Fig. 8.1
Testicular anatomy. (a) Schematic diagram demonstrates normal testicular anatomy. (b) Hydrocele: schematic diagram demonstrates fluid between tunica albuginea and tunica vaginalis
Fig. 8.2
Hydrocele and pyocele. (a) Hydrocele: ultrasound demonstrates anechoic fluid collection (arrowheads) between the parietal and visceral layers of the tunica albuginea, surrounding the testicle. (b) Hydrocele: contrast-enhanced axial CT imaging of the pelvis demonstrates the fluid-density hydrocele (arrowhead) surrounded by the parietal layer of the tunica albuginea. (c) Pyocele: ultrasound imaging demonstrates complex fluid collection (arrowheads) surrounding the testicle with multiple internal septations
Ultrasound is the imaging technique of choice in determining the type of fluid collections. While hydroceles are usually anechoic collections, hematoceles and pyoceles show complex fluid with internal echoes and variable septations and loculations.
Varicocele
Varicocele is characterized by increase in the diameter of the pampiniform plexus veins (normal range 0.5–1.5 mm), resulting in a collection of tortuous elongated veins posterior to the testicle [2].
When idiopathic, it is caused by incompetent valves in the internal spermatic vein, resulting in blood flow reversal (spermatic cord to pampiniform plexus). It is usually left-sided due to venous drainage into the renal vein rather than inferior vena cava (right vein directly drain into the inferior vena cava) [2, 3]. When acquired, it is due to increased pressure on the spermatic venous system (from hydronephrosis, hepatomegaly, and abdominal tumors). In these patients varicocele is bilateral in up to 70 % of patients and more prominent in the upright position and during valsalva maneuver [2].
Color Doppler ultrasound plays an important role in the evaluation of scrotal venous morphology and demonstrates serpentine vessels larger than 2 mm in diameter, next to the epididymis head (Fig. 8.3) [2, 4]. The blood flow is in reversed direction and typically increases during valsalva maneuver and in upright position.
Fig. 8.3
Varicocele. (a, b) Ultrasound demonstrates extratesticular tortuous tubular structures on grayscale imaging and color Doppler imaging
Although traditionally it is surgically treated, it can also be managed with coil embolization by interventional radiologist [5].
Epididymitis and Epididymo-orchitis
Infections of testicles and epididymitis are most common in young adults and are the result of retrograde passage of organisms (N. gonorrhoeae, C. trachomatis, or E. coli) from the urethra, prostate, or seminal vesicles [6, 7]. Epididymitis is the most common cause of inflammatory scrotal disease. Epididymitis and epididymo-orchitis are most commonly secondary to retrograde spread of infection from urinary tract.
The main purpose of imaging in patients with presumed inflammatory disease is to distinguish inflammation from testicular torsion or other surgically treatable causes of scrotal pain, such as abscess or testicular tumor. The ultrasound finding of inflammation includes demonstration of hyperemia, which is well displayed as low-resistance hypervascularity (Fig. 8.4). The normal epididymis demonstrates no detectable flow (even at the lowest possible flow settings), so the detection of any epididymal vascularity is abnormal and indicates hyperemia [4]. Epididymis and testis are usually enlarged and edematous. The sonographic findings of epididymitis include enlarged, hypoechoic, or hyperechoic epididymis and hydrocele. In complicated cases abscess may be visualized with hypervascularity in its margins. On sonography, orchitis is seen as testicular enlargement, heterogeneous echogenicity, and hypervascularity.
Fig. 8.4
Acute orchitis and epididymitis. (a, b) Ultrasound of the testicle demonstrates markedly increased color Doppler flow within the testicular parenchyma (arrow). The testicular echogenicity is mildly heterogeneous. (c, d) Ultrasound of the scrotum demonstrates enlarged epididymis (arrow) with increased color Doppler flow and complex hydrocele (arrowheads)
Other imaging techniques are usually not necessary. MR imaging may show increased, decreased, or normal signal in epididymis and testis with associated hypervascularity and hydrocele [8]. Abscess may be present and seen as complex scrotal fluid collection.
Fournier Gangrene
It is a rapidly progressing polymicrobial necrotizing fasciitis, seen most commonly in 50–60-year-old men. It involves the perineal, perianal, or genital regions and requires immediate surgical debridement as well as aggressive antibiotic treatment.
It is an infection, caused by multiple bacteria (average of more than three organisms), most commonly Escherichia coli, Bacteroides, and streptococcal species [9, 10]. Usually the infection spreads from abscess (perianal, perirectal, and ischiorectal), anal fissures or colonic perforations, urinary tract infections, and epididymitis. The predisposing factors are diabetes mellitus, alcohol abuse, urinary bladder instrumentation, trauma, surgical procedure, tumors, steroid therapy, chemotherapy, radiation therapy, prolonged hospitalization, and HIV infection [9].
On ultrasound, the findings include thickening of the scrotal skin, normal testicles, and hyperechoic soft tissue gas with reverberation artifacts. CT allows the evaluation of soft tissue inflammation, collections, and gas as well as complications, such as subcutaneous emphysema, abscess formation, and retroperitoneal extension (Fig. 8.5). It is also helpful in differentiating Fournier gangrene from inguinal hernia, soft tissue edema, and cellulitis.
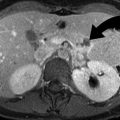
Fig. 8.5
Fournier gangrene. (a–c) Axial CT imaging of the lower pelvis demonstrates soft tissue air infiltrating in the perineum, penile shaft, and scrotal sac, secondary to anaerobic infection. (d, e) Ultrasound and CT demonstrate scrotal abscess containing foci of air (arrow). (f) Coronal CT reformation demonstrates omental fat passing through patulous left inguinal canal (arrowhead), into left scrotal hernia (arrow)
The complications include abscess extension to thigh or abdomen, coagulopathy, diabetic ketoacidosis, sepsis, and multiple organ failure. The treatment includes hemodynamic stabilization, intravenous antibiotics, and surgical debridement of the necrotic tissues. Hyperbaric oxygen has also been used as adjuvant treatment, in patients who do not respond well to surgery.
Testicular Torsion
Spermatic cord torsion is a surgical emergency which affects 1 in 125 males in the USA and requires urgent surgery. The torsion results in vascular compromise, first of the veins and then arteries.
Intravaginal torsion is the most common type and is associated with abnormal suspension of the testis by tunica vaginalis, resulting in bell-clapper deformity. This abnormality has a 2 % prevalence (40–80 % bilateral) and allows the testicle to rotate freely within the hemiscrotum.
Extravaginal torsion is most frequent in newborn, where the testicle is poorly or not at all attached to the scrotal wall, permitting rotational mobility of the testicle. The resulting spermatic cord torsion is at the external inguinal ring level.
Ultrasound is the first-line imaging technique which shows low or absent vascular flow into the symptomatic cord and organs. Other findings include enlargement of the testis as well as epididymis in the first hours of onset. Although the testicular echogenicity is initially normal, with time the testis becomes heterogeneous and hypoechoic, indicating possible nonviability (Fig. 8.6). Hydrocele is frequently present on the affected side. Infarction and hemorrhage develop 24 h after torsion onset and give the testicle a heterogeneous appearance. The diagnosis may be difficult in cases with intermittent torsion where the blood flow may be normal or there may be postischemic hyperemia.
Fig. 8.6




Testicular torsion. (a, b) Grayscale ultrasound imaging demonstrates heterogeneously hypoechoic left testicle in relation to the normal echogenicity of the right testicle (b). (c, d) Power Doppler and color Doppler imaging of the testicle demonstrate complete absence of flow in the testicle parenchyma. There is complex hydrocele identified caudal to the testicle (d)
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree