Degenerative (most common)
Inflammatory (5–10 % of all)
Mycotic
Syndromes: Marfan’s syndrome, Ehlers-Danlos syndrome
Vasculitis: Takayasu’s disease, Behcet’s disease
Traumatic
Other less frequent etiologies of AAA include mycotic aneurysm, which constitutes 1–3 % of aortic aneurysms. However, mycotic aneurysm is known to more commonly involve aorta than any other artery. Staphylococcus and Streptococcus species are the most common pathogens of mycotic aneurysm. The cases of mycotic aneurysm due to Salmonella species are more common in East Asia and demonstrate an early tendency to rupture.
The most significant complication of AAA is aortic rupture. The mortality rate for ruptured AAA is 50 %; thus, an accurate diagnosis is essential for prompt surgical intervention. The risk of rupture is proportional to the maximum cross-sectional diameter, with 1 %/year risk for aneurysms measuring 5–5.9 cm. The risk of rupture increases up to 20 %/year for an aneurysm measuring greater than 7 cm in diameter. Although AAAs are less common in females (M:F = 4:1), they are more likely to rupture when compared to males.
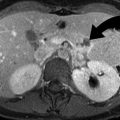
Ultrasound is the most commonly used imaging modality to screen for AAA and has been shown to reduce mortality. The imaging criteria to diagnose AAA include aortic caliber of more than 3 cm and an aortic caliber of more than 1.5 times the expected diameter of the abdominal aorta (Fig. 1.1). The aortic caliber is measured perpendicular to the long axis of the aorta, from outer wall to outer wall. Although ultrasound is highly sensitive in making the diagnosis of abdominal aortic aneurysm, it is not as reliable as CT in diagnosing aortic rupture. However, the demonstration of normal caliber of abdominal aorta by ultrasound makes aortic rupture an unlikely possibility.
Fig. 1.1
Saccular abdominal aortic aneurysm. (a and b) US demonstrate a saccular infrarenal aortic aneurysm (curved arrow) with yin-yang sign on color Doppler imaging. (c) Sagittal reformation demonstrates the saccular infrarenal abdominal aortic aneurysm (curved arrow)
Most aortic aneurysms rupture involves the middle third of the aneurysm, through the posterolateral wall and into the retroperitoneum (Fig. 1.2a). However, intraperitoneal rupture and rupture into the bowel (usually the duodenum) and very rarely into the IVC may occur (Fig. 1.2b, c).
Fig. 1.2
Abdominal aortic aneurysm rupture, aorto-enteric and aortocaval fistula. (a) Contrast-enhanced CT scan study of the lower abdomen demonstrates active extravasation of contrast (arrow) from infrarenal abdominal aortic aneurysm. There is retroperitoneal hemorrhage (arrowheads) identified around the aortic aneurysm. (b) Aorto-enteric fistula. Contrast-enhanced CT scan study demonstrates communication (arrowhead) of the third portion of the duodenum (arrow) with the infrarenal abdominal aortic aneurysm sac. The patient had recently undergone endovascular stent placement. (c) Aortocaval fistula. Doppler US shows the combination of arterial and venous spectral waveform in the inferior vena cava lumen, in a patient with aortocaval fistula
Risk Factors for Aortic Rupture
Progressive aneurysmal dilatation of the aorta with increased wall tension is directly related to the risk of rupture. The decreased proportion of thrombus to lumen ratio is also thought to play a part, as a larger thrombus better protects against rupture by providing protection against the high aortic pressures [1]. In addition, the amount of thrombus calcification, which is thought to be related to the amount of thrombus present, is also an indirect measure [2].
Imaging
The imaging modality of choice is a contrast-enhanced multidetector CT (MDCT). The CT can demonstrate an AAA with surrounding retroperitoneal hemorrhage into psoas compartment, pararenal space, and perirenal space. A contrast-enhanced CT provides additional information about the aortic size, presence or absence of active extravasation, and anatomic relationships (Table 1.2). A hyperdense crescent sign and draped aorta sign are indicators of contained aortic leak or impending rupture. Focal discontinuity of intimal calcification is also a secondary sign of aortic rupture.
Table 1.2
CT findings of aortic rupture
1. Active extravasation of contrast |
2. Retroperitoneal hematoma around the aortic aneurysm |
3. Periaortic stranding |
4. Draped aorta sign |
5. Hyperdense crescent sign |
6. Tangential calcium sign |
7. Discontinuity of intimal calcification |
Hyperdense Crescent Sign
Hyperdense crescent sign is seen as a well-defined peripheral, high-density, crescent configuration within a thrombus where there is internal dissection of hemorrhage into the thrombus and ultimately reaching the aortic wall. It is a sign of acute or impending rupture (Fig. 1.3a) [1].
Fig. 1.3




CT features of abdominal aortic aneurysm rupture. (a) Hyperdense crescent sign. Noncontrast CT demonstrates large retroperitoneal hematoma (arrowhead) from the ruptured aortic aneurysm. A hyperdense crescent (curved arrow) is present in the anterior wall of the infrarenal abdominal aortic aneurysm. (b) Draped aorta sign. Contrast-enhanced CT demonstrates draping of the posterior wall of the aorta (straight arrows) on the anterior aspect of the lumbar spine. There is large retroperitoneal hematoma (curved arrow) identified in the psoas compartment and left posterior pararenal space. (c) Schematic representation of the draped aorta sign (a) and hyperdense crescent sign (b). Draped aorta sign is characterized by draping of deficient aortic wall on the anterior aspect of the vertebral body. Hyperdense crescent sign is characterized by the presence of a high-density sickle-shaped blood clot in the aortic wall. (d) Tangential calcium sign in a patient with contained aortic leak. Noncontrast CT demonstrates intimal calcifications (arrowheads) displaced from their expected location and pointing away from the aortic circumference. (e) Rupture of mycotic aneurysm. Noncontrast CT demonstrates air in the wall of the aortic aneurysm, secondary to clostridial infection. Breech in the aortic wall is indicated by the presence of air (arrowheads) outside the aortic adventitia
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree