Fig. 6.1
Drawing illustrates the mechanism of injury for a lateral ankle sprain caused by inversion and internal rotation of the hindfoot coupled with external rotation of the lower leg
6.2.1.1 Imaging and Diagnosis
Diagnosis is usually made through history, physical exam and radiography (Fig. 6.2). The primary role of radiographs is to exclude fracture with the Ottawa Rules remaining valid (Bachmann et al. 2003). However, if there is persistent or worsening pain, swelling, or limited ability to return to play then MRI is indicated. MRI has high concordance with surgical findings for lateral ligament tears and can help identify injured ligaments when stress radiographs are normal (Cardone et al. 1993) (Figs. 6.3 and 6.4). In addition to the high sensitivity and accuracy in evaluating the ligaments, MRI allows detection of other injuries including osteochondral lesions and syndesmotic injury (Kaminski et al. 2013). One study (Khor and Tan 2013) found that a majority of lateral ankle sprains are not isolated injuries but rather associated with other pathologies (bone contusions being most common). This additional information has the potential to alter management and increase time away from play.


Fig. 6.2
Anteroposterior radiograph of the ankle shows soft tissue swelling over the lateral malleolus (arrow). Evaluation for associated injuries including fracture and syndesmotic widening is a primary reason for obtaining the radiographs
Fig. 6.3
A 29-year-old football player with ankle injury. Axial proton density- (a) and fat-suppressed T2-weighted (b) MRI of the ankle demonstrate grade 3 sprain (complete tear) of the ATFL from the talar attachment after inversion injury (arrow). ATFL is the weakest lateral ankle ligament and runs from the talar neck to the anterolateral fibular tip
Fig. 6.4
A 29-year-old football player with ankle injury. Axial (a) and coronal (b) fat-suppressed T2-weighted MRI of the ankle demonstrate grade 3 sprain of the CFL at the fibular attachment (white and black arrows). The CFL is the second most frequently injured lateral ankle ligament. CFL runs deep to the peroneal tendons (arrowheads) attaching the calcaneus (trochlear eminence) to the lateral malleolar tip. A combination of axial and coronal sequences is usually needed to fully evaluate the CFL
6.2.1.2 Grading
Ankle sprain severity is based on clinical exam finding of degree of instability and on imaging as the degree of ligament tearing. Grade 1 sprain is microtearing of the ligament with no evidence of instability. Grade 2 sprain is partial tearing of the ligament with some evidence of instability. Grade 3 sprain is complete rupture of the ligament with definite evidence of instability when physically examined (Scherl and Templeton 2003).
6.2.1.3 Treatment
The treatment for lateral ankle ligament injury is RICE (rest, ice, compression, elevation) and external support followed by rehabilitation (Beynnon et al. 2006; Hubbard and Denegar 2004). A patient’s pain and swelling may subside in weeks; however, treatment should continue to help prevent chronic instability. Rehabilitation programs focus on neuromuscular control, proprioception, and balance training to reduce the risk of recurrent injury (Holme et al. 1999; Verhagen et al. 2000; Wester et al. 1996). One study found the mean time lost from participation in the NFL was 6.5 days with nonoperative conservative management algorithms (Osbahr et al. 2013). Return to play criteria include at least 80 % functional recovery of the injured extremity compared to the non-injured leg, the player’s perception of functionality, and prophylactic support in practice and games to decrease the likelihood of recurrent sprain (Kaminski et al. 2013).
6.2.2 Syndesmotic Ankle Sprain
Syndesmotic ankle sprain, also known as high ankle sprain, is less common than lateral ankle sprain. In the athletic population, football players have been shown to have a higher incidence of syndesmotic injuries (Nussbaum et al. 2001). The tibiofibular syndesmosis refers to the anterior inferior tibiofibular, interosseous, inferior transverse tibiofibular, and posterior inferior tibiofibular ligaments, in decreasing order of injury prevalence (Sikka et al. 2012). The major role of the syndesmosis is to prevent the fibula from displacing laterally and to maintain the hinge and glide motion at the tibiotalar articulation. The deep portion of the deltoid ligament contributes to syndesmotic stability by resisting axial, translational, and rotational forces (Jones and Amendola 2007). Unlike lateral ankle ligament injury where the more common mechanism of injury is torsion, in the NFL, syndesmotic injuries are more often caused by direct impact (Osbahr et al. 2013). External rotation is thought to be the cause of a majority of syndesmotic injuries resulting in separation of the fibula from the tibia (Lin et al. 2006; Thormeyer et al. 2012) (Fig. 6.5). In football this can occur by a tackle to the outside of the knee with the body internally rotated and the foot planted in relative external rotation or a collision to the lateral leg with the foot planted causing internal rotation of the leg relative to the foot (Boytim et al. 1991).
Fig. 6.5
Drawing illustrates mechanism of injury for syndesmotic injury thought to be the caused by external rotation resulting in separation of the fibula from the tibia (Lin et al. 2006). In football this can occur by a tackle to the outside of the knee with the body internally rotated and the foot planted in relative external rotation or a collision to the lateral leg with the foot planted causing internal rotation of the leg relative to the foot
6.2.2.1 Imaging and Diagnosis
Diagnosis of a high ankle sprain requires an accurate history, physical image, and imaging studies. The history provides information on the mechanism of current injury and prior ankle instability issues. The location of injury, tenderness, and clinical examination assist in evaluating for possible syndesmotic injury. Four view radiographs are the initial radiologic workup (AP, lateral, mortise views of the ankle, and orthogonal view of entire tibia-fibula). Weight-bearing films are preferred if the patient can tolerate the exam; otherwise bilateral non-weight-bearing films can be obtained (Smith and Bach 2004). The medial clear space, tibiofibular overlap, and tibiofibular clear space are the three critical areas to evaluate (Zalavras and Thordarson 2007) (Fig. 6.6). The medial clear space is the distance between the medial talus and the lateral aspect of the medial malleolus at the level of the talar dome. In neutral positioning, this space should be less than or equal to the distance between the talar dome and tibial plafond. Associated deltoid ligament injury is suspected when the medial clear space is widened (Ebraheim et al. 2006). On the AP view, tibiofibular overlap should be at least 6 mm and on the mortise view greater than 1 mm, measured 1 cm above the tibial plafond (Zalavras and Thordarson 2007). Tibiofibular clear space is measured 1 cm proximal to the tibial plafond. The distance between the medial border of the fibula and the lateral aspect of the tibia should be less than 6 mm on both the mortise and AP views. Radiographs are the initial workup although anatomical differences and borderline measurements may lead to further cross-sectional imaging. CT scan is more sensitive in detecting subtle tibiofibular diastasis (Doughtie 1999). MRI is useful for the confirmation of the diagnosis as the syndesmotic complex is directly visualized (Fig. 6.7). A secondary sign frequently associated with syndesmotic injury is fluid extending greater than 12 mm into the tibiofibular recess on coronal sequences (Morris et al. 1996). At the professional level, MRI is increasingly used to confirm which structures are injured and evaluate for concomitant injuries (Sikka et al. 2012). Even though MRI provides this advanced level of detail, the exact role of MRI in prognosis and treatment management is still unclear (Jones and Amendola 2007).
Fig. 6.6
Normal anteroposterior (a) and mortise view (b) radiographs of the ankle demonstrate medial clear space (yellow arrow), tibiofibular overlap (red arrow), and tibiofibular clear space (black arrow)
Fig. 6.7
A 26-year-old football player with ankle injury. Coronal proton density-weighted MRI (a) of the ankle demonstrates increased signal in the distal interosseous membrane (arrow) representing a partial tear. Axial fat-suppressed T2-weighted MRI (b) demonstrates a high-grade partial tear of the AITFL which is thickened with intermediate signal at the fibular attachment (short arrow). PITFL demonstrates intrasubstance fluid signal near the fibular attachment (long arrow) representing partial tear
6.2.2.2 Grading
In athletes, syndesmotic ankle sprains are typically graded accorded to the West Point Ankle Grading System (Smith and Bach 2004). Grade 1 is no evidence of instability with minimal edema and tenderness. On MRI, grade I injuries are isolated to anterior inferior tibiofibular ligament (AITFL). Grade 2 is a decreased range of motion, moderate edema and tenderness, and possible instability. The difficulty in determining instability in grade 2 injuries has the potential to lead to underdiagnosis and inadequate treatment with devastating consequences. MRI grade II is injury to the AITFL and interosseous ligament. Grade 3 injuries demonstrate definite instability and significant edema and tenderness. MRI grade III is injury to the AITFL, interosseous, and posterior inferior tibiofibular ligaments. MRI grade IV is a grade III and injury to the deltoid ligament.
6.2.2.3 Treatment
The treatment goal is to restore anatomical alignment between the tibia and fibula to allow ligament healing. Compared to lateral ankle sprains, syndesmotic sprains can lead to persistent pain and disability with a significantly longer mean lost time from participation in the NFL at 15.4 days (Osbahr et al. 2013). A higher-grade injury on MRI has been correlated to a longer time on the disability list for players (Sikka et al. 2012). Unlike lateral ankle sprains, syndesmotic injury is not always treated conservatively. A majority of NFL syndesmotic injuries do not demonstrate diastasis, and a survey of NFL athletic trainers showed that most syndesmotic sprains are treated nonoperatively with immobilization, corticosteroid injection, rest, and ice being the most frequent treatments (Gerber et al. 1998). However, with frank diastasis, surgical correction is recommended; time away from play ranges from 9 to 16 weeks (Osbahr et al. 2013).
6.3 Knee
Knee injuries account for up to 36 % of all injuries with anterior cruciate ligament (ACL) tears being the most common (Saal 1991). Other structures which may be injured along with the ACL include the medial collateral ligament (MCL) and the menisci. Radiographs and clinical evaluation are the initial tests, although MRI plays a more crucial role in assisting in the diagnosis when compared to ankle sprains. In addition, these injuries usually need surgical correction and are season ending injuries.
6.3.1 Anterior Cruciate Ligament (ACL)
The ACL’s major role is to limit anterior translation of the tibia and secondary restraint to valgus/varus angulation when the knee is extended. Of note, given the increased awareness of head injuries with substantial penalties and fines for hits to the helmet, theories are arising that players are committing more low tackles resulting in an increase in ACL tears. However, a recent unofficial survey (Vrentas 2013) and a review of ACL tears showed that noncontact tears were more common than contact-related injury (Boden et al. 2000). Players’ strength and intensity during play are thought to contribute to these injuries. Planting the foot and cutting movements (decelerating prior to a change in direction) occur often, and this motion exerts a valgus load to a nearly fully extended knee with resulting overloading of the ACL (Olsen et al. 2004; Yu and Garrett 2007) (Fig. 6.8). Other proposed risk factors for noncontact ACL injuries include female gender, landing on the hindfoot, knee abduction, and hip flexion (Boden et al. 2009). Contact ACL tears in football are usually also a valgus injury and occur when a player takes a direct blow to the anterior thigh or lateral knee on a planted foot (Boden et al. 2000).
Fig. 6.8
Drawing illustrates valgus load applied to a nearly extended knee resulting in ACL tear and associated injury to the MCL. In football, contact and noncontact injuries lead to ACL injuries
6.3.1.1 Imaging and Diagnosis
ACL tears can typically be diagnosed by history and physical exam. The Lachman, anterior drawer, and pivot shift test are the most commonly performed maneuvers. The effectiveness of these exams depends on clinician experience and patient cooperation. Diagnostic difficulties arise with acute injuries because of the pain and swelling that can limit the clinic exam (Lubowitz et al. 2008). MRI is crucial in these cases for assisting in the diagnosis and demonstrates a high sensitivity and specificity (Lee et al. 1988), whereas radiographs have a limited role (Fig. 6.9). Also, associated injuries can be identified with MRI including MCL tears, meniscal tears, and osteochondral lesions (Remer et al. 1992) (Figs. 6.10, 6.11, and 6.12). At the professional level, MRI is generally performed for all knee injuries given the high accuracy and critical management decisions based on the findings.
Fig. 6.9
Sagittal proton density-weighted (a) and fat-suppressed proton density-weighted (b) and coronal fat-suppressed proton density-weighted (c) MRI of the knee demonstrate complete rupture of the ACL at the midportion (arrow). Injury occurred after a tackle to the outside of the knee on a planted foot which resulted in valgus stress
Fig. 6.10
Lateral knee radiograph (a) and sagittal fat-suppressed proton density-weighted (b) MRI of the knee demonstrate a deep lateral femoral sulcus sign. With an ACL tear, the tibia translates anteriorly impacting the lateral femoral condyle at the junction of the trochlea and anterior weight-bearing portion resulting in the indentation present on radiograph (arrow)
Fig. 6.11
Coronal fat-suppressed T2-weighted MRI (a) of the knee demonstrates a distal grade 3 MCL sprain. There is complete rupture of the distal attachment of the MCL with retraction (arrow) after a tackle to the lateral knee. Coronal fat-suppressed T2-weighted MRI (b) demonstrates a proximal grade 3 MCL sprain (arrow) with bone contusion in the lateral femoral condyle
Fig. 6.12
A 31-year-old football player with knee injury. Sagittal fat-suppressed proton density- (a, c) and proton density-weighted (b) MRI of the knee demonstrate acute chondral injuries. Fluid (arrow) interposed between the articular cartilage and subchondral bone represents full-thickness delamination (a). A full-thickness cartilage defect with subchondral bone marrow edema suggests acute injury (b, c)
6.3.1.2 Grading
Grading of ACL tears fall into two categories: complete and incomplete. Approximately 80 % of injuries are complete tears, and 20 % are incomplete tears that more commonly involve the anteromedial bundle of the ACL (Vahey et al. 1991). MRI is less accurate for identifying partial tears than complete ruptures. However, with higher-resolution imaging on 3 Tesla MRIs becoming more prevalent in routine imaging, the diagnostic capabilities are improving (Van Dyck et al. 2011). Increased signal within the ligament and ligament laxity are characteristic findings with partial tears (Umans et al. 1995).
6.3.1.3 Treatment
The treatment for ACL injuries in the general population is based on the patient’s activity level. For football players, conservative treatment is not a viable option if the goal is to return rapidly to the playing field. The ACL is a major stabilizer for the knee, and without surgical correction, a player would be unable to perform at the highest level and would risk further concomitant injury to the knee (Johnson et al. 1992). Recurrent bouts of instability may lead to damage of the cartilage and predispose the athlete to early osteoarthritis (Ratzl and Liang 2010). In the NFL, arthroscopic repair with patella tendon autograft is the preferred method (Bradley et al. 2002). An ACL tear is no longer a career-ending event, and a majority of NFL players return to the game after approximately a full year of rehabilitation. On the downside, studies have shown that player performance decreases after ACL repair when compared to their performance with their native ACL (Carey et al. 2006).
6.4 Pelvis/Groin
Groin injury is a general term encompassing a multitude of diagnoses and characterized by pain in the anterior pelvic and lower abdominal region. Common injuries included in this group include sports hernia, hip flexor strain, hip pointer, and labral injuries. These injuries are challenging to diagnose given the overlap in symptoms; imaging can provide a critical tool to decipher the etiology. Groin injuries are not uncommon in football, can lead to significant time on the injury list, and may need surgical treatment (Nam and Brody 2008).
6.4.1 Sports Hernia (Athletic Pubalgia)
When a player has a sports hernia, the media may use the words “abdominal strain” to describe the injury. “Sports hernia” is a misnomer because this injury is not a hernia by the traditional medical classification. Sports hernia (also known as athletic pubalgia) is a spectrum of musculotendinous strain involving the rectus abdominis, adductor longus, and pubis. The rectus abdominis and adductor longus share a common aponeurosis with the attachment on the pubis (Omar et al. 2008). Although the exact mechanical cause of injury is poorly understood, a leading theory is that an imbalance develops between the downward and lateral pull of the adductor muscles opposing the upward and oblique torque of the abdominal muscles (Fig. 6.13). In football, this may stem from cutting and explosive twisting movements where the hip is abducted and extended with rotation (hyperextension) at the waist. This disequilibrium results in tearing of the rectus abdominis, adductor longus aponeurosis, and reactive bone marrow edema in the pubis. An initial minor injury may result in instability at the pubis predisposing to further damage and instability with even minor activity (Omar et al. 2008). A majority of sports hernias are the result of repetitive trauma rather than acute injury (Preskitt 2011), and a common symptom is recurrent pain with activity that decreases at rest. The injuries can have a slow onset over weeks to months and recur with inadequate treatment.
Fig. 6.13
Drawing illustrates the leading theory on the mechanism of injury, which is that an imbalance develops between the downward and lateral pull of the adductor muscles opposing the upward and oblique torque of the abdominal muscles
6.4.1.1 Imaging and Diagnosis
The insidious onset of a sports hernia may delay the diagnosis for weeks to months. When an elite athlete develops groin pain, other etiologies must be excluded: hip/lumbar, genitourinary, intra-abdominal, and other muscle strains. On physical exam, tenderness over the pubis or the medial inguinal ring is a specific sign for a sports hernia. Pain at the inguinal floor with resisted hip adduction or resisted sit-up has also been shown to be reliable (Preskitt 2011). Initial workup usually includes radiographs to exclude a fracture. Advancements in knowledge of pelvic anatomy have transferred to MRI imaging. Dedicated protocols have been developed to evaluate this complex pelvic anatomy and allow for the detection of subtle injuries. Small field-of-view sequences evaluate the pubis, and large field of view allows survey of the entire hip/ pelvic region. Conventional orthogonal planes are usually adequate to make an accurate diagnosis, although an axial oblique sequence through the pubis may help increase certainty (Omar et al. 2008)(Figs. 6.14, 6.15, and 6.16).
Fig. 6.14
Axial oblique fat-suppressed T2-weighted MRI of the pelvis demonstrates bone marrow edema, asymmetrically worse in the left pubis (arrow). The image was obtained after the athlete returned to play from absence due to chronic, nagging groin discomfort, and the pain grew worse
Fig. 6.15
Axial fat-suppressed T2-weighted MRI of the pelvis demonstrate fluid undermining the rectus abdominis (a; arrow) and adductor longus (b; arrow), the aponeurotic attachment on the pubic symphysis representing tenoperiosteal disruption. Arrowheads demonstrate normal attachments
Fig. 6.16
Axial fat-suppressed T2-weighted MRI demonstrates high-grade disruption of the adductor longus attachment on the pubic symphysis (a; arrow). Sagittal fat-suppressed T2-weighted MRI demonstrates a tear extending cranially with fluid signal undermining the entire rectus abdominis-adductor longus aponeurosis (b; arrow)
6.4.1.2 Grading
A tenderness grading system has been used for the level of pain at the inguinal floor. The scale ranges from 0 to 5 with 0 being no tenderness and 5 being pain so severe that palpation is intolerable (Preskitt 2011). In general, a score <3/5 may be successful with conservative therapy. However, with improvements in imaging and the high-performance level of players, conservative measures are usually temporary solutions (Omar et al. 2008).
6.4.1.3 Treatment
The treatment for an injury to the rectus abdominis-adductor longus aponeurosis in an elite athlete is generally surgery. However, if the injury occurs during the season, local anesthetic and steroid may be injected at the pubic symphysis and adductor tendons along with 4–6 weeks of conservative management in an attempt to finish out the season with the expectation of off-season surgery. For lower level athletes, RICE along with core strengthening is considered first-line treatment with surgery reserved for injury recurrence or the inability to return to play after appropriate conservative management (Gerhardt 2006). Various surgical approaches have been undertaken to address and correct the presumptive root cause including herniorrhaphy and adductor tenotomy, with mixed results.
6.4.2 Hip Pointer
Hip pointer is a general term used to describe a variety of injuries to the anterior iliac crest, greater trochanter, and surrounding soft tissues. Confusion arises because in the strictest sense, “hip pointer” injury only includes a contusion to the iliac crest (Blazina 1967) as opposed to a broader use of the term referring to osseous and soft tissue injuries encompassing the entire region of the iliac crest. These injuries are most frequent in contact sports because of the direct hits to the pelvis (Hall and Anderson 2013). Also, players frequently fall to the ground landing on the anterior pelvis resulting in injury. While players wear padding to protect themselves, the degree of padding over the anterior iliac crest is usually minimal to limit the amount of restriction to a player’s range of motion and quickness. The result is relatively superficial bone and soft tissue that can readily be injured. Bone contusion and hematoma at the anterior iliac crest are the “classic” hip pointer injury, although fractures and tendon avulsions around the iliac crest and iliac spines are of utmost concern and the main reason for obtaining radiologic imaging (Figs. 6.17, 6.18, and 6.19). Muscle attachments on the pelvis that are frequently injured include internal/external obliques, transverse abdominis, gluteus medius, sartorius, rectus femoris, and tensor fascia lata.
Fig. 6.17
Anteroposterior pelvic radiograph (a) and coronal fat-suppressed T2-weighted MRI (b) of the pelvis demonstrate avulsion of the anterior inferior iliac spine (AIIS- arrow). The rectus femoris attaches at the AIIS. Avulsion occurs with eccentric muscle contraction as the hip extends with a flexed knee. Treatment is typically conservative management (Yildiz et al. 2003)
Fig. 6.18
Coronal (a) and axial (b) fat-suppressed T2-weighted MRI of the pelvis demonstrate complete rupture of the tensor fascia lata (arrow). This muscle attaches to the anterior iliac crest and assists in hip flexion and abduction. In addition, the tensor fascia lata contributes to pelvic stabilization when the hip is extended (Gottschalk et al. 1989). Complete rupture usually is the result of repetitive strains and can present with pain and hematoma formation in a distribution similar to a hip pointer injury
Fig. 6.19
Anteroposterior (a) and oblique (b) radiographs of the pelvis demonstrate a posterior acetabular fracture with fracture line extending near the sacroiliac joint (arrow). This fracture is often associated with posterior hip dislocations which occur most frequently in collision sports (Pallia et al. 2002). This injury requires significant impact and occurs when a player is tackled from behind and lands on a flexed knee with the hip flexed, adducted, and internally rotated. The additional force of an opposing player landing on the tackled player’s back drives the pelvis to the ground with the femoral head displacing posteriorly
6.4.2.1 Imaging and Diagnosis
The diagnosis of a hip pointer injury is usually readily apparent with the player’s history including the mechanism of injury and location of pain. After sustaining a traumatic event to the iliac crest, there is usually immediate pain in the area, although the development of pain may be delayed 24–48 h (Martinez 2014). Pain is usually exacerbated by activity and may limit range of motion at the hip. Physical exam may demonstrate obvious bruising and hematoma formation. Strength of the hip flexors, extensors, abductors, and external rotators should be intact, but pain may limit evaluation. Radiographs are obtained to evaluate for concurrent fracture or osseous avulsion. If solid organ injury is suspected, CT scan should be obtained, and evaluation for deep hematoma can also be performed (Martinez 2014). MRI is useful for muscle injury, hematoma formation, bone contusions, and tendons avulsions which assist in determining appropriate treatment and estimating time away from play.
6.4.2.2 Grading
There is no specific grading system for hip pointer injury. Correctly identifying this injury, preventing hematoma formation, and excluding more serious injuries are the primary concerns for appropriate management. While history and physical may be adequate to make a diagnosis, pain may limit evaluation, and advanced imaging is frequently relied upon especially in elite athletes.
6.4.2.3 Treatment
Treatment for hip pointer injury is RICE with early compression being critical to limit the degree of hematoma formation which can be subcutaneous, intramuscular, or subperiosteal (Hall and Anderson 2013). Also, high-impact contusions should be monitored closely for the development of compartment syndrome which is an infrequent occurrence but would require emergent fasciotomy. Initially, crutches are used to assist with ambulation, and subsequent activity is performed as tolerated. Complications arise if there is hematoma formation which may result in nerve compression (typically femoral and lateral femoral cutaneous nerves), fracture, or tendon avulsion (Martinez 2014). Orthopedic consult is warranted in these instances for appropriate management. Hematoma aspiration is indicated if there is compression on adjacent nerves and possible prevention of myositis ossificans; it may provide pain relief. Injection of local anesthetic and steroid has been shown to provide short-term pain relief allowing a player to return to the field sooner with less restriction in their play (Hall and Anderson 2013). When a player returns to the field, additional padding may be used in the area of prior injury to allow for an earlier return and to reduce the risk of re-injury. While return to play depends on the exact musculoskeletal injury and the player’s response to treatment, the average time away from play is 1–3 weeks. A study of NFL injuries showed that hip pointer injuries compromised 11 % of total injuries with mean time lost was 5.6 days (Feeley et al. 2008).
6.5 Shoulder
Shoulder injuries comprise a large proportion of upper extremity injuries, although they are less common than lower extremity injuries in football. Among shoulder injuries, acromioclavicular (AC) injuries make up a disproportionate share of the number of injuries [29.2 % of all shoulder injuries (Lynch et al. 2013)]. One noticeable difference in shoulder injuries is that most are caused by direct contact (Kelly et al. 2004), either with the ground or another player, whereas lower extremity injuries are often noncontact.
6.5.1 Acromioclavicular Joint
Acromioclavicular joint separation, referred to as a shoulder separation, occurs frequently in football. Quarterbacks have been shown to have the highest incidence rate of these injuries which usually occur during passing plays of a game (Kelly et al. 2004). The intense collisions either with another player or the ground result in a majority of these injuries. When a player falls to the ground with arm adducted or is contacted on the point of the shoulder, the shoulder girdle and scapula are driven downward, while the clavicle maintains anatomical positioning by restraint at the sternoclavicular joint (Fig. 6.20). The result is either ligamentous injury or clavicular fracture (Beim 2000). The supporting ligaments at the AC joint are the acromioclavicular and coracoclavicular. The acromioclavicular ligament is comprised of four areas of capsular thickening at the AC joint and maintains anterior-posterior stability. The coracoclavicular ligament is actually two ligaments (conoid and trapezoid) and prevents superior-inferior instability (Beim 2000).
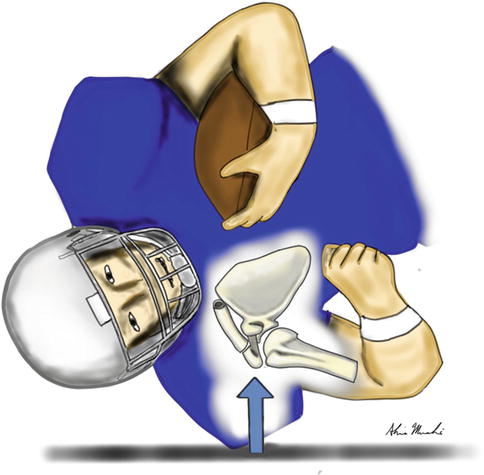
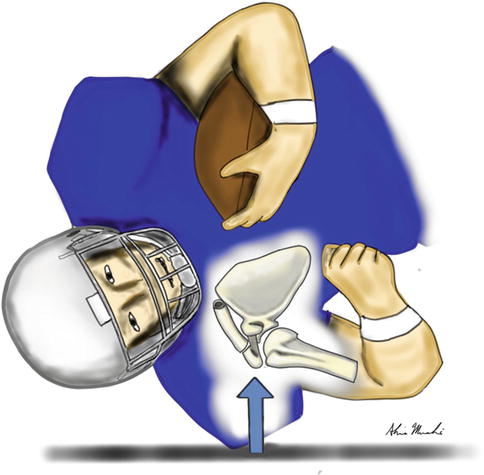
Fig. 6.20




Drawing illustrates a player falling to the ground with arm adducted landing on the point of the shoulder. The shoulder girdle and scapula are driven downward, while the clavicle maintains anatomical positioning by restraint at the sternoclavicular joint. The result is either ligamentous injury or clavicular fracture (Beim 2000)
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree