Key Facts
- •
Soft tissue calcifications appear on radiographs as punctuate, circular, linear, or plaque-like radio-dense areas. Often these calcifications, by their appearance and location, can provide clues to an associated medical disorder.
- •
Calcific tendinitis (hydroxyapatite deposition disease) is most commonly located in the supraspinatus tendon of the shoulder. It may be asymptomatic or may result in severe pain, erythema, swelling, painful range of motion, and fever.
- •
Tumoral calcinosis is a condition usually affecting dark-skinned people. It is characterized by prominent periarticular calcified masses around large joints, especially the hips. Large amorphous masses containing fluid-calcium levels are identified, especially on cross-sectional imaging.
- •
Myositis ossificans is a localized form of post-traumatic heterotopic calcification and ossification that occurs in a traumatized muscle, particularly in the anterior thigh. The mass characteristically matures from the periphery to the center; a rim of calcification is seen by 6 to 8 weeks and is separate from the underlying bone.
- •
Fibrodysplasia ossificans progressiva is a very rare condition presenting in childhood, characterized by painful soft tissue masses that progress to sheets and struts of ossification that bridge joints. These ossific bands eventually result in severely limited mobility and diminished chest wall excursion, leading to early death.
The radiographic detection of calcification and ossification in the soft tissues often provides an important clue to the correct clinical diagnosis. Soft tissue calcifications appear as irregular punctuate, circular, linear, or plaque-like radio-dense areas that do not possess a trabecular or cortical structure. The location of soft tissue calcifications is of importance in narrowing the differential diagnostic considerations.
Soft tissue calcifications that occur in tendons or bursae suggest hydroxyapatite deposition disease or calcium pyrophosphate deposition disease. Calcification in lymph nodes may indicate granulomatous infection such as tuberculosis. Arterial calcification is seen in renal osteodystrophy, diabetes mellitus, and hypervitaminosis D. Calcified nerves are a hallmark of leprosy. Chondrocalcinosis has a long list of causes including hemochromatosis, primary hyperparathyroidism, and Wilson’s disease, among others. Multiple calcified intervertebral disks suggest alkaptonuria. Soft tissue calcification of the fingertips is characteristic of collagen vascular disorders, especially the scleroderma variant known as CREST (calcinosis, Raynaud’s, esophageal dysmotility, sclerodactyly, and telangiectasias). Calcification of the pinna of the ear may raise suspicion for endocrine disorders or previous thermal trauma. Multiple calcifications in the muscles may suggest parasite or worm infestation ( Figure 39-1 ).

Soft tissue ossification may occur in neurologic diseases, physical and thermal trauma, venous insufficiency, neoplasms such as soft tissue osteosarcoma, myositis ossificans (MO) progressiva, melorrheostosis, and in surgical scars.
Generally, the work-up of a patient with soft tissue calcifications includes measurements of serum calcium, serum phosphate, PTH levels, calcitonin measurement, 24-hour urinary calcium, and phosphorus. The evaluation of cartilage calcification (chondrocalcinosis) may include measurement of serum iron, total iron binding capacity, ferritin, parathyroid hormone, and thyroid function studies.
HYDROXYAPATITE DEPOSITION DISEASE (CALCIFIC TENDINITIS, CALCIFIC PERIARTHRITIS)
Hydroxyapatite crystal deposition disease (HADD) is a crystal-induced arthropathy in which there is deposition of hydroxyapatite crystals in the paraarticular soft tissues resulting in tendinitis and bursitis. It may occur as a primary idiopathic phenomenon or be secondary to other disease states. Thus, HADD may also be seen in patients with connective tissue disorders such as scleroderma, secondary hyperparathyroidism, or osteoarthritis. More than 30% of patients with insulin-dependent diabetes mellitus may develop asymptomatic tendon calcification.
HADD is characterized by the presence of basic calcium phosphate crystals—predominantly hydroxyapatite in the periarticular soft tissue, especially the tendons ( Figure 39-2 ). Since the actual deposition may occur in the tendon, bursa, or joint capsule, the term periarthritis, rather than peritendinitis is preferred. Macroscopically, HADD appears as calcified amorphous material with a “milky” or “cheesy” consistency in the paraarticular fibrous connective tissue. HA crystals vary in size from 100 to 200 nm and are too small to be seen with ordinary polarized light microscopy.


A continuum of abnormalities ranging from monarticular periarthritis to polyarticular disease to joint destruction may occur.
The peak incidence of calcific tendinitis occurs in the fourth to sixth decades of life. It is responsible for almost 50% of all shoulder pain. Calcification about the shoulder is seen in approximately 3% of adults, although most cases discovered on radiographs are asymptomatic.
Calcific tendinitis most commonly affects the tendons about the shoulder. In addition, the tendons of the gluteus maximus, rectus femoris, vastus lateralis, quadriceps, pectoralis major, deltoid, and adductor magnus, as well as tendons of the wrist, hand, neck, and ankle may be affected.
Although most frequent in the shoulder, calcific tendinitis may affect many different tendons, including the gluteus maximus insertion and the longus colli in the neck.
In the shoulder, the most common tendon involved is the supraspinatus, and a site 1.5 cm proximal to its insertion on the greater tuberosity is the most common area of that tendon to be affected. This portion of the tendon has been shown to be subject to hypoxic and mechanical stress and is termed the critical zone. These stresses may incite events leading to fibrocartilage transformation followed by calcification ( Figure 39-3 ). Resorption of the calcification (the resorptive phase) produces extreme pain that may become incapacitating. This acute pain, which can mimic septic arthritis, may be due to increased intratendinous pressure. Acutely, erythema, swelling, painful range of motion, and fever may be noted. Finally, in the postcalcific phase, the calcific deposit has been phagocytized, and the void is rapidly replaced by granulation tissue. The chronic pain of the postcalcific stage is thought to last until the newly synthesized collagen fibers align themselves along the axis of the tendon ( Table 39-1 ).

| Stage | Histologic Findings | Clinical Findings | Radiographic Findings |
|---|---|---|---|
| Precalcific | Fibrocartilage transformation of the “critical zone” | Symptomatic or asymptomatic | None |
| Calcific: formative | Fibrocartilage replaced by calcific deposit | Homogeneous well-defined calcification | |
| Calcific: resorptive | Macrophages and giant cells resorb the calcification. | Acute symptoms | Amorphous, less dense, ill-defined calcification. Soft tissue swelling |
| Postcalcific | Calcification has been resorbed and the defect fills with collagen | Chronic pain until new collagen is aligned with long axis of tendon | None |
Hydroxyapatite deposits are seen on radiographs as homogeneous, amorphous densities without trabeculation. They are variable in size and their margins may be smooth and well-defined or ill-defined ( Figure 39-4 ).

Well-defined dense calcifications are usually chronic and may be incidental findings, whereas poorly defined, less dense calcifications correlate with acute symptoms.
Calcific tendinitis of the supraspinatus tendon is best visualized on external rotation views of the affected shoulder. As the shoulder is rotated internally, the calcifications move medially, so that the calcific deposits may project over the humeral head making them more difficult to identify.
In patients with radiographically demonstrated supraspinatus calcification, it is estimated that fewer than 10% will ever develop symptoms of acute calcific tendinitis.
Subscapularis calcific tendinitis may be more difficult to see on routine radiographs of the shoulder because the calcification can be obscured by overlying bone ( Figure 39-5 ). An axillary view is helpful. Calcific deposits due to HADD may enlarge, decrease, disperse, or completely resolve with time.


The diagnosis of calcific tendinitis is usually made clinically and can be confirmed on appropriate radiographs.
Patients with acute calcific tendinitis present with severe pain involving the affected joint. There may be intense soft tissue swelling and warmth mimicking infection.
Occasionally computed tomography (CT) is used, especially when the calcium is atypical or there is concern for cortical involvement. The use of magnetic resonance imaging (MRI) is limited and may actually be confusing as the presence of soft tissue and osseous edema may raise the suspicion of infection or neoplasm. On MRIs, the calcification appears as areas of decreased signal intensity on T1-weighted images, whereas T2-weighted images may show increased signal corresponding to edema surrounding the low signal calcific deposit ( Figure 39-6 ).


Acute calcific periarthritis of the hand mainly affects women (5:1) in the premenopausal age group. In the wrist, the distal flexor carpi ulnaris tendon is the most common location of calcific tendinitis. This may be a cause of volar wrist pain and marked associated soft tissue swelling. The calcification is best seen on a carpal tunnel view, semi-supinated oblique view of the wrist, or can be readily identified on axial noncontrast CT scans ( Figure 39-7 ).


In the neck, calcification may affect the longus colli muscle, whose primary function is neck flexion. Calcification of the longus colli is best seen on well-positioned lateral cervical spine radiographs, where the calcification is seen just anterior to C1 or occasionally C2. CT confirms calcification at the C1-C2 level and the accompanying soft tissue swelling. MRI may demonstrate prevertebral increased signal on T2-weighted images due to muscle swelling.
Calcific tendinitis of the longus colli muscle can produce odynophagia, dysphagia, and fever in older patients. The correct diagnosis can often be made on radiographs.
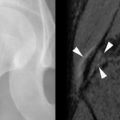
Calcific tendinitis of the distal insertion of the gluteus maximus may present with a painful upper posterior thigh. Most of the fibers of the gluteus maximus insert on the iliotibial tract of the tensor fascia lata, dorsal and distal to the greater trochanter, but some insert on the gluteal tubercle of the posterior lateral upper femoral shaft (part of the linea aspera). Calcification that occurs here can be difficult to detect. The calcium will overlie the upper femoral shaft on an anteroposterior radiograph, and therefore may be best seen on a frog lateral radiograph or even more easily on axial CT images ( Figure 39-8 ). The pain associated with calcium in this location may mimic radicular pain. In addition, posterior femoral cortical erosion adjacent to the calcification has been noted in some cases ( Figure 39-9 ).



Cortical bone erosion has been observed in calcific tendinitis, although bone destruction is not generally considered to be a feature of the disorder. Calcific tendinitis with bone erosion is most commonly observed in the femur (40%) and the humeral head (40%). Hayes et al. presented five cases; two involved the pectoralis major insertion, two involved the gluteus maximus insertion, and one the adductor magnus insertion. Bone resorption may reflect increased local vascularity and active inflammation at the tendon insertion. Alternatively, it may be caused by local pressure from the calcium deposit ( Figure 39-10 ).



Cortical erosion is the most common manifestation of osseous involvement (78% of cases), but bone marrow involvement has been demonstrated in 18 of 50 cases (36%) ; (61%) involving the greater or lesser tuberosities of the humeral head. When calcific tendinitis presents with osseous destruction, bone marrow signal changes on MRI, and soft tissue calcification, there may be confusion with neoplasm both radiographically and pathologically.
Calcific tendinitis may be associated with adjacent cortical erosion and marrow changes causing confusion with neoplasm. A comet-tail appearance of the calcification, present in calcific tendinitis, may suggest the correct diagnosis.
The main differential diagnosis for the acute symptoms of calcific tendinitis at presentation is infection or crystal induced arthritis, such as gout, especially if the area of involvement is near a joint. Rarely, acute attacks can occur at multiple sites. The differential diagnosis of radiographically demonstrated periarticular calcification due to HADD includes calcium pyrophosphate deposition disease (CPPD), metastatic calcification, connective tissue diseases, accessory ossicles (a normal variant), and soft tissue tumors containing calcium.
Milwaukee Shoulder
Milwaukee shoulder is a destructive arthropathy of the shoulder associated with chronic tears of the rotator cuff and joint effusions containing hydroxyapatite. Milwaukee shoulder most commonly affects elderly women. In addition to HA crystals, calcium pyrophosphate crystals are also frequently identified in the joint fluid. Radiographically, one can identify glenohumeral degenerative changes, soft tissue calcification, loose bodies, which will present as filling defects during arthrography, joint instability, rotator cuff tear, and soft tissue swelling. Many patients also have a severe destructive arthropathy of the knees.
Calcinosis Universalis
Idiopathic calcinosis universalis is of unknown etiology and affects infants and children. Calcium phosphate and calcium carbonate are deposited about normal fat cells. There is a foreign body reaction. Serum calcium and phosphorus levels are normal. Discrete conglomerates of calcium are arranged in longitudinal bands. The major differential diagnosis includes dermatomyositis and hyperparathyroidism.
Tumoral Calcinosis
The term tumoral calcinosis has been used liberally to describe any massive collection of periarticular calcification, although the term actually refers to a hereditary condition associated with massive periarticular calcification ( Figure 39-11 ). The inheritance of the latter condition is autosomal dominant with variable expressivity ; it may be related to an inborn error of phosphorus metabolism. Patients have slightly raised levels of urinary hydroxyproline, reduced fractional phosphate excretion, increased 1,25-dihydroxy–vitamin D formation, and a normal dynamic response to parathormone and hyperphosphatemia. Some patients may have an elevated level of serum phosphorus. However, serum calcium, parathyroid hormone, renal function, and alkaline phosphatase are normal.