- Andrea. Schwartz Doria, MD, PhD, MSc
- Paul. Babyn, MDCM
Key Facts
- •
Juvenile idiopathic arthritis (JIA) comprises arthritides of unknown etiology that begin before age 16 years and that persist for greater than 6 weeks.
- •
Ultrasonography is a very useful modality in children because of its ability to detect joint effusions and pannus and measure cartilage thickness, all without ionizing radiation.
- •
Magnetic resonance imaging (MRI) can document erosion not visible on radiographs and can determine the presence and activity (vascularity) of pannus.
- •
Complications of JIA include growth abnormalities, amyloidosis, uveitis (especially in patients with oligoarticular disease), and the macrophage activation syndrome.
- •
Enthesitis-related arthritis refers to arthritis accompanied by enthesitis (inflammation at the sites of attachment of ligaments or tendons to bone). Also included are those conditions with either arthritis or enthesitis plus two of the following: (1) sacroiliac joint tenderness and/or inflammatory spinal pain; (2) presence of HLA-B27; (3) family history of HLA-B27–positive disease; (4) acute anterior uveitis; or (5) onset of arthritis in a boy older than 8 years.
- •
The diagnosis of psoriatic arthritis in children includes children with arthritis and psoriasis or those with arthritis and at least two of the following: (1) dactylitis; (2) nail pitting or onycholysis; or (3) family history of psoriasis in a first-degree relative. Girls are most often affected.
- •
Arthritis occurs in about 10% of patients with inflammatory bowel disease. The sacroiliitis and spondylitis may progress despite control of the bowel disease. The peripheral joint disease activity mirrors the activity of the bowel disease.
- •
Suspicion of a septic joint generally requires aspiration. Radiographs are usually performed for initial evaluation. MRI is usually more sensitive than computed tomography or scintigraphy for the detection of changes suggesting septic arthritis.
- •
Transient synovitis of the hip is an acute, self-limited condition of unknown origin and is most commonly seen in boys between the ages of 3 and 6 years. It usually affects one joint but can be bilateral in up to 5% of cases. Ultrasound, rather than radiography, may be the method of choice for initial evaluation.
- •
Hemophilic arthropathy produces fairly specific findings on imaging studies. Low-signal synovitis is due to hemosiderin within the hypertrophied synovium and is a characteristic but not an entirely specific feature of the disease.
Imaging often plays a key role in establishing the presence of arthropathy, determining its extent, and defining the specific diagnosis. Previously, radiography was the principal method used to evaluate and follow bone damage in patients with inflammatory arthritis. More recently the use of magnetic resonance imaging (MRI) and ultrasonography have gained wider acceptance due to their multiplanar capabilities. Arthrography is not commonly used in imaging of arthritis in children because less invasive modalities are available that also have the ability to image both bone and soft tissue abnormalities.
Most synovial joints undergo significant osseous development and maturation in early childhood. In the newborn, extensive unossified epiphyseal cartilage limits radiographic joint assessment because the unossified cartilage cannot be distinguished from adjacent soft tissues. Epiphyseal cartilage transforms to bone with increasing age, narrowing the radiographic joint space to the thickness of the opposing layers of articular cartilage.
Normal articular soft tissue components have a similar radiographic density and cannot be clearly differentiated from each other or from adjacent muscles, fascia, tendons, ligaments, nerves, or vessels by radiography. However, displacement of fat deposits in fascial and intermuscular planes assists in the determination of joint effusions in the elbow, knee, and ankle.
This chapter discusses the imaging modalities that are currently available for evaluation of children with arthropathy, including ultrasonography and MRI, and presents the imaging features of common causes of acute and chronic arthritis.
INFLAMMATORY ARTHRITIS
Juvenile Idiopathic Arthritis
The term juvenile idiopathic arthritis (JIA) comprises arthritides of unknown etiology that begin before age 16 years and that persist for greater than 6 weeks. Classification into subtypes (systemic, oligoarthritis, polyarthritis with negative and positive rheumatoid factors, psoriatic arthritis and enthesitis-related arthritis, other arthritis) within this overall term is based on the clinical characteristics of the disease rather than on any understanding of the underlying pathology.
JIA is the most important rheumatic disease affecting children and one of the most common chronic diseases of childhood. Although JIA may be self-limited with a majority of patients having no active synovitis in adulthood, many children have significant joint complications.
In JIA the synovium is the target tissue for inflammation. Early in the disease course the affected joints are clinically swollen, stiff, painful, and warm and show limited motion. There is synovial proliferation and infiltration by inflammatory cells including polymorphonuclear leukocytes, lymphocytes, and plasma cells and increased secretion of synovial fluid with development of synovial thickening and pannus formation. Inflammation of synovial coverings of tendons and bursa, which can also be affected, can lead to periostitis. With prolonged inflammation, destruction of cartilage, adjacent bone erosions, and even joint ankylosis may be seen.
Imaging
Osteoarticular Imaging Features
Imaging can be used to determine whether arthritis is indeed present, establish a specific diagnosis, and determine the extent of disease. It may also be used to determine disease activity, detect disease complications, evaluate disease progression, and judge efficacy of drug treatment.
Radiography
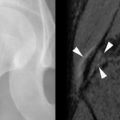
Radiographs of symptomatic areas should be obtained at initial presentation to exclude other differential diagnoses and assist in the diagnosis of arthritis ( Box 24-1 ). In early arthritis, radiography is often of limited utility, as the inflamed synovium, soft tissue changes, and cartilage erosions that precede bone erosions are not well seen. Initial radiographs are often nonspecific, reflecting early response of the soft tissues and bones to inflammation with soft tissue swelling, osteopenia, joint effusions, and periosteal reaction ( Figure 24-1 ). The osteopenia is initially periarticular, becoming more diffuse with time. Rarely one sees the band-like pattern observed in leukemia. Periosteal reaction is commonly seen in the phalanges, metacarpals (see Figure 24-1 ), and metatarsals but can also occur in the long bones.
ALIGNMENT
Atlantoaxial subluxation
Coxa valga
BONE DENSITY
Juxtaarticular osteoporosis
Diffuse osteoporosis (late)
Metaphyseal lucencies (rarely)
Periosteal reaction adjacent to affected small joints
CARTILAGE SPACES
Erosions (late), may appear corticated
Cartilage space narrowing (late)
Ankylosis (especially spine, wrists)
DISTRIBUTION
Monarticular, pauciarticular, or polyarticular
GROWTH ABNORMALITIES
Affected small bones are shorter than normal
Overgrowth (lengthening) of affected long bones
Advanced maturation of affected epiphyses
Large epiphyses
Micrognathia (may have mandibular notching)
Protrusio acetabuli
Fused cervical vertebrae
Angular carpals
Square patella
Intercondylar notch widening (also a feature of hemophilia)
SOFT TISSUES
Effusions and joint distension
Nodules
Periarticular calcification (probably due to corticosteroid injections)









Soft tissue nodules can be noted, as may periarticular calcification (see Figure 24-1 ), although this usually is a consequence of prior intraarticular corticosteroid injection therapy. Joint space narrowing and erosions (see Figure 24-1 ) are typically later radiographic findings seen 2 years or so after the disease onset. However, in rheumatoid factor–positive polyarthritis and in up to one third of patients with systemic arthritis, early erosive disease can occur. Abnormalities in growth and maturation may be present, leading to accelerated osseous growth, altered maturation, and enlarged epiphyses (see Figure 24-1 ).
Late sequelae of JIA are not uncommon and include epiphyseal deformity, abnormal angular carpal bones, widening of the intercondylar notch of knees, and premature fusion of the growth plate with brachydactyly (see Figure 24-1 ). Growth disturbances are more frequent if the onset of the disease is precocious. Other changes include large cyst-like well-corticated erosions, which may be lobulated. Joint space narrowing and osseous erosions are less frequent in JIA than in the adult-onset disease and are usually late manifestations.
Cartilage space narrowing and bone erosion are less frequent and are later findings in JIA than in adult rheumatoid arthritis (RA).
At the hip protrusio acetabuli (see Figure 24-1 ), premature degenerative changes, coxa magna, and coxa valga can be seen. Joint space loss can progress to ankylosis particularly in the apophyseal joints of the cervical spine and in the wrist (see Figure 24-1 ). Subluxation of the joints especially at the wrist (see Figure 24-1 ) may be evident, and atlantoaxial subluxation may also occur. Growth disturbance of the temporomandibular joint may lead to micrognathia and abnormalities of the temporomandibular disk.
Radiographic Scales Available for Assessment of JIA
Despite the limited sensitivity of conventional radiography to early disease, it remains the standard practice technique used for assessment of responsiveness of therapy for JIA in many pediatric centers around the world. Most radiographic classification systems that are currently available to assess the degree of joint destruction in JIA are in fact targeted to changes of RA in adults. Pettersson & Rydholm’s classification method for JIA is objective, is highly reproducible, and correlates well with the clinical status of the disease, but the authors evaluated only a small sample of children with JIA (n = 15) with this scoring system by the time the method was first described. Steinbrocker et al. proposed a four-stage scoring system for evaluation of RA. This system has low sensitivity and reproducibility in part because of the vague description of the changes that qualify for each stage. Although no correlations have been found between hand radiographic findings, which were thought to have prognostic implications, and patient functional disability using this system, this scoring system is the oldest and simplest method described. The methods that are most widely used for assessment of rheumatoid arthritis are the Larsen and Sharp scoring systems with their modifications. Larsen et al. reported a six-graded scoring system based mainly on erosive damage on standard reference radiographs. It is recommended by the European League against Rheumatism (EULAR). In contrast to Steinbrocker’s system, Larsen’s method has proved to be of high reproducibility, despite the fact that the changes noted between two radiographic examinations may not qualify the joint for an increase in stage. The Sharp system assigns separate scores for erosions and joint space narrowing, which are combined to provide the final score.
Ultrasonography
Ultrasonography is widely used in assessing the pediatric musculoskeletal system largely because of its ability to visualize cartilage, which is abundant in the immature skeleton and the absence of ionizing radiation.
Ultrasonography can be used to detect joint effusion, cartilage thickness, and synovitis without ionizing radiation. Ultrasound guidance can be used to guide joint aspiration.
Although total joint assessment is often hindered by acoustic barriers, ultrasonography can be used to assess articular cartilage thickness and to detect synovial thickening, joint effusions, and associated synovial cysts. Ultrasonography is very sensitive in detecting joint effusion in the hips ( Figure 24-2 ) and shoulders, where radiographs are insensitive. Ultrasonographic scoring systems have been recently developed for assessment of finger joint synovitis in RA of adults. Ultrasonography can also be used to assess tendon sheath synovial proliferation (see Figure 24-2 ) and bursal hypertrophy, to evaluate soft tissue nodules (see Figure 24-2 ), and to guide joint aspiration or injection. Although previous studies in JIA have shown that MRI is superior to ultrasonography to evaluate erosions in the articular cartilage of knees, ultrasonography seems to be more sensitive than conventional radiography and clinical assessment, as demonstrated in adult RA. Power Doppler shows promise in evaluating the amount and activity of pannus.



A novel ultrasonographic technique uses intravascular microbubble contrast agents to improve the Doppler signal intensity. Preliminary results of the use of contrast agents in JIA have shown a potential application for the technique in subclinical cases (see Figure 24-2 ); however, the lack of standardized interpretation, increased cost, and greater invasiveness have somewhat limited the use of the technique in clinical practice.
Magnetic Resonance Imaging
With MRI one can directly image synovial proliferation, joint fluid, pannus formation, and erosion of cartilage and bone ( Figure 24-3 ). MRI is suitable to assess disease severity or progression and plays an increasing role in diagnosis and outcome assessment of the disease. Uncomplicated joint fluid has usually dark signal on T1-weighted and bright signal on T2-weighted images (see Figure 24-3 ). Other findings in JIA include popliteal cysts (see Figure 24-2 ) and meniscal hypoplasia (see Figure 24-3 ) or atrophy.



MRI enhancement of the synovium can be used for early detection of synovial proliferation, which precedes destructive changes. Normal synovium is thin and shows slight enhancement. Proliferating synovium on MRI without contrast appears as intermediate soft tissue density on T1-weighted and T2-weighted sequences (see Figure 24-3 ). It may have slightly higher signal intensity than adjacent fluid on unenhanced T1-weighted images. Pannus appears as thickened intermediate to dark signal intensity on T2-weighted images best seen when outlined by bright signal joint fluid. Its variable signal intensity reflects its different amounts of fibrous tissue and hemosiderin.
Synovial thickening may be difficult to define without contrast. Contrast enhancement improves visualization of the thickened synovium especially with the use of fat suppression techniques, which allows the proliferating synovium to be seen in regions normally devoid of synovium appearing as enhancing linear, villous, or nodular tissue. Images should be obtained immediately after contrast injection, as diffusion of contrast from the synovium into the joint fluid occurs over time. Hypervascular inflamed pannus enhances significantly, whereas fibrous inactive pannus shows much less enhancement.
MR images obtained shortly after IV contrast injection demonstrate enhancement of hypervascular-inflamed synovium (pannus) but less enhancement of fibrotic, inactive synovial tissue, thus allowing disease activity to be assessed.
Quantitative techniques may be used to determine synovial volume. MRI is more sensitive than clinical evaluation in detecting temporomandibular joint involvement, demonstrating inflammatory change in the absence of clinical symptoms. There is marked variation in the appearance of the intraarticular disk with age, and a flattened disk should only be considered pathologic in the older child ( Figure 24-4 ).

Hemosiderin deposition can occur in JIA but is more often seen in disorders typically accompanied by hemarthrosis, including pigmented villonodular synovitis, hemophilic arthropathy, synovial hemangioma, and posttraumatic synovitis. Gradient echo sequences are most sensitive in detecting hemosiderin deposition within the synovium with signal loss occurring due to increased magnetic susceptibility.
Hemosiderin containing synovitis appears very low in signal (black) on all MRI sequences, and this is accentuated on gradient echo sequences.
With prolonged synovial inflammation, as in JIA or tuberculosis, well-defined intraarticular nodules termed “rice bodies” (because of their characteristic macroscopic appearance) can be noted. Rice bodies likely arise from detached fragments of hypertrophied synovial villi and may lead to painless swelling of the joint. On MRI, rice bodies have dark signal on T2-weighted images (see Figure 24-3 ) owing to their fibrous tissue composition and are associated with joint effusion, synovial hypertrophy, and synovial enhancement after gadolinium administration.
“Rice bodies” are intraarticular nodules that may develop in JIA or tuberculosis.
Cartilage evaluation is important, as cartilage is one of the earliest sites of damage and destruction in JIA. In the immature skeleton, hyaline and epiphyseal cartilage are better distinguished from each other on fast spin echo (FSE) T2-weighted and fat-suppressed proton density sequences. Cartilage is of bright signal on both of the aforementioned sequences, hyaline cartilage having the highest intensity. The articular cartilage should be assessed for areas of altered signal, thinning, erosions, and deep cartilage loss that may extend to the subchondral bone (see Figure 24-3 ). The fat-suppressed three-dimensional spoiled gradient-recalled echo imaging (3D-SPGR) provides excellent contrast between cartilage, which is of bright signal, compared with adjacent structures. The development of fast imaging methods with increased signal-to-noise ratio (SNR) efficiency and higher cartilage-synovial fluid contrast, such as driven equilibrium Fourier transform (DEFT), dual-echo steady-state (DESS) imaging, Dixon water-fat separation technique, and steady-state free precession (SSFP) imaging have improved the MRI evaluation of cartilage morphology. The advent of 3-Tesla clinical MRI scanners has improved the signal-to-noise and contrast-to-noise ratio efficiencies of the images, enabling detailed identification of very early cartilage abnormalities in adults. Further investigation in the pediatric population should follow.
Scintigraphy
Bone scintigraphy affords high sensitivity but has low specificity for assessment of arthritis because of its lack of spatial resolution. Although previous studies in adults have shown that scintigraphy is effective at detecting synovial inflammation and that scintigraphic evidence of synovitis correlates well with later progression of joint erosions in RA, MRI has replaced to a certain extent nuclear studies in the investigation of JIA. Radiotracer accumulation in synovitis depends on increased blood flow, enlargement of the vascular pool, and capillary leak. The radionuclide detection of the active soft tissue inflammatory process of arthritis consists of rapid early transit of activity on angiographic images and enhanced concentration of soft tissue phase activity on blood pool images. Multiphase (angiographic, soft tissue, and delayed) bone scintigraphy with 99mTc methylene diphosphonate (Tc-99m MDP) or hydroxymethylene diphosphonate (Tc-99m HDP) have been considered the preferred imaging technique for differentiation of soft tissue and bone abnormalities and may be useful in excluding serious infection or neoplasm in children with nonspecific arthritic symptoms.
Bone scintigraphy may be useful for excluding serious infection or tumor in children with nonspecific arthritic symptoms.
Similarly, a few studies in adults have demonstrated the ability of positron emission tomography (PET) to detect inflammation of the synovium; however, very little information is available in children, and clinical implications of potential findings are not clear at this point.
Bone Densitometry
Osteopenia is a well-recognized radiographic finding in JIA as a consequence of chronic corticosteroid therapy. The technique of dual energy x-ray absorptiometry (DXA) permits regional bone and whole body measurement of bone mineral content and bone mineral density. Using a low-radiation-dose scan beam, the computer-generated images are not of diagnostic use. They are used for gross anatomic detail and allow for the selection of regions of interest that will be analyzed by computer. Normative values in children are becoming available ; however, overall there is a paucity of appropriate reference databases for osteoporosis. In addition, no formal guidelines are currently available at this point to define pediatric osteoporosis. This is in large part related to reservations that clinicians have about the diagnostic significance of reduced bone mineral density measurements for children and adolescents, in contrast to what these changes mean for adults. As a result, many advocate that the current diagnosis of pediatric osteoporosis should be based on multiple rather than single tests of bone health. Alternative methods for assessment of bone densitometry include quantitative computed tomography (QCT) and quantitative ultrasonography (QUS).
Investigational MRI Techniques for Assessment of Pediatric Osteoporosis
Micro-MRI–based virtual bone biopsy: This imaging modality seeks to acquire images at a resolution sufficient to visualize individual bony trabeculae and to obtain quantitative information in the form of structural parameters similar to those of histomorphometry. This method consists of bracelet-style MR receive-only radiofrequency phased array surface coils that detect the raw data, MR scanner software that enhances the SNR, and image processing software that uses special algorithms to transform the data into highly detailed, 3D models of bone microarchitecture. The in-plane image resolution with this technique is approximately 156 μm, which is similar to the dimensions of the bony trabeculae (78 to 200 μm).
Measurement of R 2 * of the trabecular bone marrow: This method is based on the rate for the decay of the free induction signal, which is sensitive to the local magnetic field inhomogeneities induced by the trabeculae in the marrow spaces. Reduced bone density lowers R 2 *, which is also a function of trabecular orientation relative to the magnet’s static field.
Measurement of trabecular bone volume fraction: This technique is based on the attenuation of the spin echo amplitude because of the fractional occupation of the imaging voxel by bone (which does not generate a signal). Its resolution is not sufficient to discriminate the individual elements of the bone.
Sagittal Laser Optical Tomography
Optical methods that rely on transillumination measurements have emerged as potential new tools for detecting joint inflammation in JIA. This investigational technique uses low-level, non-ionizing near-infrared radiation. It constitutes a low-cost joint imaging modality with a potential application in JIA for distinguishing joints that have been affected by synovitis versus those that have not.
Extraarticular Findings
Rarely retroperitoneal fibrosis may be associated with autoimmune disorders or idiopathic arthritis. Cross-sectional imaging with ultrasonography, CT, or MRI may demonstrate the retroperitoneal fibrosis directly and identify any associated vascular and ureteral narrowing.
Anemia caused by poor dietary intake, by chronic gastrointestinal blood loss due to drug treatment, or by the chronic disease process may be a significant problem in JIA. Oligoarticular arthritis is associated with chronic uveitis, which is asymptomatic and may therefore go underdetected.
Chronic uveitis is asymptomatic and is most often found in patients with oligoarticular arthritis. Thus periodic ophthalmologic examination is warranted in patients with oligoarticular disease.
Systemic JIA is associated with amyloidosis, which leads to significant morbidity and mortality. Radiolabeled serum amyloid P component scintigraphy and turnover studies were shown to be useful complementary tools in the diagnosis, screening, and quantitative monitoring of amyloidosis in JIA ; however, in practice, other non–radiation-bearing imaging techniques are more frequently used in JIA. Systemic JIA has also been associated with the “macrophage activation syndrome,” which may be related to intercurrent viral illness, uncontrolled disease activity, and the use of certain drugs such as gold and sulphasalazine. This syndrome is characterized by fever, hematocytopenia, hepatic dysfunction, encephalopathy, and disseminated intravascular coagulation.
The macrophage activation syndrome is characterized by fever, hematocytopenia, hepatic dysfunction, encephalopathy, and intravascular coagulation.
Cross-sectional imaging including Doppler ultrasonography of the hepatic vasculature and head CT and MRI are adjunct tools for assessment of potential complications. Ultrasonography and CT may be used to identify extraarticular complications such as hepatosplenomegaly or serositis ( Figure 24-5 ).

New MRI Techniques
Perfusion-weighted imaging (PWI): Used to assess blood flow and residual tissue perfusion in ischemic areas by estimating the physiologic properties of the synovial microvessels, including blood/plasma volume and transendothelial permeability of the contrast agent. It uses intravenously administered paramagnetic contrast agents and is based on a dynamic process that quantifies the blood supply to a given region of interest during the transit of the contrast material. Potential roles of this technique in the developing skeleton are to recognize maturation patterns of cartilaginous enhancement in order to rule out pathologic processes such as epiphyseal ischemia, inflammation, edema, and revascularization ; to quantify and to monitor synovial inflammation ; and to direct therapeutic scheduling for RA according to enhancement patterns.
Delayed gadolinium-DTPA – enhanced T1-weighted imaging (dGEMRIC): A technique sensitive to quantification of cartilage proteoglycan content. Proteoglycans, collagen, and water play critical roles in the mechanical function of cartilage. Due to negatively charged glycosaminoglycan (GAG) side chains, proteoglycans attract cations and water into the tissue, causing a swelling pressure. These interactions result in a poroelastic, mechanically resilient tissue that enables smooth joint movements and load bearing during locomotion. The dGEMRIC technique utilizes the negative charge of the paramagnetic MR contrast agent, which is assumed to distribute into the cartilage inversely to the fixed charge density of negatively charged GAGs. Thus T1 relaxation time in the presence of the contrast agent is approximately linearly related to the GAG content.
Blood oxygen level dependent (BOLD) MRI: A noninvasive diagnostic technique that assesses the concentration of oxyhemoglobin and deoxyhemoglobin at the capillary level during functional activation by comparing the response of the tissue to vasodilatory (hyperoxia) and nonvasodilatory (normoxia) stimulus. An activated (hyperoxic) state increases the concentration of oxyhemoglobin, thus reducing the concentration of deoxyhemoglobin, which serves as an intrinsic, oxygen-sensitive, paramagnetic marker. This technique may detect temporal changes in the synovial response of the joint to a stimulus.
T2-relaxation time mapping: This technique of evaluation of the superficial cartilage has been shown to be sensitive to the integrity of the collagen network. Spatial variation of T2 correlates with the 3D arrangement of the collagen fibrils as revealed by polarized microscopy. While cartilage degeneration is known to involve progressive disruption of the collagen network, T2 measurements may characterize the structural integrity of the cartilaginous tissue and quantitatively assess the degree of cartilaginous degeneration as previously shown in the pediatric population.
Recommendations for Imaging
Assessment of disease activity is important for monitoring treatment efficacy and predicting outcome. Histopathologic evidence of persistent synovitis and radiologic deterioration has been observed in patients assumed clinically and biochemically to have inactive disease.
Radiography can be used to quantify joint destruction and assess disease treatment with absence of change and lack of progression implying treatment success. In children who received methotrexate, no interval carpal length narrowing was found in responders compared with the progressive worsening seen in nonresponders. Although joint space narrowing and erosion scores did not improve, some patients did show improvement in carpal length.
Intraarticular corticosteroids can be used to temporarily suppress local joint inflammation. Following injection of intraarticular corticosteroids, periarticular calcification can be noted. Other changes related to intraarticular therapy seem uncommon even with repeated joint injections.
Ultrasonography may also be a useful means to noninvasively follow changes in synovitis with therapy. Ultrasonography may play a role in supporting clinical suspicion of disease activity in clinically mild or silent joints and in deciding upon discontinuation of therapy. Increases in synovial thickening and synovial fluid accompany clinical worsening; however, the significance of residual synovial thickening and effusion seen on ultrasonography in asymptomatic patients remains unclear. It may represent active silent disease or inactive fibrous pannus in a quiescent phase. Following intraarticular therapy for JIA in the hips and knees, decrease in synovial effusion, synovial proliferation, and adenopathy has been noted on ultrasonography.
Contrast-enhanced MRI can be used to quantitatively monitor synovial membrane volumes, effusion volumes, and cartilage and bone erosion scores. Synovial membrane volume may reflect the degree of edema, dilated vessels, and cellular infiltration in the synovial membrane and may be a measure of synovial inflammatory activity. Synovial volume, however, may also reflect the cumulated synovial proliferative disease activity and appears to correlate with duration of clinical remission. Several studies have indicated a close relationship between the rate of contrast enhancement and inflammatory activity with the enhancement rate apparently decreasing after intraarticular corticosteroid administration and remaining low during clinical remissions and increasing prior to the return of symptoms, which indicates subclinical increase in synovial inflammatory activity. However, there may be regions of marked heterogeneity in rate of synovial enhancement, so the use of small regions of interest may be a limitation. Cases of clinical relapse show increased enhancement back to pretreatment levels.
Enthesitis-Related Arthritis
This diagnostic subgroup comprises those children with arthritis and enthesitis (inflammation at the site of attachment of ligaments or tendons to bone). Also included are those with either arthritis or enthesitis plus two of the following: (1) sacroiliac (SI) joint tenderness and/or inflammatory spinal pain; (2) presence of HLA-B27; (3) family history of HLA-B27–positive disease; (4) acute anterior uveitis; or (5) onset of arthritis in a boy older than 8 years. A family history of psoriasis would lead to exclusion from this category. Other entities related to the seronegative spondyloarthropathies include the arthritis associated with hyperostosis, acne and/or palmar pustulosis, Whipple’s disease, and Behçet’s disease. These disorders affect the axial and extraaxial joints. Synovitis and enthesitis are recognized as major target areas of inflammation. Enthesitis is commonly present especially at the insertions of the Achilles’ tendon, plantar fascia, and patellar and quadriceps tendons. The juvenile form of enthesitis is more common than the adult form. This group of disorders affects boys more often than girls, begins in late childhood or early adolescence (mean age of onset, 10 to 12 years; range, 3 to 15 years), and typically involves fewer than four joints. A family history is often present (30%) as is the HLA-B27 antigen (90%).
Osteoarticular Imaging Features
Radiographic findings are common amongst all the spondyloarthropathies and are similar to JIA with the exception of sacroiliitis and enthesitis, which are more specific for spondyloarthropathy.
Peripheral Skeleton
Radiography
Radiography typically shows asymmetric involvement of the large joints of the lower limb; in other words, the hip, ankle, knee, and tarsal joints ( Box 24-2 ). The small joints are less frequentlyaffected; however, the interphalangeal joint of the hallux is often involved at presentation. Radiographs are usually normal initially but later may demonstrate soft tissue swelling, effusion, ossification and epiphyseal overgrowth, erosions ( Figure 24-6 ), osteopenia, joint space narrowing, or erosion and rarely fusion. Erosions are typically associated with irregular bone apposition at joint margins, referred to as “whiskering” (see Figure 24-6 ). Rapid joint destruction can be noted. With hip involvement, these proliferative changes are noted at the junction of the femoral head and neck. Dactylitis may be seen with soft tissue swelling and periosteal reaction along the shaft of metacarpals, metatarsals, or phalanges. In juvenile ankylosing spondylitis, extraaxial arthritis usually involves one or more large joints of the lower extremities (e.g., hips, knees, ankles) along with the sacroiliitis.