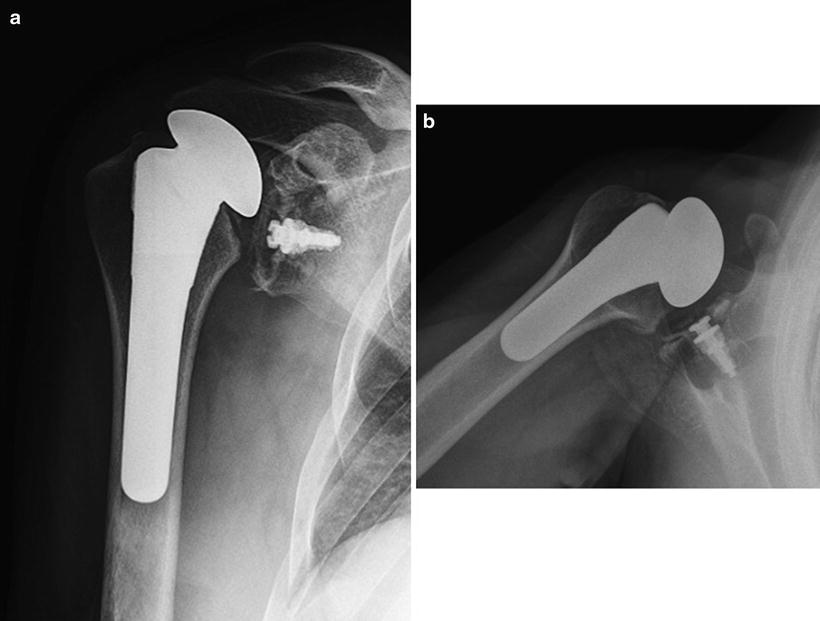
Fig. 19.6
Anteroposterior (a) radiograph shows superior migration of the humeral head, and the axillary (b) shows anterior subluxation. Both indicative of a rotator cuff tear
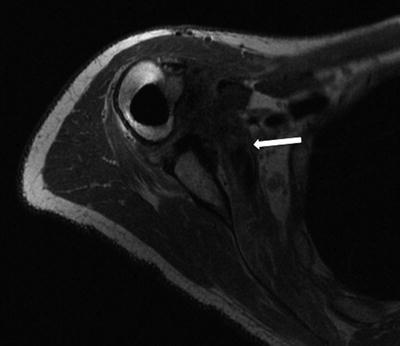
Fig. 19.7
MRI showing dehiscence of the subscapularis with retraction of the main tendon stump past the coracoid (arrow)
Patient underwent conversion of his total shoulder replacement to a reverse shoulder arthroplasty (Fig. 19.8). Four years later the patient now has 150° of forward flexion, 15° of external rotation, and internal rotation to the back pocket all with minimal pain.


Fig. 19.8
Anteroposterior radiograph after conversion of the total shoulder replacement to a reverse shoulder arthroplasty
Rotator cuff tears can be assessed radiographically by observing superior migration of the humeral head and measuring a reduction of the acromio-humeral distance. However, this measurement can be imprecise because it varies according to the projection, size, and sex of the patient. Instead, Skirving [30] advocated the importance of the continuity of the scapulohumeral line (analogous to Shenton’s line in the hip) on a true AP of the shoulder taken with the arm in neutral or external rotation. When there is a break in this line, it is a more sensitive indicator of superior migration of the humeral head and, therefore, of rotator cuff tears. Despite these findings, plain radiographs have limited ability to assess the integrity of the cuff, the quality of the muscle, and the degree of retraction of a torn tendon.
Consequently, MRI has been relied upon to provide a more accurate diagnosis in the face of clinical and conventional imaging limitations [63]. MRI, however, presents its own particular set of imaging challenges in shoulder arthroplasty due to the magnetic susceptibility generated by the implant resulting in local field distortions that obscure the regional structures. The intensity of the susceptibility artifact is a function of the relative ferromagnetism of the components, with titanium being less ferromagnetic (and thus causing less artifact) than cobalt-chrome alloy components, as well as the orientation of the components relative to the external magnetic field. Additionally, the eccentric location of the shoulder relative to the isocenter of the imaging bore and the large spherical component increase the susceptibility artifact of shoulder arthroplasty when compared to knee or hip arthroplasty [63, 64].
Modifications in conventional fast spin echo techniques have improved visualization of the soft tissues around implants. In an MRI study of 42 painful shoulder arthroplasties, Sperling et al. [63] suggested that MR imaging is a useful tool to determine the integrity of the rotator cuff; however, they found that the lesser tuberosity and glenoid component were obscured by artifact created by the proximal spherical humeral component. Relatively new commercially available pulse sequences, multiacquisition variable-resonance image combination (MAVRIC) and slice-encoding metal artifact correction (SEMAC), can further reduce susceptibility artifact near implants [65–67]. These new pulse sequences rely on conventional imaging techniques and can be used with standard clinical 1.5-T and 3-T MRI hardware.
Early studies have shown that MAVRIC images can detect pathology not visible with standard metal artifact-reduction FSE sequences. Hayter et al. [65] evaluated the quality of MAVRIC images compared with that of metal artifact-reduction FSE images of 27 patients who underwent shoulder arthroplasty. Their findings included significantly improved visualization of the synovium, periprosthetic bone, glenoid osteolysis, and supraspinatus tendon. Importantly, detection of supraspinatus tears was significantly increased with MAVRIC compared with FSE imaging alone (Fig. 19.9a, b). Although the lesser tuberosity and subscapularis footprint often remain obscured, the muscle tendon junction and its muscle belly are typically visualized and should be carefully evaluated for failure, as this is a common cause of anterior instability. Application of MAVRIC or SEMAC to axial images could potentially better elucidate subscapularis tears at the footprint (Fig. 19.7).
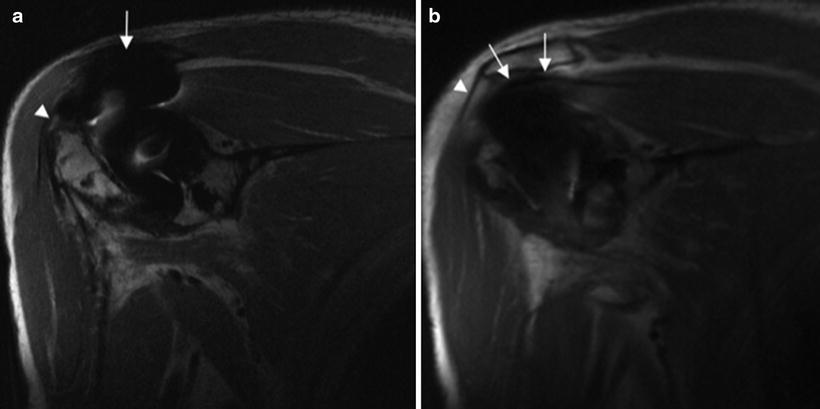
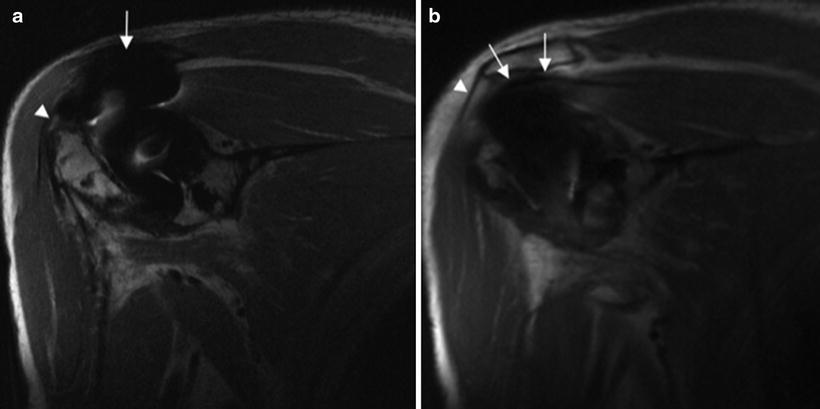
Fig. 19.9
(a) Coronal oblique FSE proton density image demonstrates bulky dephasing artifact superiorly obstructing the supraspinatus muscle tendon junction (arrow). Note that the supraspinatus footprint (arrowhead) remains visualized, which is hyperintense in this case indicating tendinosis but no tear. (b) Coronal oblique MAVRIC FSE proton density image allows visualization of the supraspinatus muscle tendon junction (arrows), thereby increasing the ability to detect supraspinatus tendon tears and retraction. Note the ability to see the origin of the deltoid (arrowhead)
By decreasing image distortion and improving visualization of the bone-prosthesis interface, these new metal reduction techniques (MAVRIC/SEMAC) serve to complement conventional FSE images, which ultimately offer higher spatial resolution than MAVRIC images, thus providing greater detail of the visualized soft tissues [65].
Similar to MRI, ultrasound is able to assess periarticular soft tissues without radiation; however, sonography has the added benefits of eliminating interference from the implant and allowing dynamic examinations. Westhoff et al. [68] performed static and dynamic ultrasound examinations on 22 patients, and results were correlated with clinical outcome. Pathologic changes within the supraspinatus and infraspinatus tendons were found in several shoulders. A halo sign around the biceps tendon was detected in seven shoulders (Fig. 19.10). This low-echogenic halo around the biceps tendon correlated well with fluid in the synovial sheath and indicated effusion within the glenohumeral joint according to a study by Rupp et al. [69] Increased intra-articular volume was detected in five patients, two of whom also had a halo sign around the biceps tendon. Subdeltoid bursitis was found in only one shoulder. Loosening of the glenoid during dynamic examination was detected in one shoulder. Pathological findings also correlated well with poorer outcomes, while lack of findings correlated with better outcomes.
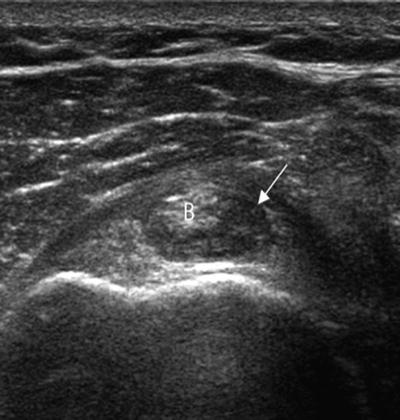
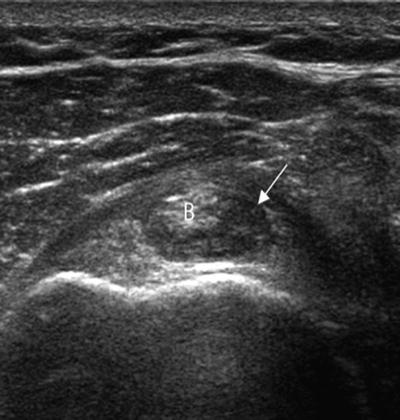
Fig. 19.10
Ultrasound image demonstrates the long head of the biceps tendon (B) in short axis with a hypoechoic rim of synovial fluid and debris (arrow)—“halo” sign
Sofka and Adler [57] performed ultrasound examinations on 11 shoulder arthroplasty patients who had clinical suspicion of rotator cuff tear, pain, and decreased range of motion. Sonographic findings included six supraspinatus tendon tears and three infraspinatus tendon tears. Nine patients had biceps tendinosis. The prosthesis did not hinder examination of the rotator cuff in any patient (Fig. 19.11). The authors concluded that sonography is a rapid and reliable method to use for evaluating the periprosthetic soft tissues, including the rotator cuff, in patients who have undergone shoulder replacement. Disadvantages of ultrasound are that it does not give a global picture of the joint and it provides limited evaluation of component loosening [70].
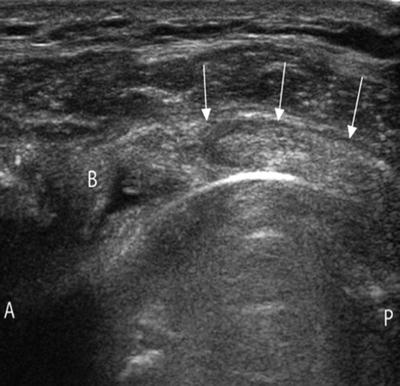
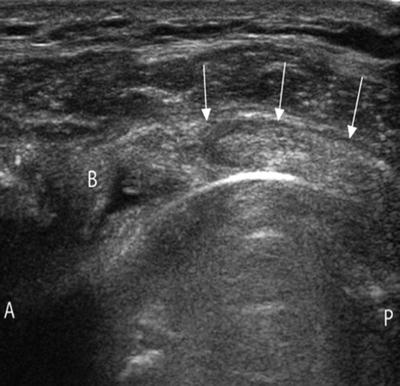
Fig. 19.11
Short axis ultrasound image shows an intact supraspinatus tendon (arrows). The hyperechoic curvilinear line deep to the supraspinatus is the humeral component. B biceps long head tendon
Despite the relatively common use of MRI and ultrasound for evaluation of most soft tissue shoulder abnormalities, CT arthrography can also provide an accurate assessment of the rotator cuff, the capsular-labral-ligamentous structures, and the articular cartilage of the glenohumeral joint [71, 72]. Multi-detector CT (MDCT) is a development that has provided excellent spatial resolution and multiplanar capability, thus markedly improving the diagnostic power of CT arthrography of the shoulder [73]. Some authors [74, 75] prefer MDCT arthrography for imaging patients with shoulder prostheses because the images have minimal artifacts while allowing sufficient assessment of prosthetic and periprosthetic bony and soft tissue abnormalities. Post-processing of volume-rendered 3D CT can also substantially reduce beam-hardening artifacts and can be used to assess hardware integrity [76]. Additionally, joint fluid can be aspirated during the intra-articular administration of contrast medium and sent for culture and sensitivity testing if clinical suspicion of infection warrants [77]. General indications for MDCT arthrography pertain to the inability to perform MRI or failure of MRI to adequately evaluate the shoulder. For example, indications include the presence of metal hardware close to the joint, the presence of MRI-incompatible implanted medical devices, and a history of claustrophobia. In patients who have undergone shoulder surgery, MDCT arthrography has been found to be more accurate than nonarthrographic MRI [78]. However, to date there has not been a direct comparison of MDCT arthrography and MR arthrography.
Infection
Although infection is a rare complication of primary shoulder arthroplasty, it can have devastating consequences. Bohsali [8] found an overall prevalence of 0.7 % across several studies. Susceptible host-related factors for infection include diabetes, rheumatoid arthritis, systemic lupus erythematosus, previous surgery, and remote sources of infection. Extrinsic causes of infection include chemotherapy, systemic corticosteroid therapy, and repeated intra-articular steroid injections [5, 46].
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree








