Key Facts
- •
DiGeorge’s syndrome, type I autoimmune polyglandular syndrome, X-linked or autosomally inherited hypoparathyroidism, and PTH gene mutations are the most frequent causes of congenital hypoparathyroidism.
- •
Pseudohypoparathyroidism (PHP) is an inherited disorder resulting from mutations in the end-organ PTH receptors, leading to PTH resistance.
- •
Albright hereditary osteodystrophy is a somatic phenotype of PHP characterized by developmental delay, mental retardation, obesity, round face, hypoplastic dentition, short stature, subcutaneous calcifications, brachymetacarpals, and brachymetatarsals (shortening of affected bones).
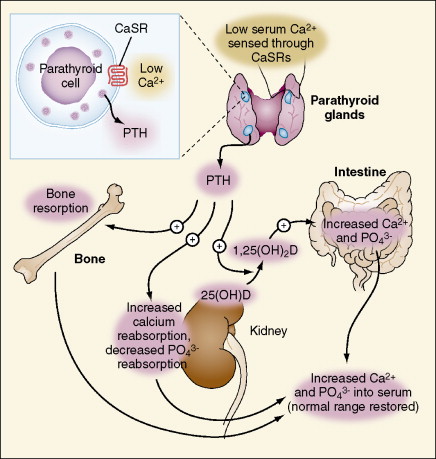
Hypoparathyroidism, the impaired secretion of parathyroid hormone (PTH) from the parathyroid glands, is the most common cause of hypocalcemia. The inadequate parathormone (PTH) secretion causes failure to mobilize calcium from bone, reabsorb calcium from the distal nephron, or stimulate renal I α-hydroxylase activity. The decreased 1,25[OH] 2 vitamin D leads to inefficient absorption of calcium from the gut ( Figure 34-1 ). Hypoparathyroidism occurs as a result of congenital (inherited) or acquired (secondary) disorders. DiGeorge’s syndrome, type I autoimmune polyglandular syndrome, X-linked or autosomally inherited hypoparathyroidism, and PTH gene mutations are the most frequent causes of congenital hypoparathyroidism. In DiGeorge’s syndrome, a defect in the development of the third and fourth pharyngeal pouches leads to agenesis of parathyroid gland. Type I polyglandular syndrome is characterized by hypoparathyroidism, adrenal failure, and mucocutaneous candidiasis and develops from circulating antibodies against parathyroid, thyroid, and adrenal glands. Parathyroid glands are absent in X-linked (or autosomally) inherited hypoparathyroidism. PTH is deficient in PTH gene mutations.
Damage to the parathyroid glands can lead to secondary hypoparathyroidism. Postsurgical hypoparathyroidism is the most frequent cause of prolonged hypocalcemia and is seen after thyroid and other head and neck surgeries. Infiltration of the parathyroid glands may develop subsequent to several disorders including hemochromatosis, thalassemia major (iron overload due to numerous blood transfusions), Wilson’s disease, and rarely, metastases. Radiation and radioactive iodine thyroid ablation are other secondary causes.
Pseudohypoparathyroidism (PHP) is an inherited disorder resulting from mutations in the end-organ PTH receptors leading to PTH resistance. Similar to hypoparathyroidism, the ultimate outcome would be the absence of PTH action on end organs. In contrast to hypoparathyroidism, in pseudohypoparathyroidism the serum level of PTH is high due to of the lack of negative feedback on the parathyroid glands. Besides the radiographic manifestations of hypoparathyroidism, specific findings are also noticed in pseudohypoparathyroidism as described below.
IMAGING FEATURES OF HYPOPARATHYROIDISM
Radiographs
Radiography is the most widely used modality to evaluate the skeletal and soft tissue changes of hypoparathyroidism. Localized or diffuse osteosclerosis (increased density of bone tissue) is the most common skeletal finding in hypoparathyroidism. Thickening of the facial bones and cranial vault with a widened diploe are seen. Sutural diastasis may be present as a consequence of increased intracranial pressure. Intracranial calcifications (basal ganglia, falx, and rarely the cerebellum and choroids plexus) occur due to the metabolic abnormality. Calcification of ligaments (e.g., anterior longitudinal ligament and posterior paraspinal ligaments in the spine) and calcifications of muscle insertions (enthesopathy) are features of hypoparathyroidism. Hypoplastic dentition, delayed or failed eruption of the teeth, and a thickened lamina dura (the thin hard layer of bone that lines the socket of a tooth appearing as a white line on radiography) may be observed. Asymptomatic or painful subcutaneous calcifications, particularly around shoulders and hips, can develop. Band-like radiodensities are noticed in the metaphyses of long bones, and sclerosis of the iliac crests and the margins of the vertebral bodies may be present. Premature closure of the physes is another radiographic finding in the developing skeleton.
Rarely, the radiologic changes of ankylosing spondylitis and hypoparathyroidism may resemble each other. However, in the latter, there is no tenderness in the spine and pelvis, and although spinal osteophytes and calcification of spinal ligaments may be seen, the sacroiliac joints are spared.
Ultrasonography
Renal ultrasonography may reveal nephrocalcinosis in the patients receiving treatment due to the resultant calciuria. Therefore, a baseline renal ultrasonogram is recommended prior to the initiation of treatment.
Nephrocalcinosis may develop with treatment of hypoparathyroidism as a consequence of calciuria. A baseline renal ultrasound examination is recommended.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree